
Weekly News Recap
- Allscripts announces mixed Q2 results, which include a $145 million charge toward settling any liability that results from the Department of Justice’s Meaningful Use investigation against its acquired Practice Fusion.
- CVS beats Wall Street’s quarterly expectations and announces plans to expand its HealthHubs concept and to implement “next best action” programs for chronic care management.
- England’s NHS announces plans to form an $300 million artificial intelligence lab.
- Truman Medical Center pays ransomware hackers to regain access to its systems.
- Duke Clinical Research Institute and Cerner announce a pilot project to study patient data from non-Duke sites as the initial step in forming Cerner’s Learning Health Network.
- The DefCon cybersecurity conference creates a mocked-up hospital full of medical devices for hackers to play with.
- A new funding round values London-based AI health services vendor Babylon Health at over $2 billion.
- Guidehouse will acquire Navigant for $1.1 billion.
- Beaumont Health responds to reports of IT-heavy layoffs and the recent departure of its CIO and CMIO.
Best Reader Comments
Are you getting your license in other states for telemedicine purposes?? It always interests me how you have to have to be credentialed in the state of the patient even though you are providing the service from a different state, right?. Then I think of weird examples, like if you are on the phone with a patient who is riding in a car and they drive across state lines. One second you are having a legal conversation with a person and the next second you might be breaking the law! (Creds)
Even the most tech-awarded CHIME and HIMSS hospital systems are relying on their insurance to protect the corporation (not patients’ privacy) from hackers, Shamefully, most hospital CIOs have maintained very small budgets for cyber protection solutions and put basic security on auto pilot. [Ransomware victim] Truman Medical Center is “Most Wired” since 2010, Stage 7 HIMSS Analytics since 2013, a 2015 Davies Enterprise winner, and a Cerner model show site in its home town. (Are CIOS Ignoring or Ignorant?)
We need a law that says that they can’t play around with “re-identifiable data.” At this point we’re all aware that de-identified really means “not immediately identified”, or “you have to put in some work to make identifiable again.” De-identified should become un-identifiable. Of course in order to do that, you’ll probably be destroying whatever value they’re getting out of it. But they shouldn’t get to call it de-identified, it’s still PHI/PII unless mathematically provable that you can’t use that data to get to the identity of the people. (AC)
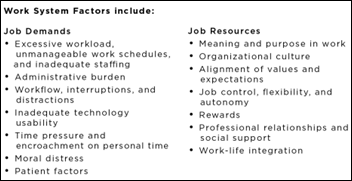
Why is Eric Topol not brave enough to say it? If you are in hospital administration, the group that collectively lobbies for you is called the AHA. If you are a small business owner – physician, the group that collectively lobbies for you is the AMA. If you are an employee of either of those two, the group that collectively lobbies for you is called a union. Ask a nurse to explain it to you. (SelfInflictedWound)
Meditech’s sales revenue is declining again. The company’s progress seems to be one step forward, two steps back. Saying the company is profitable and the balance sheet looks good, as was heard at the shareholder’s meeting, is another way of saying they are surviving. Meditech has yet to explain to its shareholders why it suffered such a large contraction during the period of greatest expansion the market has ever experienced, placing it a very distant third behind Cerner and Epic. (Running on MT)
I’ve talked to 5+ doctors about the thought process that they use to diagnose patients. I would characterize it as being a “satisficing” approach and I don’t think that computers are going to help make it better. I’m curious, though, about the percentage of diagnoses people think are incorrect. It really depends on how you define a misdiagnosis. 10% seems reasonable. (IANAL)
What’s [tackling problems with more impact than misdiagnosis] worth in real dollars that real physicians or medical organizations are going to spend? Unless I can convince enough physicians to pay for that service, what good does that do? I have to pay for my rent and groceries, too. We can have as many clever ideas for improving outcomes and patient health as we like, but we can’t do it for free. (HIT Girl)
Watercooler Talk Tidbits
A doctor from University of Calgary’s medical school mines Alberta’s EHR to find 60 ED visits that contain the word “scooter” to determine the extend of e-scooter injuries, although he admits that word usage might compromise accuracy. He urges those using the scooters to wear a helmet, which few riders of the newly introduced rental e-scooters do. The city requires helmets for bicyclists but not scooter-riders and allows only scooters to be ridden on sidewalks.
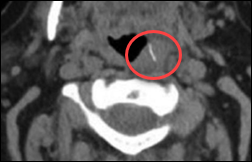
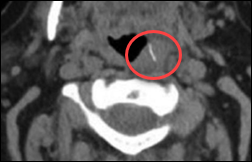
Doctors eventually find that a Michigan woman who had choked on the first bite of a grilled hot dog and then experienced repeated problems afterward with breathing, talking, and swallowing had a wire embedded in her throat, which turned out to be a bristle from a grill brush. Doctors removed it and she’s fine. She urges people to use plastic grill cleaning brushes, explaining that her husband later passed a magnet over the grill and picked up 30-40 more bristles.
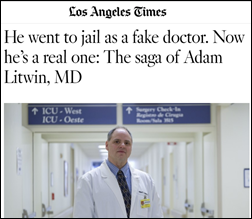
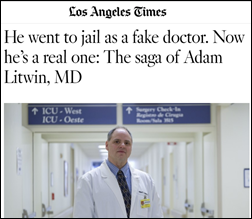
A man who was sentenced 20 years ago to jail and six months of psychiatric counseling for impersonating a doctor over a six-month period at UCLA Medical Center graduates from a Caribbean medical school at 47, admitting that it’s tough to get licensed and accepted into a US residency when his past includes forging prescriptions. His education probably isn’t helping his quest – a current student of the for-profit Saint James Medical School says the school has a minimum GPA of 2.0, an MCAT-optional admissions process, an attrition rate of 86%, an 8% first-pass NBME pass rate, and a low residency match rate.
Physician assistant Johnny Presley buys the recently closed Cumberland River Hospital (TN), pledging to open his fourth outpatient clinic there within four weeks and then possibly eventually adding a standalone ED. He paid $200,000 for the hospital, which had been bought for $6 million by a local hospital in 2012 that closed it after ongoing financial losses. He explains, “I might not be hardly as smart as some people or have as much money as some people, but I’ll outwork anybody. I just apply a lot of commonsense approaches. It’s a one-man show … I spent my life working in rural hospitals and rural communities and it’s a needed service in these areas. Unfortunately, it’s like time left those places, and it’s very sad. Growing up and working in them, seeing them all start to close is very sad.”

The for-profit hospital operator that bought two Wheeling, WV-area hospitals two years ago announces plans to close them both. One started as a city hospital in 1890, while the other opened its doors in 1906.

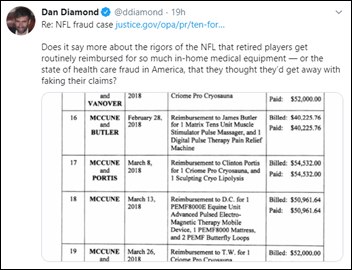
A jailed, 77-year-old pain management doctor in Detroit who is accused by the federal government of bilking insurers out of $500 million in a scheme involving opioid prescribing and spinal injections offers to turn his lakefront estate into a privately guarded prison if authorities will release him. Raj Bothra, MD’s most prolific prescriber, Eric Backos, MD – who “specializes” in “pain management, medication management, opioid detoxification, EMG/NCS testing to identify specific location of nerve injury, Botox therapy, and acupuncture” – prescribed 5.9 million pills from 2013 to 2018, with 86% of them being opioids and with at least two patients dying of overdoses following their visit.
In Case You Missed It
Get Involved


















































In fairness to the person on the thread the other day: Now THIS is politics on the blog. :)