News 12/19/18
Top News
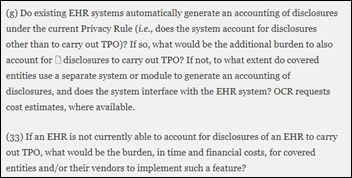
HHS OCR issues an RFI for help in identifying aspects of HIPAA’s privacy and security regulations that may be impeding value-based care and care coordination.
OCR is also interested in public comments about Privacy Rule changes it is considering, including:
- Rewarding or requiring providers to share PHI with other providers and families
- Requiring EHRs to include information about treatment, payment, and operations disclosures in the accounting of disclosures in separating “use” and “disclosure”
- Eliminating the requirement that providers get written acknowledgment that patients have received a Notice of Privacy Practices.
OCR is also looking at how long it takes for patients to get copies of their medical information, whether the currently allowed 60 days is too long, and whether covered entities should be required to give patients copies of their electronically stored information faster.
Also in the RFI is an important clue about OCR thought process – they want to know if providers are refusing to share PHI for treatment purposes or are requiring requesting providers to fill out request forms that go beyond HIPAA.
The long document is mandatory reading for those who follow HIPAA requirements and information sharing.
Reader Comments
From Med4295831: “Re: Greenway Health. Sent an email this week to all customers recommending that they file a MIPS hardship exemption for 2018 because Prime Suite’s Promoting Interoperability measures were calculated incorrectly.” Unverified, but the reader sent the email he or she says they received.
From Grand Delusion: “Re: PokitDok. One of several HIStalk sponsors being acquired. Thoughts?” We’re seeing the usual industry consolidation, but it does seem that my sponsors are often involved, for which I can offer these potential reasons:
- The companies were looking for exposure in hoping for that particular outcome.
- Companies moving up the food chain may sponsor at a higher rate and thus would attract attention otherwise simply because they are growing and honing their message.
- The exposure drew attention to them that they wouldn’t have had otherwise, perhaps of the Fear of Missing Out variety.
- Coincidence, especially since I have quite a few sponsors.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
Change Healthcare acquires “intellectual property and other key assets” of health IT API and blockchain vendor PokitDok, which Change will use to launch its API and Services Marketplace.
Canada-based health IT vendor Premier Health will acquire Cloud Practice, which offers an EHR based on an open source product developed by McMaster University, for up to $5 million, most of it in tiny-capitalization shares whose price has swung wildly between $0.04 and $0.85 in the past year.
ResMed’s string of health IT acquisitions continues as its Brightree post-acute care technology subsidiary acquires Apacheta, which offers mobile software for medical equipment vendors.
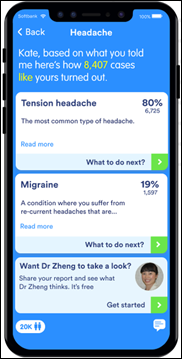
K Health, which offers a free AI-powered, questionnaire-driven app for consumers that uses a “People Like Me” history database, raises $25 million in a Series B funding round, increasing its total to $38 million. The company’s business plan apparently involves eventually selling its service to employers and placing referrals to paying doctors. The Israel-based company, formerly known as Kang Health, obtained its treatment history database from an HMO in Israel, which is likely a limitation for the US market.
Sales
- Johns Hopkins Medicine will implement Nuance Dragon Medical One and Dragon Medical Advisor for its “Joy at Johns Hopkins Medicine” physician burnout reduction program.
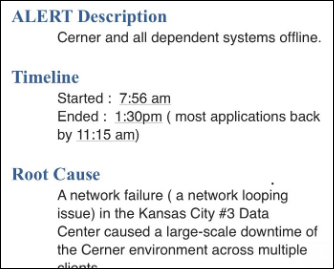
- Mid-Valley Hospital (WA) chooses Cerner Millennium and HealtheIntent.
People

FDA names Amy Abernethy, MD, PhD (Flatiron Health) as principal deputy commissioner for food and drugs.

Providence St. Joseph Health hires B. J. Moore (Microsoft) as CIO. Moore — whose background includes cloud, AI, and enterprise commerce – will report to the health system’s CFO, who also came from Microsoft. It’s an interesting choice for the country’s third-largest health system given that Moore has no advanced degree, no healthcare experience, and a deeply technical work history. It’s also odd that he’s reporting to the CFO, who also had no previous healthcare experience. I don’t know how EVP/CIO Janice Newell fits in – she’s still on the leadership page, but wasn’t mentioned in the announcement.

Todd Rothenhaus, MD (Athenahealth) joins medical equipment tracking system vendor Cohealo as CEO. He replaces co-founder Brett Reed, who will move to president.


Chronic disease management technology vendor Livongo Health hires Zane Burke (Cerner) as CEO, replacing Glen Tullman, who moves to executive chairman. The company also promoted Chief Medical Officer Jennifer Schneider, MD, MS to president. Livongo’s valuation is $800 million and Tullman has indicated that the company may go public in early 2019.

Paula LeClair (Onduo) joins Glytec as executive director and GM of outpatient.

Atrium Health hires Rasu Shrestha, MD, MBA as EVP/chief strategy officer.
Announcements and Implementations
NextGen Healthcare launches Health Data Hub, a cloud-based HIE platform for sharing and aggregation of patient data.
Netsmart will work with Kindred Healthcare to develop a clinical platform for long-term, acute care hospitals, rehab, and care management.
Government and Politics

Senator Lamar Alexander (R-TN), who is active in federal health IT initiatives in his roles of chairman of the Senate’s HELP committee and author of the 21st Century Cures Act, will not seek reelection in 2020 after serving three terms.
Other

Teladoc Health EVP/COO/CFO Mark Hirschhorn resigns following publicity and lawsuits over his romantic affair with a since-resigned Teladoc employee to whom he gave stock tips. The company had previously stood by its decision to discipline Hirschhorn with a one-year suspension of share vesting. TDOC shares dropped 6 percent after Monday’s announcement but regained ground Tuesday, having increased 35 percent in the past year vs. the Nasdaq’s 2.4 percent loss.
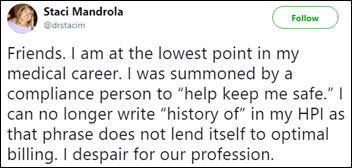
This tweet by a palliative care doctor drew interesting Twitter responses as she decried negation of “hundreds of years of our communication as healers” for not being allowed by compliance to write “history of” in the HPI (history of present illness). Some reactions:
- “History of” is not a good choice of words since it suggests that the condition has resolved.
- Doctors who argue that “I’ve always done it this way” also don’t see the benefits of turning their patients over to hospice doctors like the author.
- “Billing” is not the same as “compliance” and being counseled for the former posing as the latter is not ethical.
- The VA doesn’t have those problems – they use the language that’s best for communication among healthcare professionals.
- Just wait until hospitals try to make you document every inpatient as having malnutrition to make the numbers look better.
- Being paid by CMS requires jumping through hoops and the compliance officer is just trying to do their job in an insurance-driven world.
- Open a direct patient care practice and stop taking insurance.
A judge rules that the former CEO of St. Mary’s Hospital (FL) can sue CNN for libel over a report by Anderson Cooper in which the hospital’s pediatric surgery mortality rate was claimed to be running triple the national average. David Carbone, MHA says CNN compared the hospital’s 12.5 percent mortality rate for open heart surgery to a national average for all surgeries and didn’t risk-adjust the data. The hospital closed its pediatric cardiothoracic surgery program two months later amid public backlash, triggering CEO Cardone’s resignation. CNN argued that its report didn’t mention Carbone by name and that disagreeing with the method of comparing mortality rates doesn’t support a claim of intentional defamation.
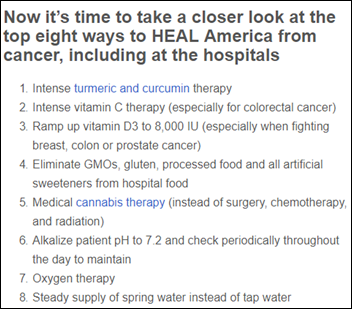
A cardiologist’s New York Times opinion piece called “Dr. Google is a Liar” says that fake medical news spread by social media and search engines (as in the above example, which features a video by the hilariously phony Dr. Leonard Coldwell) threatens our lives, making these observations:
- A woman had a heart attack after not taking her prescribed statin because she had read wacky Internet information from sites run by zealots, peddlers of alternative therapies, and people just looking for attention.
- False claims that HPV vaccine causes seizures has reduced vaccination coverage in Japan from 70 percent to less than 1 percent.
- Sites pushing alternative therapies for cancer argue that tumors are a healthy reaction, that surgery spreads harmful cells, and that medications cause cell mutations by increasing acidity.
- News sites regularly overstate alternative therapy benefits because less-rigorous observational studies that contradict medical wisdom make better stories than the not-shocking results of randomized controlled trials.
- Doctors should weave science with stories to become as effective as the “merchants of medical misinformation.”
Weird News Andy titles this story “Socks Appeal.” A man who sniffs his socks every evening after work when changing clothes develops a severe respiratory fungal infection from breathing in spores.
Sponsor Updates

- Casenet staff volunteer at the Christmas in the City event in Boston.
- Audacious Inquiry appoints Penny Thompson (CMS) to its board.
- EClinicalWorks publishes a podcast titled “How EClinicalWorks is Reducing the Risk of Physician Burnout.”
Blog Posts
- More Providers Sign On for MEDITECH Expanse in 2018 (Meditech)
- Go from ESignature LCD to MVP (Access)
- Your employee resigns unexpectedly. Here’s what to do next. (Advisory Board)
- Tools to Help Your Practice Optimize the End-of-Year Rush and Help Your Patients Optimize Their High-Deductible Medical Plans (Aprima)
- There’s a movement happening in healthcare IT (Bluetree)
- Takeaways from the 2018 AARC Conference (Bernoulli Health)
- The 2018 Hot List – What Healthcare Developers Were Reading (Datica)
- 6 Keys to Connected Care from Yale New Haven Health (Burwood Group)
- Physicians’ Compensation Remains Flat, Many Look to Revenue Cycle Management for a Revenue Boost (ChartLogic)
- 2018 Year in Review (CoverMyMeds)
- Innovation Amidst the Crisis: Part 4 – Resource Allocation and Access (Divurgent)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.



































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…