Agfa HealthCare

Booth 2225
Contact: Kara Clarke, director of marketing, North America
kara.clarke@agfa.com
At HIMSS26, Agfa HealthCare will showcase its vision for “One Platform” Enterprise Imaging, a cloud-ready, SaaS-enabled approach designed to simplify complex imaging ecosystems; strengthen interoperability; and support secure, resilient clinical and IT workflows. What’s new includes continued advancements in its unified Enterprise Imaging platform; zero-footprint streaming technology for fast, full-fidelity image access anywhere care is delivered; and RUBEE Workflow Orchestration with embedded, vendor-neutral AI capabilities that streamline enterprise worklists and enhance diagnostic confidence without adding workflow friction.
Visitors to the booth can participate in personalized, one-on-one product demonstrations to explore real-world use cases and modernization strategies. Visitors are invited to connect with the team on Wednesday, March 11, during a Belgian Beer Tasting event. The speaker lineup will also feature a Main Stage session, “Defining Your Cloud Enterprise Imaging Strategy,” with Tampa General Hospital Senior Director of IT Steve Johnson and Agfa HealthCare Director of Enterprise Imaging Strategy Charles Morris, who will offer practical insights into cloud transition and enterprise-wide imaging transformation.
AGS Health

Contact Matt Bridge to arrange a meeting.
Contact: Matt Bridge, SVP of strategic solutions
matthew.bridge@agshealth.com
AGS Health is more than a revenue cycle management company — we’re a strategic partner for growth. Our distinctive methodology blends award-winning services with intelligent automation and high-touch customer support to deliver peak, end-to-end revenue cycle performance and an empowering patient financial experience.
We employ a team of 15,000 highly trained and college-educated RCM experts supporting customers across diverse care settings and specialties, including nearly half of the 20 most prominent US hospitals and 40% of the nation’s 10 largest health systems. Our thoughtfully crafted RCM solutions deliver measurable revenue growth and retention, enabling customers to achieve the revenue to realize their vision.
Altera Digital Health

Booth 4431
Contact: Lindsey Honig, marketing communications manager
lindsey.honig@alterahealth.com
A global healthcare IT leader, Altera Digital Health develops and elevates technology that brings next-level healthcare within reach. At HIMSS26, we’re excited to showcase how our AI and EHR advancements help healthcare organizations navigate their top challenges while supporting the human moments that matter most for patients, providers, and their communities.
Visit booth 4431 as EVP of AI Ben Scharfe provides crucial guidance on maximizing AI’s value while managing new liabilities in his educational theater session, “AI Unbound: Agentic workflows and deregulated risk,” on Wednesday, March 11, from 1:00–1:10pm.
Join our in-booth happy hour on Tuesday, March 10, from 4:30–5:30pm to meet Altera solution and subject matter experts while enjoying complimentary beverages and light fare. For our full theater schedule and to learn more about Altera’s presence at the event, visit our events page.
Arcadia

Booth 2447
Arcadia Customer AMAs
Stop by our booth for live “Ask Me Anything” sessions with Arcadia customers and hear directly from the people using our solutions every day. Ask your questions, learn from real-world experiences, and get an honest take on what it’s like to work with Arcadia – from peers who’ve been there.
Sips and Socks
It’s back! Don’t miss one of the most anticipated moments of the conference – our annual Arcadia HIMSS sock reveal. Stop by the booth to grab a drink and score a pair of our 2026 socks. Arrive early – these fan favorites are first-come, first-served, and they will go fast!
Speaker Sessions
Tuesday, March 10, 4:00-5:30pm
Wednesday, March 11, 4:00-5:30pm
“Improving Medicaid Outcomes with Digital Equity and Nutrition Support,” Tuesday, March 10, from 11:00-11:30am, Level 3, Murano 3304
“Artificial Intelligence in Action: Clinical Process Maps Get Modern,” Tuesday, March 10, from 11:00 – 11:30am, Level 5, Palazzo D
Visit our HIMSS page to learn more.
Artera

Booth 6421
Contact: Adrianna Hosford, chief communications officer and head of marketing
Adrianna.Hosford@artera.io
833.234.9355
Artera is the proven agentic healthcare company, leveraging a decade of deep expertise to support 2 billion patient communications annually. Our solutions empower humans and AI agents to work together to fix patient communications across text, phone, and web, unifying the entire patient journey – from scheduling and intake to billing and more. Trusted by over 1,000 healthcare organizations (including specialty groups, FQHCs, large IDNs, and federal agencies), Artera directly increases staff efficiency, boosts patient engagement, and improves the provider bottom line, helping patients get the care they need with simplicity and speed.
2B+ Annual Comms. | 200M+ Patients | 10yrs Experience | FedRAMP High in Process | www.artera.io
Join us at HIMSS to experience our fully autonomous AI agents in action – we’ll demonstrate how these agents manage a range of complex workflows (scheduling, FAQ resolution, appointment management, and more) to reduce staff burden and improve the patient experience.
Stop by our booth to connect with our experts and explore strategies for optimizing patient access, implementing AI-driven patient communication and much more. Plus, when you schedule and attend a meeting with an Artera team member, you’ll receive a $25 Amazon gift card. As an added bonus, you’ll be entered to win an iPad Pro in our post-event raffle. Schedule a meeting with our team at booth 6421 here.
Cardamom

Contact Adam Dial to arrange a meeting.
Contact: Adam Dial, chief customer officer
adam@cardamom.health
608.469.6154
The Cardamom team is excited to attend HIMSS! Reach out to connect with us during the event. Cardamom is a minority-owned, technology-forward health IT professional services company serving healthcare providers, payers, and health IT organizations. With a team-based, AI- and automation-first approach focused on committed outcomes, Cardamom helps customers more effectively use data, analytics, AI, and applications to improve care quality, reduce costs, and enhance patient and provider experiences. Cardamom is also committed to growing industry talent by hiring high-potential team members without prior health IT experience and providing comprehensive training and mentorship to deliver industry-leading results. For more about Cardamom, visit https://cardamom.health.
CereCore

Booth 6126
Contact: Phil Sobol, chief customer officer
Phil.Sobol@CereCore.net
855.276.9112
CereCore works behind the scenes to empower hospitals and health systems with IT services. Need to drive operational efficiency, improve financial outcomes, and uncover more bandwidth for your IT team? Our experts understand the major EHR platforms inside and out. Tap into support desk solutions that will result in happier users and providers.
For the second year, we earned a top KLAS Research rating in managed IT services, and we were the only vendor whose clients responded “Yes” 100% of the time when asked if their managed IT services provider exceeded expectations.
Facing an EHR transition that requires additional expertise? CereCore partners with healthcare organizations across the US and globe to provide comprehensive EHR consulting, IT and application support, technical professional and managed services, strategic IT consulting, and advisory services. Our hospital operations experience means we can help you create customizable roadmaps for RCM optimization, overcome talent shortages, and maximize your HIT investment.
Get a healthcare IT assessment and benefit from an outsider’s perspective, because the cost of not knowing often far exceeds the investment in finding out. Connect with us at HIMSS and find meaningful change with CereCore’s healthcare IT managed services.
Clearsense

Booth 1058
Contact: Kara Freeman, senior director of revenue operations
kfreeman@clearsense.com
612.747.2134
Stop Legacy Bloat: Clearsense Delivers the Blueprint for Cost Optimization at HIMSS26
Gartner reports that cost optimization is now the top priority for health system CIOs. Yet, while application rationalization is a powerful driver of savings, it remains healthcare’s most underutilized strategy. At HIMSS26, Clearsense will demonstrate how health systems are transforming legacy application decommissioning into a disciplined, repeatable engine for sustained cost reduction and operational modernization.
Visit booth 1058 to see how Clearsense helps health IT leaders move beyond simple archiving to build a governed, trusted data foundation that:
- Delivers recurring cost takeout: Eliminate ongoing maintenance, infrastructure, and TSA expenses through structured application rationalization and active archiving programs that generate sustained operating expense savings.
- Strengthens security and compliance: Reduce legacy application risk by retiring redundant and unsupported systems while preserving secure, audit-ready access to retained clinical and operational data.
- Creates an AI-ready core: Consolidate fragmented historical data into a centralized, governed archive – establishing a reliable foundation for advanced analytics and scalable AI initiatives.
In addition, Clearsense will officially unveil its AI strategy at HIMSS26, integrating intelligence across the platform to drive faster operational execution while delivering a more intuitive, insight-driven experience at the point of care.
Schedule a meeting with the Clearsense team by clicking here!
Clearwater

Booth 10001-07 in the Cybersecurity Command Center
Contact: John Howlett, SVP and chief marketing officer
773.636.6449
You’ll find Clearwater exhibiting in the Cybersecurity Command Center at booth 10001-07, where our team will be showcasing how healthcare organizations can proactively manage cyber risk, protect patient data, and strengthen compliance across increasingly complex digital ecosystems. Stop by to learn how Clearwater helps healthcare leaders:
- Reduce cyber risk across clinical, operational, and third-party environments.
- Navigate evolving regulatory and compliance requirements.
- Build resilient, security-first digital health programs.
Also, be sure to catch our session “Healthcare AI Governance & Risk Management: Securing Innovation Without Slowing Care” in the Cybersecurity Command Center on Wednesday, March 11, from 10:00-10:20am. Clearwater VP of Consulting Solutions & Strategy Dave Bailey will be joined by Onvida Health CISO Blaine Hebert for a discussion of how to harness AI innovation while managing new and evolving risks.
Clinical Architecture

Booth 5753
Contact: Jaime Lira, VP of marketing
jaime_lira@clinicalarchitecture.com
317.580.8400
Clinical Architecture delivers scalable data quality and transformation solutions that help healthcare organizations turn complex, inconsistent data into trusted, actionable information. Our solutions support providers, payers, life sciences companies, and public agencies with tools to standardize data, assess quality, and enable reliable exchange.
With the PIQXL Gateway, our implementation of the emerging Patient Information Quality Improvement (PIQI) framework, we provide a score-based, real-time view into patient data quality, pinpointing gaps like missing, invalid, or non standard elements so you can remediate quickly. By improving data integrity and compliance, we empower organizations to power analytics, strengthen decision-making, and advance value-based care with confidence.
Be sure to attend “Enhancing Healthcare Data Quality: Digital Measurement Standards and the PIQI Approach” on Monday, March 9, from 11:20am-12:00pm, Level 5, Palazzo L. Our CEO, Charlie Harp, will be presenting on a panel with NCQA CTO Edward Yurcisin and Levitt Partners Principal Ryan Howells.
Visit us at booth 5753 for a live demo of the PIQXL Gateway and see how data quality can be objectively scored and improved using the PIQI framework. We look forward to seeing you in Vegas!
CloudWave

Booth 6235
Contact: Christine Mellyn, VP of marketing
cmellyn@gocloudwave.com
508.251.8899
Visit CloudWave, the healthcare data security experts, at booth 6235 for an interactive, informative experience! Our team of experts will be available to discuss important topics such as cybersecurity, cloud solutions, compliance, and more. In addition, we’re excited to offer a hands-on tabletop card game that immerses you in incident response and cybersecurity strategies. Using the Backdoors & Breaches deck of expertly designed cards, players will simulate real-world cyber incidents, sharpen response skills, and gain a deeper understanding of modern cyberattack techniques.
We’ve got a lot happening:
- Win a Prize! – Participate in raffles at the conclusion of each day. You don’t need to be present to win!
- Ask Questions, Get Answers – Visit our solution stations and speak with our experts about how CloudWave can help address your IT and cybersecurity challenges.
- Meet with Our Team – Request a personal meeting (customersfirst@gocloudwave.com) with us to discuss your unique needs.
- Tabletop Simulations – Join us for hands-on simulations and take home your own card deck, plus a bonus gift if you complete the game.
CognomIQ

Booth 11724
Contact: Bonny Roberts, VP of customer success
Bonny.Roberts@CognomIQ.com
614.565.7884
Healthcare Data Sucks. CognomIQ can UNsuck it. One end-to-end platform replacing more than two dozen SaaS tools like Snowflake, DataBricks, PowerBI, Tableau, ESRI, Datavant, TriNetX, and more. Save seven-figures per year immediately with a 15X speed increase or we’ll refund 100% after the first year. We’re that confident. Come by booth 11724 on the AI Trail and tell us to UnSuck it! We’ll brand you with swag.
Concord Technologies

Booth 1461
Contact: Liza Marie Hayward, marketing program manager
lhayward@concord.net
Concord is the market leader in Intelligent Data Exchange for the healthcare industry, securely processing over 4 billion pages of protected data every year. Our portfolio includes AI-powered fax and document workflows, Intelligent Document Processing, and Straight-Through Processing of patient data into the EHR. With 30 years of proven expertise, Concord empowers healthcare organizations to eliminate manual workflows, improve operational efficiency, and enhance the delivery of care.
We hope you’ll join us for some of our activities throughout HIMSS:
- Tuesday, March 10: Attend our Main Stage session, “Rethinking Interoperability: Is it time to trust LLMs over standards?” from 2:40–3:10pm.
- Wednesday, March 11: Concord-sponsored Happy Hour in booth 1461 from 3:00-5:00pm.
- All exhibition hall hours at booth 1461: Race to win in our Simulator Challenge. Put yourself in the driver’s seat and take a few laps around the track in our in-booth race simulator. Take your place on our leaderboard after you pass the checkered flag!
CTG Health Solutions

Booth 3516, Venetian Level 2
Contact: Sarah Blafer, marketing team lead, demand generation
Sarah.Blafer@ctg.com
860.942.2180
CTG, a Cegeka company, delivers IT and business solutions that enhance digital agility. With 55+ years of experience – and 35+ years in healthcare – we empower healthcare organizations to modernize systems, improve performance, and advance digital initiatives through innovative services and modern technologies. We’ve supported 1,000+ healthcare organizations, including children’s hospitals, health systems, and academic medical centers. Our expertise spans EHR implementation and managed services, cybersecurity, ERP, cloud, infrastructure, IT/application support, and clinical optimization. Combining local market knowledge with 10,000+ Cegeka Group professionals in 15+ countries, we serve healthcare and other high-growth industries. For more information, visit us at booth 3516.
DrFirst

Booth 3243
Contact: Erin Hall, director, event strategy and experience
eleasehall@drfirst.com
216.650.7687
Meet with DrFirst at HIMSS! Behind every prescription is a tangle of benefit checks, prior authorizations, and pharmacy back-and-forth. Meet with us at HIMSS to see how DrFirst cuts through the complexity within the prescribing workflow before problems start.
Prior authorizations are resolved right away, not days or weeks later. Coverage and cost are visible at the point of prescribing. Prescriptions arrive at the pharmacy ready to fill. Automated text messages keep patients engaged and on therapy. The result: Fewer abandoned prescriptions, better patient outcomes, and less administrative burden.
To learn more, don’t miss the session featuring Magnolia Regional Health’s Ben Long, MD showing how SMS text notifications reduced odds of CHF readmissions by 6% on March 12 at 8:30am in Palazzo D, Level 5.
Let’s chat in Las Vegas!
About DrFirst
For 25 years, healthcare IT pioneer DrFirst has empowered providers and patients to achieve better health through intelligent medication management. The company has won over 25 awards for excellence and innovation, including Time’s list of the “World’s Top HealthTech Companies of 2025,” recognizing the company’s medication management solutions and integrated workflows that make every step of the patient journey easier, from first prescription to ongoing adherence. DrFirst solutions help 100 million patients a year and are used by more than 450,000 prescribers, 71,000 pharmacies, 270 EHRs, and over 2,000 hospitals in the US. To learn more, visit DrFirst.com.
Ellkay

Booth 5423
Ready to build the future of healthcare? Ellkay is a trusted enterprise data management partner, driving innovation and connectivity across the healthcare ecosystem.
Join us at HIMSS26! We will have daily coffee bars and Happy Hours on Tuesday and Wednesday at booth 5423. Come get a drink and discuss how your organization can transform care delivery through true interoperability and data management solutions.
FDB

Booth 3235
Contact: Sammy Keating, product marketing manager
Sammy.Keating@fdbhealth.com
802.343.2619
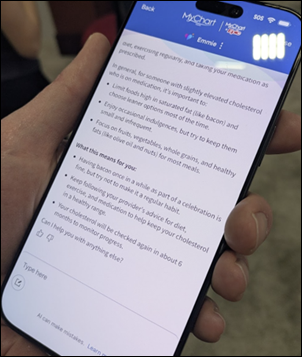
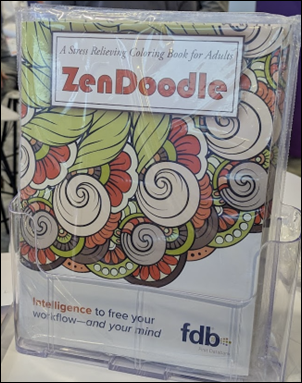
At FDB (First Databank), we’re proud to be the leading provider of drug knowledge that helps healthcare professionals make precise, confident medication decisions. At HIMSS26, we’re bringing our theme, “Intelligence to Free Your Mind,” to life – showcasing how our medication intelligence, built on decades of trusted drug knowledge and delivered in patient-specific clinical context, helps reduce cognitive burden, restore focus, and strengthen both human and AI-enabled workflows.
As healthcare organizations look for safe, scalable ways to adopt AI and automation, we’re excited to introduce new innovations at booth 3235. We’ll be featuring FDB MedProof MCP, our AI-native server that standardizes governance and access to medication intelligence across AI-enabled systems. We’ll also highlight workflow advancements like FDB Script Agent, an AI-enabled prescription automation agent designed for ambulatory settings, and FDB VerifyAssist, an inpatient pharmacy order verification assistant designed to help hospital pharmacists quickly spot orders that need closer review.
Attendees can also explore how our trusted solutions – FDB MedKnowledge, FDB Targeted Medication Warnings, FDB AlertSpace 2.0, Pharmacogenomics CDS, and FDB Meducation – support health systems in improving medication safety, reducing non-actionable alerts, and delivering truly patient-specific decision support and education. We’ll also be showcasing FDB Vela, our modern e-prescribing network built to power resilient, connected medication workflows.
While you’re at our booth, join one of our daily micro-sessions covering topics like agentic workflows, medication reconciliation, and pharmacy order verification. And of course, we’re creating space to recharge and connect. We’ll be hosting “Calm Continues at Happy Hour” on Wednesday, March 11, from 4:00 to 5:30pm at our booth, with beer, wine, soft drinks, and light bites. Throughout the conference, stop by for complimentary chair massages, infused water, themed giveaways, and a chance to win a Theragun Mini (3rd Gen) portable massage device. We’re looking forward to connecting with you at HIMSS26!
Five9

Kiosk 3264-04
Contact: Roni Jamesmeyer, director of industry marketing
roni.jamesmeyer@five9.com
972.768.6554
Five9 helps healthcare organizations reimagine patient engagement by unifying every interaction – voice, digital, and automated – on a single intelligent platform. Our HIPAA-compliant cloud contact center integrates seamlessly with Epic, Cerner, and Salesforce, enabling real-time access to scheduling, patient data, and care workflows.
By combining advanced AI, automation, and workforce optimization, Five9 empowers patient access teams, care coordinators, and revenue cycle staff to reduce wait times, improve access to care, and deliver faster, more personalized experiences. The result is a smarter, more connected patient journey – from first contact through follow-up – driving higher satisfaction, lower operating costs, and better outcomes.
Five9 will be located in kiosk 3264-04 in the Patient Experience & Wellness section and in a large booth located at Enterprise Connect at the Caesars Forum. We will have a booth raffle on Wednesday for everyone! Five9 and Pindrop will host a dinner at Ruth’s Chris on March 10 – please ask for an invitation!
Fortified Health Security

Booth 11302
Contact: Rachel Bryant, marketing coordinator
rbryant@fortifiedhealthsecurity.com
904.316.3310
Join Fortified Health Security at HIMSS26 to explore the latest in digital health innovation, cybersecurity, and healthcare transformation. Fortified is built for healthcare, offering tailored solutions to help you address your unique challenges, navigate the ever-changing legislative landscape, and work alongside you to create a stronger cybersecurity posture.
Tee off HIMSS26 with us at Top Golf Las Vegas on March 8, or connect with our team at booth 11302 and enter our daily giveaway. Get all the details to secure your spot here. We look forward to seeing you in Las Vegas!
Health Data Movers

Booth 4935
Contact: Brooke Foster, marketing coordinator
brooke@healthdatamovers.com
847.404.0326
Health Data Movers is hosting our second annual Vivas Las Datas Happy Hour and Raising the Stakes for a Cause poker tournament! Hosted by Health Data Movers and CitiusTech, as well as the Kansas and Greater Kansas City HIMSS Chapters, the Vivas Las Datas Happy Hour brings together healthcare leaders for a relaxed opportunity to unwind, reconnect, and talk about what’s next in healthcare data. No sales pitches. No panels. Just great people, great drinks, and great conversation. Join us at Chica at The Venetian Las Vegas on March 10, from 5:00-7:00pm. Space is limited, so be sure to save your spot. RSVP here.
Raising the Stakes for a Cause will be a night of fun and friendly competition, all while supporting the Michael J Fox Foundation. Get ready to show off your poker skills and enjoy a great time with fellow attendees. Don’t miss out on this exciting event for a great cause! Join us in The Poker Room at The Venetian Las Vegas on March 10, from 8:00-11:00pm. Space is limited, so be sure to save your spot. RSVP here.
Lincata

Booth 1365
Contact: Adam DeRocher, chief revenue officer
adam.derocher@lincata.com
712.541.9132
Lincata’s Bedside Operating System (OS) transforms hospital televisions into digital experience tools that launch MyChart Bedside TV directly in-room. It’s simple. LincTV by Lincata, coupled with MyChart Bedside TV, existing TV screens, cameras, microphones, and other equipment helps health systems create the foundation for smart room capabilities and virtual care. LincTV consists of a proprietary set-top box and purpose-built MDM that provides flexibility, scalability, security, and ease of deployment. More than TV. Make it LincTV.
Med Tech Solutions

Booth 5448
Contact: Shana Tachikawa, director of marketing
stachikawa@medtechsolutions.com
Med Tech Solutions (MTS) is a managed services provider delivering comprehensive IT and EHR support to healthcare organizations nationwide. With a singular focus on healthcare technology, MTS empowers clients with IT and EHR managed services, cloud hosting, 24/7 help desk, and revenue cycle solutions, along with tailored software and security offerings. With Stoltenberg Consulting now part of the MTS family, MTS expands this reach with deep Epic, Oracle Cerner, NextGen, ECW, and Meditech consulting; staff augmentation; go-live support; and legacy system services. Together, MTS and its brands help healthcare providers optimize technology, streamline operations, and enhance patient care across full IT lifecycles.
Elicit greater value from your EHR investment. Ensure long-term success of your EHR program across organizational growth. Leverage skilled, flexible, EHR-certified resources to cost-effectively fill IT expertise gaps with:
- EHR Service Desk
- EHR-Certified Staffing
- Legacy EHR Managed Services
- EHR Data Archiving
- EHR Data Integration
- Go-Live Support
- M&A Systems Alignment
Backed by 3x Best in KLAS standing for Partial IT Outsourcing, maximize your EHR’s full potential. Schedule an executive meeting with Med Tech Solutions in booth 5448!
Medcurio

Booth 222
Contact: Joe Lovato, director of customer solutions
joe@medcurio.com
503.704.3920
Medcurio helps health systems access and act on their EHR data in real time, without waiting months for integrations or settling for partial interfaces. Its VennU platform installs inside the customer’s environment and gives teams direct, governed access to the data they already own. The result is faster insight, faster action, and fewer workarounds. VennU is used to power dashboards, alerts, automations, and any downstream workflows that depend on complete and timely EHR data. Customers decide what data is accessed, who can use it, and how it is applied, with full auditability and security controls. Nothing leaves the customer’s control.
Medcurio has been invited by InterSystems to showcase its technology live at their booth. We’re demonstrating how we’ve made it incredibly simple to get ANY data – in real time – out of the EHR. Not limited to: FHIR, HL7, latent or batch-based data. This is true real-time access without the traditional constraints.
We’ll be giving live demos of our cutting-edge platform. If your organization has ever struggled to extract real-time data from your EHR, stop by!
Medicomp Systems

Booth 5435
Contact: James Aita, director of strategy and business development
marketing@medicomp.com
703.803.8080
Medicomp delivers the industry’s only physician-curated universal data foundation, transforming healthcare data into trusted intelligence through Quippe, its evidence-based Clinical Intelligence Engine. Quippe connects information across domains, normalizes every input, and validates AI outputs to ensure accurate, interoperable insights at the point of care – fueling innovation, improving accuracy, and unlocking the full value of clinical data.
Medicomp will be showcasing entirely new functionality that streamlines clinical workflow, combining technologies like ambient listening, natural language processing (NLP), and Model Context Protocol (MCP); and leveraging its universal data foundation and knowledge graph to deliver the efficient, intelligent, clinical workspace that clinicians have been craving.
The gap between data and understanding is probably costing you – in denied claims, compliance penalties, technology ROI, clinician burnout, and patient safety risks. Stop by the Medicomp booth to learn how your systems can benefit from:
- Clinically-validated LLM outputs.
- Diagnostic intelligence that understands context, is evidence-based, and makes disparate data computable.
- Clinical-grade agents based on a universal data foundation.
Solve the data reliability problem with diagnostically intelligent clinical data solutions. To learn more, visit Medicomp.com.
Meditech

Booth 5031 and Interop+Smart Experience Pavilion booth 12623
Contact: Rachel Wilkes, AVP of marketing
rwilkes@meditech.com
781.774.4555
Join Meditech in booth 5031 to see firsthand how the intelligent Expanse platform is turning innovation into impact for health systems of all sizes – from small rural hospitals to large IDNs. Visitors will hear directly from clinicians and see demonstrations of the Expanse EHR platform in action. See how the Expanse platform strengthens patient engagement, leverages AI to unburden staff, and enables connected care across all healthcare settings.
Meditech will also host daily Lunch & Learn sessions in the booth. Attendees can enjoy a complimentary lunch while hearing from Meditech and customer experts on the following topics:
Monday, March 10
”The Intelligent Application of AI,” from 12:45-1:05 pm.
”Meditech Expanse: A Foundational Platform for Innovation,” from 1:30-1:50pm.
Tuesday, March 11
”Efficiency Unleashed: The Intelligent EHR in Practice,” from 12:15-12:35pm.
”Empowering Patients Beyond the Clinic,” from 1-1:20 pm.
Wednesday, March 12
”Intelligent Interoperability in Action,” from 12:15-12:35 pm.
”Create, Share, Grow with Greenfield,” from 1-1:20 pm.
Outside the booth, Meditech customers will present their latest innovations and real-world experiences, successes, and strategies in educational presentations covering a wide array of topics, including nurse retention strategies, data-driven approaches to rural population health, and more.
You can also visit Meditech in the Interop+ Smart Experience Pavilion at booth 12623 to see how the company’s intelligent interoperability solutions empower patients and their care teams with complete, unfettered access to health data. Experience three dynamic demonstrations running daily: The Connected Clinician, The Empowered Patient, and The Interoperable Enterprise. Each demonstration will follow the patient journey to illustrate how Meditech Expanse, alongside partner solutions, transforms interoperability into a true force multiplier for care.
Attendees can also hear directly from Meditech and healthcare leaders at the Interop+ Smart Theater:
- Tuesday, March 10: “Orchestrating the Payer-Provider Care Team for Rural Health Resilience,” from 11:45am–12:05pm.
- Wednesday, March 11: “From Conversation to Cash Flow: AI and the Future of Revenue Integrity,” from 10:15–10:35am.
- Thursday, March 12: “Powering Rural Health Through Open, Intelligent EHR Innovation,” from 10:15–10:35am.
See Meditech’s HIMSS event page for a full listing of sessions.
Nordic Global

Booth 631
Contact: Rebecca Whaley, head of marketing
Rebecca.Whaley@nordicglobal.com
Join Nordic, a global leader in healthcare transformation, at #HIMSS26 in booth 631 to explore the future of healthcare technology. Enjoy free, all‑day coffee at our booth and meet the Nordic team to discuss how we can support your workforce and operational priorities for 2026. We’ll also be unveiling our new look at our HIMSS brand launch party.
Highlights:
- Enjoy free, all‑day coffee and meet the Nordic team at booth 631.
- Join us at the Buzzed After Dark Networking Reception, sponsored by Nordic, on Sunday, March 9, from 9:00pm-12:00am.
- Donut panic. Fewer apps are possible. Grab a free donut and learn about application portfolio management with Nordic and our partner Clearsense on Monday, March 10, from 10:00–11:00am at booth 631.
- Connect with Nordic and Workday at the FQHC Happy Hour on March 10, from 5:00–6:00pm at the B Bar at the Wynn. (invite only)
- Join us as we officially launch Nordic’s new brand during Under the Nordic Star, a client and partner reception, sponsored by Clear and ServiceNow, on March 10, from 6:00–9:00pm. at La Cave Bar + Restaurant at the Wynn.
- Meet Nordic CMO Craig Joseph, MD, author of “Designing for Health,” to explore why human‑centered design matters in healthcare on Monday, March 10, from 1:00–2:00pm and Tuesday, March 11, from 10:00–11:00am at booth 631.
- Join Nordic for a networking happy hour during the HIMSS Chapter Social hosted by HIMSS Wisconsin on March 11, from 4:00-5:30pm at booth 631.
Visit our event page to see what Nordic is doing at HIMSS and book a meeting with our team!
Optimum Healthcare IT

Meeting Room MP11356
Contact: Larry Kaiser, chief marketing officer
lkaiser@optimumhit.com
Best in KLAS, Overall Implementation Firm, Optimum Healthcare IT will be at HIMSS. You bring your goals and outcomes, we will bring the strategy and team to make it happen. Optimum’s comprehensive service offerings include enterprise application services; digital transformation; and workforce management, which features our Optimum CareerPath skill development program. Backed by a leadership team with extensive expertise, we deliver tailored healthcare consulting solutions to diverse organizations.
HIMSS Highlights
Meeting Room MP11356
AWS Demos March 12
AWS Booth: UC Davis Health – Primary care scheduling reduces no-shows effectively. Patient verification streamlines appointments, enhances revenue.
Wrapt Health: Oncology scheduling with predictive rescheduling modeling. Reduces cancellations, minimizes medication waste costs.
Microsoft Demo March 10 at 10:00am, March 11 at 11:10am, and March 12 at 12:50pm.
Microsoft Booth: Deliver secure, high-performance clinical workspaces in AVD – anywhere.
Reception on March 11 at 6:00pm. Contact your Business Development Executive for more information.
PerfectServe

Booth 1665
Contact: Jenn Corcoran, senior marketing manager
jcorcoran@perfectserve.com
802.379.5352
Struggling with after-hours coverage, missed handoffs, or “Who’s on call?” confusion? At HIMSS, PerfectServe is offering complimentary 15-minute workflow reviews for healthcare leaders who want to identify gaps in their communication and scheduling processes – and leave with clear, practical next steps. During the 15-minute Workflow Review, we’ll:
- Walk through your current communication and scheduling workflow.
- Identify failure points that create delays, burnout, or risk.
- Highlight opportunities to simplify, automate, or integrate with your EHR.
- Share how peers are addressing similar challenges.
You’ll leave with:
- A clearer picture of where things break down.
- Practical ideas you can take back to your team.
- A benchmarked perspective from other health systems.
Who should book time:
- CMOs, CIOs, COOs
- Clinical operations leaders
- IT leaders responsible for clinical communication
- Physician and nursing leadership
- Scheduling managers
Why PerfectServe?
PerfectServe helps health systems accelerate speed to care by bringing communication and scheduling into a single, EHR-integrated platform. We help organizations:
- Create a single source of truth for staff scheduling.
- Enable secure, role-based care team communication.
- Power a reliable clinical contact center.
- Finally answer, with confidence, “Who’s on call right now?”
For more, visit our dedicated event page.
Praia Health

Contact Conrad Swanson to arrange a meeting.
Contact: Conrad Swanson, VP of sales
conrad@praiahealth.com
Praia Health is the patient experience orchestration platform for health systems. We help health systems attract, engage, and retain patients by supercharging their portals and digital tools with seamless, personalized journeys in one platform. The result is higher retention, lower costs, and measurable ROI.
Praia Health was named Best in Show at the HIMSS26 Emerge Pitch Competition, winning in the Health Systems: Address Hospital Capacity Crisis category. Praia Health CEO Justin Dearborn will be presenting during the HIMSS Emerge Innovation Pitch Competition: Best-in-Show Solutions for Hospital Systems Challenges on Wednesday, March 11, from 11:50am-12:35pm. Team members will also be available throughout the conference to share more about our patient experience orchestration platform.
RevSpring

Booth 1335
Contact: Andrea Zaczyk, VP of marketing
azaczyk@revspring.com
RevSpring helps healthcare organizations improve the financial experience for patients while strengthening revenue cycle outcomes. The platform combines billing, payments, analytics and patient engagement tools to simplify healthcare payments and make financial communications clearer. At HIMSS, attendees can visit the booth to see how RevSpring is modernizing the patient financial journey with smarter billing communications, digital payment options, and data-driven insights.
Rhapsody

Booth 4832
Contact: Michelle Blackmer, chief marketing officer
michelle.blackmer@rhapsody.health
404.974.5060
Simplify interoperability, accelerate EHR integration, and get your data foundation ready for what’s next. That’s what teams do with Rhapsody – purpose-built for healthcare and trusted by 1,900+ organizations worldwide. Best in KLAS for 17 years.
Stop by booth 4832 for live demos of Rhapsody Axon, the industry’s first healthcare integration agent embedded in Rhapsody and Corepoint Integration. See how AI-powered integration reduces friction, shortens build cycles, and moves from kickoff to go-live faster.
Connect with our experts to explore how you can:
- Integrate with EHRs across your ecosystem.
- Modernize legacy environments while supporting FHIR, APIs, and HL7.
- Strengthen person identity and terminology data foundations.
- Build an agent-ready interoperability layer.
Then, join us Tuesday, March 10, from 6:30-8:30pm at Brera Osteria (St. Mark’s Square at The Venetian Resort, Grand Canal Shoppes), to continue the conversation.
SlicedHealth

Contact Jason Whiteaker to arrange a meeting.
Contact: Jason Whiteaker, regional VP, channel partnerships
jason.whiteaker@slicedhealth.com
901.493.3110
SlicedHealth is a payer contract revenue intelligence platform designed to help hospitals, health systems, specialty practices, and surgery centers navigate payer complexity and secure the revenue they’ve rightfully earned. Through AI-driven contract modeling and real-time analytics, SlicedHealth identifies underpayments, denial patterns, and price transparency gaps while bringing clarity to complex payer agreements.
Our team will be onsite at HIMSS meeting with healthcare finance and revenue cycle leaders focused on reimbursement strategy and contract performance. To connect during the conference, please reach out directly to Jason Whiteaker (jason.whiteaker@slicedhealth.com) to coordinate a time to meet and discuss how revenue intelligence can drive measurable financial impact in 2026 and beyond.
Sonifi Health

Booth 2861
Contact: Jared Allen, SVP of sales
jallen@sonifihealth.com
801.386.1450
Sonifi Health provides industry-leading, interactive patient engagement technology proven to improve patient outcomes and staff productivity. The EHR-integrated platform is designed to anticipate the needs of patients and clinicians, infusing the principles of hospitality into care experiences. As part of Sonifi Solutions, Inc., the company supports more than 300 million end user experiences annually. Learn more at sonifihealth.com.
Surescripts

Booth 1139
Contact: Kate Giaquinto, PR manager
kate.giaquinto@surescripts.com
603.548.5273
Join Surescripts at the forefront of healthcare innovation and learn how we can inform and accelerate decisions to keep patient care on track.
Connect with us at HIMSS26 in booth 1139 to discover how we can partner to:
- Deliver clinically appropriate prior authorization decisions faster.
- Empower the healthcare ecosystem with intelligence and interoperability.
- Add real-time cost and care intelligence to existing workflows.
Tegria

Booth 4802
Contact: Berit Rhody, Manager, Events and Engagement
berit.rhody@tegria.com
Tegria is a global healthcare consulting and services company that partners with provider and payer organizations to transform healthcare. Tegria’s global team of more than 1,000 experienced professionals has helped drive meaningful change for more than 650 provider and payer clients across North America and Europe. Tegria has been ranked and recognized in consecutive Best in KLAS reports, including a #2 ranking in the “2026 Best in KLAS: Software & Services” report for Overall IT Services Firm and Best in KLAS recognition for Payer IT Consulting (2025) and Application Hosting (2024).
Join us for some engaging sessions while you are at HIMSS :
“Lunch & Learn: How Leading Health Systems are Closing the Access Execution Gap” on Tuesday, March 10, from 12:30-1:45pm on Venetian Level 1, Casanova 601. As patient access becomes a strategic driver of financial performance and growth, health systems must move beyond scheduling to optimize the entire patient journey. This session shares executive insights and real-world examples to help organizations strengthen foundational access metrics, align strategy with execution, and turn digital access into a sustainable enterprise advantage. Register here to reserve your spot.
“Don’t Gamble on ROI: Win Big with Change Management” on Wednesday, March 11, from 12:00-12:20pm in the Business Ops Pavilion, Level 2, Hall C, booth 4400. Healthcare organizations often struggle to achieve lasting value from technology investments because the challenge lies not in the systems, but in how change is managed. In this session, KLAS Research and Tegria will introduce a proven change management framework that helps leaders drive adoption, protect ROI, and sustain workforce and patient trust throughout transformation.
“Denied No More: A Revenue Recovery Playbook” on Wednesday, March 11, from 2:00-2:30pm on the Connect Theater Stage. This session explores how a data-driven approach can uncover hidden patterns behind costly bundled procedure denials, including specific service combinations and payer behaviors. Through a real-world case study, attendees will gain practical strategies to reduce denials, improve billing accuracy, and strengthen overall revenue cycle performance.
View full details for all of Tegria’s HIMSS26 sessions on our event page.
TruBridge

Demo station 23 in Microsoft booth 2812
Contact: Shane Smith, sales consultant
Shane.Smith@trubridge.com
502.671.9292
TruBridge empowers rural and community healthcare with tech‑enabled solutions designed for their realities. With 45+ years of experience and 1,500+ clients, we deliver RCM, EHR, coding, analytics, and data tools.
Join us at demo station 23 at booth 2812 to learn more about Microsoft Dragon Copilot embedded within TruBridge Notes. We will host demos on:
- Tuesday, March 10, from 12:30-2:50pm
- Wednesday, March 11, from 3:10-5:30pm
- Thursday, March 12, from 9:30-11:20am
TrustCommerce, a RevSpring company

Booth 1624
Contact: Ryne Natzke, chief commercial officer
rynen@spherecommerce.com
Visit TrustCommerce, a RevSpring company, at booth 1624. For over 25 years, TrustCommerce comprehensive patient payment solutions have earned the trust of the country’s largest healthcare organizations. Now, together with RevSpring, we’re expanding integrated payments and accelerating innovation in financial engagement, combining Best in KLAS patient financial experience solutions with enterprise-grade gateway capabilities and deep integrated payments leadership.
Four reasons you won’t want to miss us:
- See how you can transform the way you process payments using TrustCommerce integrated solutions. Experience secure and compliant payment processing, anytime and anywhere – all while being seamlessly connected to leading EHRs like Epic, Veradigm, and AthenaIDX.
- Together, with RevSpring, you can have a more simplified payment ecosystem. End-to-end visibility enables reduced vendor complexity, improved reconciliation, and a more consistent patient payment experience across pre-service, point-of-service, post-service, and back office.
- See our patient-friendly digital payment experience that proudly supports digital wallets such as Google Pay, Apple Pay, and PayPal.
- Learn about partnership opportunities. Ask us how to integrate TrustCommerce payment solutions with your digital health software to drive revenue, reduce risk, and increase workflow efficiencies.
Swing by booth 1624 for a coffee, recharge with fresh juice, catch a live demo, and charge your phone while you’re there!
Visage Imaging

Booth 3753
Contact: Brad Levin, general manager, North America
blevin@visageimaging.com
540.454.9670
Visage is not only leading imaging’s move to the cloud, we’ve defined it. Visage is delivering Visage 7 | CloudPACS, an AI Optimized Enterprise Imaging Platform purpose-built and proven. Visage 7 | CloudPACS provides unparalleled speed, interpretation efficiency, and much needed relief from the current challenges facing radiologists, clinicians, and imaging IT professionals.
At HIMSS26, Visage will be demonstrating our latest Visage 7.1.20, including Visage Chat+, Visage 7 | Digital Pathology, and Visage Ease VP for Apple Vision Pro, as well as our latest work-in-progress efforts for Visage 7 | AI. Join us at booth 3753 and enjoy the best gourmet coffee available at HIMSS26, with coffee beans carefully roasted by Visage staff.


































































I saw that one, but I didn’t see anything about wrongful death or specific issues with medication displays within Epic.…