Katie the Intern 2/12/21

Interview: Rafid Fadul, MD, MBA, executive medical director, Wheel; and director of pulmonary medicine, Blanchard Valley Health System.

Email me or connect with me on Twitter.

Interview: Rafid Fadul, MD, MBA, executive medical director, Wheel; and director of pulmonary medicine, Blanchard Valley Health System.

Email me or connect with me on Twitter.

It seems like Cerner is going for the data play for their growth. That’s what Allscripts told Wall Street for the past five years and they never were able to execute on it. The solution in that space is not really a technology as much as it is a social process. Maybe they can pull it off. On a different note, CPSI seems to be more in the outsourced to Overseas billing business than in the EHR business these days. (IANAL)
This seems to me to be part of an ongoing problem space that really shouldn’t be part of a free market society. We have seen many examples of VCs buying facilities and clinics then turning them into profit centers. Be that through purchase of rural hospitals and using the lab systems to “outsource” labs at many multiples of the normal cost, or hospitals aggressively pursuing clinical debt up to and including leans on homes and garnishment. The stories are numerous and from credible sources (KHN, NPR, DOJ). Frankly, we shouldn’t allow venture capitalists into our health systems — their mission is to turn a profit and they use the opaqueness of the HC system to do that. A $46,000 rabies shot that normally costs $3,000? (AnInteropGuy)
Readers funded the Donors Choose teacher grant request of Ms. P in Pennsylvania, who asked for three sets of books covering math, space, and the environment for her elementary school class. She reports, “These books have made a big difference in our classroom. Since I am teaching virtually, I have recorded myself reading the books to the children. This way they can go back and listen whenever they wish. There are definite favorites. I don’t blame the children, I have my picks too. When we return back to in-person classes, these books will have a special home. They will have there own special shelves for easy access for the children. I can see them being read for years to come.”
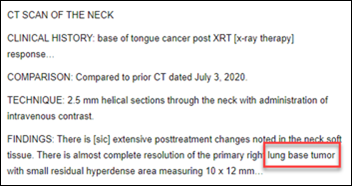
A patient in Canada who is undergoing treatment for throat cancer panics when new CT scan results that he saw on MyChart referred twice to his lung cancer. He couldn’t reach his oncologist, but the hospital connected him with the radiologist, who apologized that the transcription system had misheard his dictated “tongue” and instead documented “lung.” The patient says of his stressful reaction, “It confirmed my impression that the healthcare system has yet to establish an effective way for caregivers and patients to communicate except through in-person, video, or telephonic visits. I’ve not been successful in getting questions answered using the Cancer Centre’s Patient Support Line. And so far, MyChart has mostly wasted my time or misled me … I’m struck that when I read my CT report, I saw immediately that the reference to ‘lung’ was anomalous. If a layperson can see an anomaly, could we train an AI to catch one? Don’t dismiss the thought. I certainly don’t want a robot that autocorrects CT reports. But I do want one that can register surprise when something unexpected happens.”
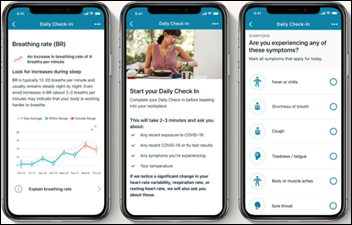
NASA will offer 1,000 employees, including astronauts, a Fitbit Charge 4 device and Fitbit’s Ready for Work app to help them decide whether they are experiencing COVID-19 symptoms and should stay home from work during the critical pre-flight period. The app tracks resting heart rate, heart rate variability, and respiratory rate and allows users to self-report symptoms, temperature, and possible COVID-19 exposure.

This is American culture and its healthcare system in a nutshell. Tessica Brown uses Gorilla Glue spray adhesive as a replacement for hair spray in a pinch, then spends 22 hours in the ED trying to get it removed. The daycare owner was finally freed of her adhesive hair net by a plastic surgeon, but meanwhile earned dozens of millions of TikTok video views, raised $22,000 in a GoFundMe to cover her medical bills for “this unfortunate ordeal,” and is reportedly planning to sue Gorilla Glue for misleading her (she denies reports that she’s suing). Not to be outdone, a fellow Louisiana resident – who previously earned his 15 minutes of fame on Dr. Oz for participating in the “ice cream challenge” of licking the contents of a carton of ice cream and putting it back on the store’s freezer shelf for someone else to buy — attempts to prove that Brown was exaggerating by gluing a Solo cup to his lip, then videoing himself triumphantly licking it off. That didn’t work as planned and he, too, ended up in the ED, where doctors peeled the cup off.
A UK hospital asks midwives to change their childbirth-related terms to be more inclusive – “mother” will be replaced by “birthing parent;” “her” will be retired in favor of “them;” “maternal” will become “maternal and parental;” and the new term for “father” will be “co-parent.”
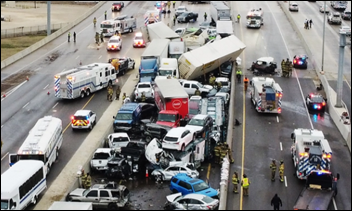
A Texas nurse whose car was pinned between two semi trucks in the early morning 100-car I-35W accident that killed six people crawls out through her trunk to free herself, hops the highway barrier to hitch a ride with a co-worker going the opposite direction, and goes to work.

Cerner Charitable Foundation Program Manager Allison Chael worked her other job as a Kansas City Chiefs cheerleader last weekend. Each team had to choose eight members of its cheerleading squad — the Chiefs have 33 cheerleaders on the roster – and they were not allowed on the playing field for this year’s game.

Cheering on the other side of the Super Bowl field was Tampa General Hospital ICU nurse and Buccaneers cheerleader Anastasia Lusnia, RN.

Providence, 13 other health care systems back data platform Truveta
Providence and several other big health systems form Truveta, a Seattle-based startup that will provide its hospital owners, drug companies, and researchers with anonymized patient data for approved research projects.
Watchdog: pause on VA’s $16B electronic health records project might be needed
A GAO report recommends that the VA postpone new Cerner implementations until it can address critical severity and high severity test findings.
Signify Health IPO prices well above expectations, valuing company at over $5.3 billion
Value-based care coordination and payments vendor Signify Health prices its IPO at a valuation of $5.3 billion.
Cerner Reports Fourth Quarter and Full-Year 2020 Results
Cerner reports Q4 earnings: revenue down 3%, adjusted EPS $0.78 versus $0.75, meeting earnings expectations and exceeding on revenue.
Providence and several other big health systems form Truveta, a Seattle-based startup that will provide its hospital owners, drug companies, and researchers with anonymized patient data for approved research projects.
The company notes that its information spans health systems and thus, unlike that offered by insurance companies, does not disproportionately represent white and insured patients.
Truveta, which is run by former Microsoft executive Terry Myerson, has hired 53 employees.
As with all such companies, patients do not share in the profit of having their information sold or used and are not required by HIPAA to be notified of the arrangement.
I ran across the latest HIMSS tax filings, for the year ending June 30, 2019, and provided a brief summary. The version that includes the first half of 2020 – and thus some of the HIMSS20 damage – will be posted in July.
Thanks to PatientKeeper for quickly snapping up the top-of-page banner spot for a long-term run. They have been an HIStalk sponsor since June 2008.
Listening: new from Jagwar Twin, the solo project of singer-songwriter Roy English. It’s modern, mostly upbeat pop with a hip hop edge, without the usual one-track collaborations, overreliance on computers, and profanity. I also ran across some amazing 1960s soul (from the viral hits chart of Portugal, for some reason) of Memphis-born soul singer-songwriter William Bell, who recorded for the legendary Stax Records, got drafted into the Army for a two-year hitch, had a couple of hits and awards, and is still playing at 81 years of age. His is the joyous, gospel-influenced music that could only come from America. I don’t recall ever hearing his stuff, but it is remarkable.
February 24 (Wednesday) 1 ET. “Maximizing the Value of Digital Initiatives with Enterprise Provider Data Management.” Sponsor: Phynd Technologies. Presenters: Tom White, founder and CEO, Phynd Technologies; Adam Cherrington, research director, KLAS Research. Health systems can derive great business value and competitive advantage by centrally managing their provider data. A clear roadmap and management solution can solve problems with fragmented data, workflows, and patient experiences and support operational efficiency and delivery of a remarkable patient experience. The presenters will describe common pitfalls in managing enterprise information and digital strategy in silos, how to align stakeholders to maximize the value of digital initiatives, and how leading health systems are using best-of-breed strategies to evolve provider data management.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Value-based care coordination and payments vendor Signify Health prices its IPO at a valuation of $5.3 billion. The company’s CEO is Kyle Armbrester, MBA, who along with several of his executive team peers, used to work for Athenahealth.

Cerner reports Q4 earnings: revenue down 3%, adjusted EPS $0.78 versus $0.75, meeting earnings expectations and exceeding on revenue. CERN shares dropped slightly on the news and down 1% over the past 12 months versus the Nasdaq’s 46% gain, valuing the company at $24 billion. From the earnings call:

CPSI announces Q4 results: revenue down 5%, EPS $0.22 versus $0.78, missing Wall Street expectations for both and sending shares down 11%. CPSI shares are up 25% in the past 12 months versus the Nasdaq’s 46% gain, valuing the company at $446 million. The company said in the earnings call that it has hired an advisor to review its business in hopes of increasing shareholder value. It also said in an SEC filing that it will reduce its workforce by 1%, or 21 employees.

Mary Lantin, MPH (Optum) joins Diameter Health as president/COO.

Innovaccer hires industry long-timer John Pigott (Allscripts) as management director of its payer and life sciences sales team.

Aver hires Michael Johnson (Rx30) as chief revenue officer.

EFamilyCare, which offers family caregivers virtual support from experts to reduce hospitalizations, promotes Naveen Kathuria, JD to CEO.
The HCI Group earns Meditech UK Ready implementation certification.

FDA issues 510(K) clearance to B-Secur’s ECG algorithm library for signal conditioning, heart rate, and arrhythmia analysis. The Northern Ireland-based company’s technology can be licensed by medical technology vendors and is approved for home and healthcare environments.
Well Health and Twilio partner to offer providers two patient engagement options, particularly around COVID-19 vaccination – supporting providers who want to built custom workflows using Twilio’s SMS and voice delivery APIs and those who would prefer to roll out Well’s Health pre-built platform that supports bidirectional texting, email, telephone, and live chat in 19 languages.
Smarter Health, which sells a payer-provider data integration platform in Southeast Asia, will offer data analytics from Health Catalyst.
Arkansas State Hospital goes live on Medsphere’s CareVue Cloud EHR and RCM Cloud.
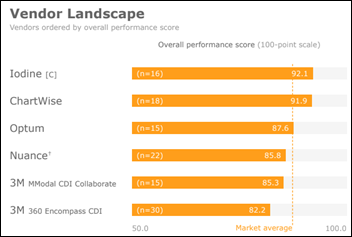
A new KLAS report on clinical documentation improvement finds that Iodine, ChartWise, and Optum lead in performance, while 3M 360 Encompass is often considered because of its strong technology but service and support lags and customers complain about being nickeled and dimed.
Renown Health (NV) will pay $75,000 to settle HIPAA Right of Access charges that it took 11 months to send an electronic copy of a patient’s records to her attorney.
CDC reports that 45 million doses of the 66 million COVID-19 vaccine doses that have been distributed have been administered (68%). Anthony Fauci, MD predicts that an increased supply of vaccine will allow any American to get a shot who wants one by April, but logistical limits will make achieving herd immunity unlikely before late summer. A new poll finds that one-third of Americans definitely or probably won’t get the vaccine, which predicts both an epidemiologic challenge as well as a shift from a shortage of supply to a deficiency of demand.
FDA issues emergency use authorization to a combination of two Eli Lilly monoclonal antibodies (bamlanivimab and etesevimab) for the treatment of COVID-19 in patients who are over 65 or who have other medical conditions, where risk of hospitalization and death can be reduced by 70%. Also new in COVID-19 treatment: the RECOVERY study finds that tocilizumab reduces mortality, inpatient stay length, and a need for ventilation of patients who are hypoxic and have inflammation.
Volunteer technologists have quickly developed vaccination appointment websites that centralize information from multiple sites in each state, but the beneficiaries are usually tech-savvy people who have time on their hands to cruise for appointments, not necessarily disadvantaged groups who have the highest need. Some of the sites don’t take into account eligibility differences between a state and individual counties, such as in California where the state’s 65-year-old threshold is overridden by the 75-year cutoff of some counties, leading people to show up at sites with their system-generated appointment and barcode in hand only to be turned away because they don’t meet county criteria.
The federal government says that a flood of fake 3M N95 masks from China is the most consistent COVID-19 scam, as hospitals have in some cases distributed the counterfeit masks to frontline workers. 3M says that 10 million counterfeit masks have been seized and it has fielded 10,500 authenticity questions. On the other hand, testing has found that the fake masks actually work about as well as the real thing, even though they are harder to breathe through and seal-and-fit isn’t always adequate.
Overrun hospitals in Mexico are sending COVID-19 patients home, where they are likely to die because their families can’t get oxygen tanks. A national shortage has caused the price to jump to $800 for the smallest tank (10 times the US price) and criminal groups are hijacking trucks carrying the tanks and stealing them at gunpoint from hospitals that are then sold by uncertified profiteers from their cars. Desperate family members are also paying thousands of dollars for oxygen concentrators that don’t necessarily work.
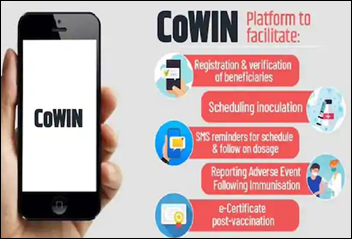
India will use Co-WIN to manage its efforts to inoculate 300 million people for COVID-19 by August, which has no ability to extract high-priority people from a list based on age and comorbidities. Epidemiologists say that the only surefire way to hit the numbers target is to go door to door and sign high-risk people up. They also question whether Co-WIN will be used to collect private health data since signing up for a shot automatically creates a national health ID that is supposed to be voluntary.

The IT director of 15-bed critical access hospital Syringa Hospital (ID) urges its board to stick with Cerner instead of following its plan to use Epic from Kootenai Health. The hospital says it is switching to gain cost savings and better connectivity to other Epic hospitals, but the IT director says it would “really grieve me” to re-do the work and warns that not all information will convert. She adds that Epic isn’t in the top five EHRs for small hospitals. A board member said she appreciates the input, but the IT director’s view is slanted because “that’s her baby,” adding that the board expected the hospital’s leadership to come to them with a recommendation and instead they were divided.
Blog Posts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.

Abhishek Begerhotta, MS, MBA is founder and CEO of 314e of Pleasanton, CA.

Tell me about yourself and the company.
I founded 314e in 2004. I used to work as a programmer on a project that IBM had undertaken to create a clinical information system for Kaiser Permanente. In around 2004, I think, Kaiser fired IBM and hired Epic. The rest is history. That’s when I founded 314e to provide services to Kaiser. Since then, we have worked with over 250 organizations across the healthcare value chain, including providers, payers, med tech, and life sciences companies. Our core areas of competence are EHR implementations, cloud, data engineering and analytics, interoperability, and automation. We take pride in delivering high quality at a reasonable price to our customers.
How are hospitals complying with the requirement to send ADT messages to the patient’s other providers?
We are working with a few customers on this. They all seem to have different issues and challenges, but I am unfortunately not up to speed on all of the details. I know that there are newer healthcare communication platforms emerging that facilitate this. 314e’s Muspell XI tool can also send ADT notifications, and we are working with a customer to integrate our tooling into their enterprise service bus to deliver these notifications to the right providers.
Where do most health systems fall in your eight-level Healthcare Analytics Adoption Model, and how are they prioritizing their next steps?
We think that most are somewhere in the middle, Level 3-5. We certainly have customers that are at Level 7, and we have helped them get there. Most organizations we know struggle with managing complex ETLs and getting data to a warehouse. The processes are brittle and do not support any form of self service or business agility.
We are seeing a trend towards adoption of cloud analytics platforms like Databricks on Snowflake running on Azure / AWS. These systems give the basic infrastructure on top of which high quality BI, AI/ML workloads, etc. can be run. Our customers are tapping us to migrate from decades-old warehouses to such more modern data lake / warehouse environments to get to Level 6 and higher. In fact, we are helping several customers today in collating EMR, imaging, lab, registration, claims, patient satisfaction, and home health types of data into FHIR-based enterprise data lakes. This results in getting to Level 4-5 in under a year.
Will the move to virtual implementation and support services continue even after some degree of normal travel resumes?
The pandemic has really exposed a lot of inefficiencies and waste in the healthcare industry, and one of those is the cost of travel and lost productivity for implementation consulting. With the shift to virtual, we’re adapting and becoming accustomed to doing things remotely, leveraging modern technologies like Teams and Zoom.
There are certainly some things lost by not having those face-to-face interactions where you build and strengthen relationships and alignment between IT and operations. So I do believe that some key personnel will start traveling more frequently when normal travel resumes. But overall, my gut tells me this trend of virtual implementations will continue.
Training and at-the-elbow support, specifically for new implementations, are two key areas that are presenting unique challenges for our clients to deliver virtually. I anticipate, at least for new implementations, that we will see those services resume to more in-person. We have spent considerable investment developing solutions and a product for our clients to address ongoing new hire training and ongoing on-the-job performance support which can be delivered digitally anytime, anywhere and provides on-demand targeted training assistant embedded in the EHR workflow. That trend is moving to more virtual.
How much interest or potential are you seeing in robotic process automation?
RPA adoption has been turbocharged by the pandemic. Providers and payers have both realized that RPA can make the processes more efficient and reliable in addition to the cost savings it brings. A Gartner report published in the middle of 2020 said that around 5% of healthcare providers in the US have invested in RPA and that this number will reach around 50% in the next three years. However, almost all of our customers have started at least one pilot initiative around RPA in some way, shape, or form, and many have at least one proof-of-concept in place. Most of them don’t have in-house capability to deal with this and are working with partners like 314e.
As a company, we are very bullish on automation, web automation as well as desktop app automation. We are building products to help customers deploy RPA to automate enterprise workflows. We believe that there is a need for an RPA framework which can allow healthcare providers to quickly and easily deploy an army of bots for different problems and design an orchestration system to manage these bots. We are piloting our bot orchestration system with a customer today.
How will payer-to-payer data exchange improve member experience?
CMS mandated the payer-to-payer data exchange to prevent fragmented member data from getting stuck in silos with different payers. Members can now have one unified record of all their health data, including claims data. This allows for a true continuum of care, not just across providers, but also across payers as the member switches jobs and possibly moves from one payer to the other. Payers need to use USCDI for this exchange. 314e has invested heavily in FHIR to help payers power such an exchange.
What 3-5 year goals do you have for the company?
At 314e, we are playing the long game; the infinite game. We started out as a few people helping a large IDN with data conversion. Then we got into staff augmentation on Epic implementations. But today we are true technology partners to customers across the healthcare continuum. Our goal is to become the go-to technology provider of services for cloud, analytics, integration, innovation, and automation for healthcare.
We want to do this by IP-led service delivery and products. We already have multiple products in the market, including one that we call Speki, which means “wisdom” in Old Norse. Speki is a content, help, video delivery platform with a SMART on FHIR launch. It is currently on the Epic App Orchard. We can take instructor-led EHR training, convert it into byte-sized chunks, and make that searchable and viewable from within the EHR.
Similarly we have a FHIR-based enterprise data lake product that we call Muspell. It supports archival and clinical data repository use cases and can be a data aggregation platform used by providers and payers. We run this on top of Databricks and it is available on both AWS and Azure. We have dozens more product innovations that we want to bring to market in the next 3-5 years.

Even with all the turmoil the US has gone through in the last several months, the institutions of government are still going strong, and the folks at CMS have not missed a beat. They did, however, extend the deadline for submission of 2020 data for the Medicare Promoting Interoperability Program. You now have until April 1, 2021 at 11:59 p.m. ET to attest through the QualityNet portal.
New Hampshire lawmakers have introduced HB 602, which aims to eliminate existing provisions protecting telehealth coverage. It would eliminate coverage entirely for audio-only services, which may have the unintended consequence of reducing access for those either not able to access the internet or who aren’t technically savvy enough to manage audio/video links. Surprisingly, one of the bill’s sponsors, Representative Jess Edwards, was one of the co-sponsors of the 2020 law that created payment parity for telehealth coverage.
As a telehealth physician, audio-only visits can be high quality interactions. In addition to the limitations above, some patients are just not comfortable on video due to their living environment or other factors. We’ll have to see whether this bill makes it through the process or not.
The ongoing usefulness of telehealth is discussed in this recent Journal of the American Medical Association editorial. The authors note that both patients and clinicians may want to continue virtual visits and that those visits could be as effective as in-person visits or used in conjunction with in-person visits as a hybrid model. Concerns about use of telehealth in the absence of hands-on examinations are valid, particularly when considering the overuse of expensive tests in lieu of physical diagnostic skills. Still, some conditions don’t require extensive physical examinations, but do require a physician’s cognitive effort.
For example, I was diagnosed with a food allergy a few years ago and I now doubt that diagnosis. I’m trying to get a second opinion from an allergist. The next available appointment that meshes with my work schedule is two and a half months away. No physical exam elements are part of this evaluation, and I recently had a full physical exam with the findings available in the shared EHR. Essentially, I need a learned expert to perform a review of my existing records and have a discussion with me about the risks/benefits of testing to determine whether it’s worth trying to proceed.
I’m willing to pay for the physician’s knowledge, experience, and time, but the construct in which we operate requires me to drive halfway across town to do it instead of being able to teleconference with the provider in the open slot that she has on Friday that would work with my schedule except for the drive time.
Of course, not every visit is suitable to a non-visit approach, but it’s time we think outside the box and focus on patient access, delivering high-value care in ways that are win-win for everyone involved. Real concerns also exist about fraud, abuse, and low-quality care. I would argue, however, that telehealth can be an important adjunct to whole-person care and for scenarios where a physical exam isn’t necessary or a recent exam is well documented. It could save a substantial amount of time and money for all parties involved.

I’m continuing to follow up on some random leads from the Consumer Electronics Show. One of them was a note that I made for voice-activated faucets. Kohler has launched a not only operate on command, but can measure specific amounts of water. The faucet also connects with a smartphone app that allows households to monitor water usage and be notified if it appears anything is out of the ordinary. Some models even offer a “wash hand” command that will instruct a user through the recommended steps for handwashing, including audible guides for lathering, cleaning, and rinsing. For parents who are tired of hearing two rounds of “Happy Birthday” as they try to instill good habits, it’s tempting, but the $1,700 MSRP is daunting. Most of us will have to go back to the old-fashioned egg timer and some adult supervision.
I enjoyed having easy access to the CES materials and sessions for a reasonable time after the show. Whatever HIMSS plans for its hybrid conference in August, I hope they improve their learning management system, because trying to find the sessions you want to watch after the fact is sometimes daunting. As someone who used the HIMSS sessions in the past for Maintenance of Certification credit for my informatics boards, it always seemed like the sessions I wanted to attend were on top of each other and watching after the conference was the answer. I hope they announce more information soon about the hybrid format, because I need to make some hotel decisions soon.
I had some additional adventures as a patient this week. The local hospital sent me an email reminding me that I had a bill due that I actually paid a month ago. I tried to use the integrated chat function to get it clarified, and the first thing I experienced was that despite the chat requiring me to enter the bill’s ID code along with the amount due (so that it could presumably be made available for the agent when he arrived in the chat), the agent asked me whether the bill was for a different amount that has never appeared on my account. I also quickly noticed that the chat client had no audio indicator that the agent had messaged me, so I had to sit there and stare at it to know if there was a communication. The agent kept telling me I had a zero balance despite the email and the home page that clearly showed a balance, and then told me not to worry about it.
I asked him to please escalate the fact that the system is sending balance due emails to patients with zero balances, since I’m a referring physician as well as a patient and know that would bother my patients as much as it bothered me. He then decided to tell me it is a known issue and that they are working with the vendor to resolve. I’m not sure why he didn’t tell me that up front when he realized my issue looked like one of the known issues, or why he decided to tell me once I said I was a physician, but either way, It wasn’t outstanding customer service. I hope the vendor gets their act together and fixes the defect soon because it’s annoying to say the least.
Do you feel like your healthcare team has accurate billing practices? Or do you see a high volume of patient complaints? Leave a comment or email me.

Email Dr. Jayne.
This information is from the 2018 Form 990 of HIMSS, which covers the tax year ending June 30, 2019. The 2019 form, which will include the first half of 2020 when HIMSS20 was cancelled, will be filed in July 2021.
Income and Expense
Total revenue: $112 million (up 18% from the previous year)
Total expenses: $91 million (down 5.5% from the previous year)
Revenue less expenses: $21.2 million (versus a $1.2 million loss the previous year)
Program Service Revenue
Conferences: $42.8 million
Corporate sponsorships: $13.1 million
Membership: $12.9 million
Advertising and media: $10.0 million (classified as unrelated business revenue)
Analytics and maturity models: $3.0 million
Revenue from Related Organizations
HIMSS Media: $13.2 million
HIMSS Analytics: $3.0 million
Personal Connected Health Alliance: $2.6 million
HIMSS Europe: $1.6 million
HIMSS also reported taxable partnerships through its Healthbox consulting firm.
Major Expenses
Conferences: $15.9 million
IT: $6.4 million
Occupancy: $2.2 million
Travel: $4.1 million
Highest Compensated Employees
Steve Lieber, former president and CEO: $2,666,485 (retired December 2017)
Hal Wolf, president and CEO: $1,291,414
Carla Smith, EVP: $671,788 (resigned November 2018)
Bruce Steinberg, managing director, international: $548,909
John Whelan, EVP, HIMSS Media: $426,732
Blain Newton, EVP, HIMSS Analytics: $451,265
Stephen Wretling, chief technology and innovation officer: $393,866
Patricia Mechael, EVP, Personal Connected Health Alliance: $355,787 (six months)
Total salaries and wages: $38 million for 459 employees, plus $4.1 million in pension plans and other employee benefits.
Alleva Raises Seed Funding to Further Capacity to “Help the Helpers”
Behavioral health EHR startup Alleva raises an undisclosed amount of seed funding, bringing its total raised to $3 million.
OCR Settles Fifteenth Investigation in HIPAA Right of Access Initiative
Renown Health in Nevada will pay $75,000 to settle allegations that it violated HIPAA by failing to fulfill a patient’s medical records request in a timely manner, including sending digitized records to a third party.
Therapy Brands, backed by Lightyear Capital, Oak HC/T, is up for sale
Therapy Brands, parent company of numerous mental and behavioral health software brands, puts itself up for sale.
Sitka Secures $14M in Series A Financing Led by Venrock to Help Transform Specialty Care
Virtual consult company Sitka raises $14 million in a Series A round led by Venrock.
Nuance Announces First Quarter 2021 Results
Nuance announces Q1 results: revenue down 4%, adjusted EPS $0.20 versus $0.22, beating Wall Street expectations for both.
Several weeks after raising $3.7 million, medical billing startup Gentem Health raises $10 million in a Series A round led by Vulcan Capital.
Nuance acquires Saykara, a developer of automated charting software.
Saykara founder and CEO Harjinder Sandhu, PhD was an executive in Nuance’s healthcare research and development division before co-founding automated patient engagement company Twistle in 2011 and Saykara in 2015.
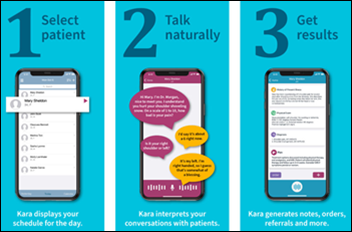
Nuance will assign Saykara’s 30 employees to its Dragon Ambient Experience (DAX) team. A stock analyst asked Nuance how they would keep Sandhu since “he keeps leaving and developing more stuff you guys are buying” (he was a co-founder of Nuance acquisition MedRemote as well). Nuance CEO Mark Benjamin says the opportunity with the acquisition was to combine the scientists of both companies.
I interviewed Harjinder Sandhu this past October, when I asked him how he would compare Saykara’s Kara to Nuance’s DAX.
From Equity Management Person: “Re: SPACs. Here are some counterpoints.” Thanks for providing an expert’s point of view in response to my cheap-seats comment about the SPAC phenomenon. EMP makes these points:
From Dry Heat: “Re: Super Bowl commercials. You should have a similar contest for health IT vendor ads.” I’m not sure that companies in our industry have the media savvy or cash to produce jaw-dropping ads given their niche B2B audience, but an ad contest for HIMSS conference week would be fun in the presence of adequate enthusiasm, even in the form of creative video messages rather than “commercials.” My favorite Super Bowl commercial is “Terry Tate: Office Linebacker,“ but it’s also an illustration of entertainment versus commercial success — Reebok ended it fairly quickly despite endless watercooler buzz because the connection to the company was subtle and sales were mostly unaffected. Reebok shoe competitor K-Swiss later produced the most profanely funny and Tate-like video I’ve seen (NSFW and definitely don’t click if you don’t know for sure that you like the always-offensive and profane “Eastside & Down.”) K-Swiss was brave for featuring Kenny Powers, MFCEO, but buzz aside, they sold the money-hemorrhaging company to a Korea-based outfit shortly after.
Welcome to new HIStalk Platinum Sponsor ChartSpan. The Greenville, SC-based company is the largest managed service provider of chronic care management (CCM) programs in the United States. It provides turnkey managed care coordination and compliance programs for doctors, clinics, and health systems. ChartSpan manages patient care coordination and value-based programs for more than 100 of the most successful practices and health systems in the United States. In addition, ChartSpan offers a SaaS-based Annual Wellness Visit program that allows practices to maximize their AWV capture rate by simplifying the AWV process. Through these offerings, ChartSpan is able to help practices increase their reimbursements while improving patient outcomes. Thanks to ChartSpan for supporting HIStalk.
Here’s a good “what we do” intro video from ChartSpan that also defines the value of chronic care management.
I subscribed to the online edition of the AP Stylebook since I refer to it often in choosing to follow most (but not all) of its own standards. Below are some I follow except when I slip up:
I noticed that the Walgreens website wasn’t working this morning, which from Googling seems to have been the case for a couple of days.
February 24 (Wednesday) 1 ET. “Maximizing the Value of Digital Initiatives with Enterprise Provider Data Management.” Sponsor: Phynd Technologies. Presenters: Tom White, founder and CEO, Phynd Technologies; Adam Cherrington, research director, KLAS Research. Health systems can derive great business value and competitive advantage by centrally managing their provider data. A clear roadmap and management solution can solve problems with fragmented data, workflows, and patient experiences and support operational efficiency and delivery of a remarkable patient experience. The presenters will describe common pitfalls in managing enterprise information and digital strategy in silos, how to align stakeholders to maximize the value of digital initiatives, and how leading health systems are using best-of-breed strategies to evolve provider data management.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Talent solutions company Ettain Group acquires INT Technologies, a veteran-owned staffing and consulting company that serves a variety of industries including healthcare.
Sitka raises $14 million in a Series A funding round, increasing its total to $22 million. The company offers PCPs the ability to virtually consult with specialists using its VConsult software.
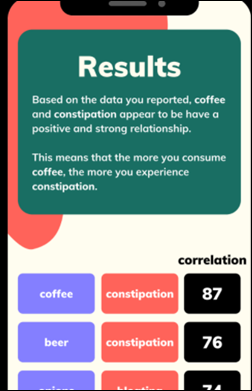
Paging Weird News Andy: microbial sciences company Seed Health acquires Auggi, whose AI technology analyzes pictures of bowel movements to assess gastrointestinal health. Auggi also offers an app for use in clinical trials, while Seed will launch a consumer app this year.

Nuance announces Q1 results: revenue down 4%, adjusted EPS $0.20 versus $0.22, beating Wall Street expectations for both. The company said in the earnings call that revenue for Dragon Medical and Dragon Ambient Experience (DAX) rose 22% over Q1 of last year, with DAX contributing $10 to 20 million in annual recurring revenue and customers expanding their implementation to additional medical specialties.

Jeff McHugh (R1 RCM) joins Innovaccer as regional VP of sales.

Bret Cottick (Olive) joins Medical Informatics Corp. as national VP of sales.
Beauregard Health System (LA) goes live on Meditech Expanse with consulting help from Engage.

Wake Forest Baptist Health (NC) implements RxRevu’s SwiftRx Direct real-time prescription benefit software.
Blessing Health System (IL) develops a home-based care program for COVID-19 patients using remote patient monitoring and telemedicine software from Cloud Dx.

The 377th Medical Group at Kirtland Air Force Base in New Mexico will go live on Cerner Millenium in April as part of the DoD’s continued rollout of MHS Genesis.
True Health (FL) leverages Emerge’s ChartGenie and ChartScout technologies in its conversion to Athenahealth.
All US COVID-19 measures are trending down significantly to early fall 2020 levels, with the hospitalization number slipping to around 80,000. US deaths are at 465,000, 20% of the world’s total. CDC reports that 42 million of 59 million distributed vaccine doses have been administered (71%).
The hottest topic among epidemiologists – should the 90 million Americans who have already had COVID-19 receive just one dose of vaccine? Consensus seems to be yes given the performance of the vaccines in clinical studies and the need to maximize the use of a limited supplies of vaccines.
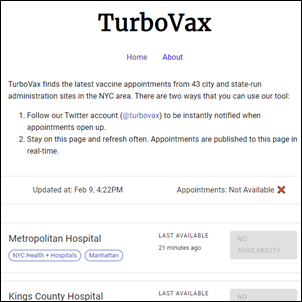
Another software developer takes it upon themselves to create an easy-to-use COVID-19 vaccination sign-up site. Huge Ma, a 31-year-old Airbnb software engineer, spends five days developing TurboVax, which compiles all available New York City appointments from the several signup systems and locations. Others have developed similar sites in New York and elsewhere. A Manhattan clinical psychologist who realized that none of her elderly relatives could have made their own appointments by finding the sites and booking a time slot online before someone grabs them concludes, “The system is set up to be a technology race between 25-year-olds and 85-year-olds. That’s not a race, that’s elder neglect.”
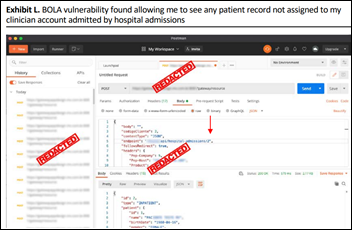
A security researcher’s analysis of 30 popular health apps (they weren’t named) finds problems:
Imagine if this were a hospital: a remote hacker gains access to a Florida city’s water treatment system and increases the amount of sodium hydroxide to dangerous levels, which was luckily noticed and quickly reversed by a supervisor who happened to observe the change happening on his computer screen. The city has disabled the remote access function that the hacker used.
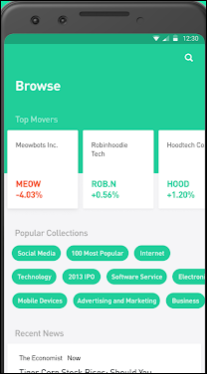
Another news item that may bear healthcare lessons, especially about consumer usability and how medical apps are supported. The family of a 20-year-old student sues trading firm Robinhood after he kills himself upon seeing his account balance reach a $730,000 loss. Alex Kearns, who tried unsuccessfully to reach someone at the company several times before taking his own life, didn’t actually owe $730,000 – he didn’t realize that Robinhood’s on-screen balance didn’t include the value of his unexercised options, which would have given him an overall $16,000 profit. The last words of his suicide note, in which he said he had “no clue” about what he was doing, were, “How was a 20-year-old with no income able to get assigned almost $1 million worth of leverage?” The company says it has improved its user interface, added help desk staff, and started asking new users about their finances and trading experience.
Blog Posts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.

Six Health Information Exchange Organizations Across the U.S. Form New Consortium
CRISP, CORHIO, CyncHealth, Health Current, IHIE, and Manifest MedEx band together to form the Consortium for State and Regional Interoperability.
Nuance Announces Acquisition of Saykara
Nuance acquires AI-powered mobile voice assistant and automated charting software vendor Saykara.
Ettain Group Acquires INT Technologies, a Technology Staffing & Consulting Company
Talent solutions company Ettain Group acquires INT Technologies, a veteran-owned staffing and consulting company that serves a variety of industries including healthcare.
It’s been a pretty crazy week in the clinical trenches, with COVID cases ticking up in my area. I’m approaching my one-year COVIDversary, memorializing one year since the day I saw my first COVID case, which happened to be one of the first five in my city.
I laugh a little thinking about it, since of course it presented itself at the urgent care as so many other health conditions do. It wasn’t some diagnostic mystery at a tertiary medical center, or an academic puzzle for someone like House. It was a household contact of someone suspected to be infected, who presented to our office saying she had a fever and couldn’t smell dirty diapers. My physician assistant and I spent the next several weeks wondering if we were going to die. Little did we know that the day would come when we would be seeing 15 to 20 known positive patients a day, with essentially the same level of employer-provided personal protective equipment we had prior to the pandemic (although many of us are supplying our own N95s).
Urgent care centers are healthcare’s front door for many patients who might not have a primary physician or who can’t see theirs during hours that are convenient. Even before COVID, our practice was seeing significant growth, having expanded from five locations to more than 20 in the five years I had worked there.
In November, I was having heated phone calls with our governor’s office about their vaccine plan that left non-hospital-owned urgent cares out in the cold. They were incredulous that urgent care offices treat COVID patients. “When did that start?” they asked. That would be March 14, when COVID-19 first crossed our state lines. The staffer seriously thought that all COVID patients were being seen in the emergency department, which doesn’t give me great confidence in our state understanding how healthcare is delivered to its residents. They also didn’t fully grasp that my practice performs almost 10% of the state’s COVID testing and diagnoses sometimes 500 new COVID cases a day. Seeing more than half a million patients a year, damn straight we’re on the front lines, so how about sending us some vaccine?
As I reflect back on the last year, it’s been a wild ride. At the beginning of COVID, we had to temporarily close several of our locations due to low volumes. I was furloughed without pay, something I never expected to happen as a physician. Once we started offering testing, though, it was off to the races, with volumes going crazy. I’ve mentioned before that in my clinical world I’m just a worker bee, an hourly physician with no leadership responsibility. However, due to my experience and as a consultant, I’m constantly analyzing the actions of my employers against what I might do or recommend that my clients do in a similar situation.
Some of the things they’ve done have been good. Retention bonuses for our clinical support staff helped boost morale and prevent turnover, particularly when patient volumes were high. However, they never did anything to bolster physician morale. When we brought it up, we were told that we should be glad to have jobs since one of the local health systems had completed a significant physician layoff. That never makes one feel good.
Neither does learning that your employer accepted millions of dollars in Paycheck Protection Program funds despite a clinical rebound that had us seeing more patients than we have ever seen in organization’s existence. It’s particularly special when you read about the PPP amount on the front page of the local paper right after seeing an email from your boss that everyone needs to tighten their belts because of the finances. They weren’t following any communications playbook that I would recommend as a consultant, that’s for sure.
The “acting poor” strategy also didn’t play very well when they announced that we were opening additional locations even though we couldn’t fully staff the existing ones. As a part-timer with other sources of income, I had the luxury of being able to push any negative reaction to the back of my mind, but I watched some of my full-time colleagues begin to look for employment elsewhere. Burnout is real and 12-hour shifts are rough, especially when they routinely stretch to 13 or 14 because you’re never allowed to say no to patients who are streaming in the door. I watched several of my favorite physician assistants leave for jobs with eight-hour shifts at local hospitals and have to say I was a bit envious.
I suspected something major might be up several months ago when they hired a new member of the C-suite, but didn’t announce his presence to the physicians. I met him walking through my patient care area after he had been on the job for a couple of weeks. I was underwhelmed by his demeanor and the fact that he was oblivious to my full patient board and the 40+ patients on the parking lot wait list and wanted to stand there and chat. I was even more underwhelmed a week later when his announcement email finally arrived, not from the CEO or COO, but from himself. At that point, I decided to start looking for other clinical opportunities, even though I knew that part-time physician spots basically don’t exist in my community and I’m only in this one because I’ve been here so long.
Toward the end of an already busy clinical week, we received an invitation to an all-hands meeting a couple of hours from when the email was sent. That’s never a good sign. Most of our staff meetings are at 6 a.m. so people can get to their shifts on time. During this quickie Zoom call, we learned that our previously physician-owned practice had gone the way of so many before us in being acquired.
I can’t say I’m surprised knowing the personalities involved, but it explains so much about how they’ve been managing the finances and some of the other decisions that have been made over the last several months. I’m sure it was all targeted towards making the balance sheet look as healthy as possible.
I’ve seen many versions of this movie before and I’ve never seen an ending that works out well for all parties. Inevitably, the investors want their money back and then some, and that money has to come from somewhere. I’m at a point in my career where the plot has to be pretty compelling for me to stay until the end and I’m not sure this fits the bill. I’ve done some research on the investors and I’m not impressed by their healthcare experience. Having participated in due diligence exercises with other organizations looking for outside funding, what I could find on them left me with quite a few questions and not as many answers as I would like.
Most people don’t realize that when physicians leave a clinical position, it’s not like quitting other jobs. It’s not unusual for physicians to be required to give a 90- or 120-day notice so that patients aren’t left in the lurch. Sometimes non-continuity practices like mine will accept less notice, but that’s not the case with my employer, who actually lengthened the notice period for some recent hires. There are some other things that were announced in addition to the investors, and frankly I’m not sure I want to be around when those proverbial bombs begin to drop.
I’ve been thinking about leaving for a while, and this might just be the push I need. When the handwriting on the wall wasn’t done with Sharpie but rather with red spray paint, it’s likely time to dust off the resignation letter. It’s an unsettling feeling since I’ve only resigned from two long-term jobs in my career, but I trust my gut, even in the middle of a global pandemic and without another clinical gig on the horizon. Time for my next leap into the unknown.
What’s your best job quitting story? Leave a comment or email me.

Email Dr. Jayne.
Building Evidence-Based Care Plans That Drive Better Outcomes
By Nan Hou, PhD, RN
Nan Hou is managing editor of Zynx Health, part of the Hearst Health Network, of Los Angeles, CA.

Evidence-based care plans play an essential role in guiding interdisciplinary care teams toward the most effective steps likely to yield high-quality care and the best patient outcomes.
For hospital-based interdisciplinary teams in particular, care plans offer several important benefits — including ensuring continuity of care across nursing shifts, promoting interdisciplinary collaboration across clinical and operational teams, improving patient engagement, and helping meet documentation requirements from payers and regulators.
However, too often, evidence-based guidelines either go ignored or take too long to implement. While estimates vary, the most frequently cited figure holds that it takes about 17 years for new knowledge generated by randomized controlled trials to be incorporated into practice. Even then, application is highly uneven, according to the 2001 U.S. Institutes of Medicine’s landmark report “Crossing the Quality Chasm.”
To promote greater adherence to evidence requires getting the right information to the right person at the right time in the workflow. For many hospital-based patients, this process begins with a care plan created by an interdisciplinary team that includes key information such as diagnosis and goals and is updated as the patient progresses. When developed by experienced care team and based on the best available evidence, care plans enable hospitals to standardize care, improve outcomes, and maximize performance.
One useful model for evaluating care plans is the Agency for Healthcare Research & Quality’s “Clinical Decision Support 5 Rights” framework. The model states that providers can achieve clinical decision-supported improvements in desired healthcare outcomes by communicating the following five “rights”:
Creating evidence-based practices
One of the foremost goals of evidence-based practice is to create standardized care that is supported by data and facts, reducing unnecessary variation in care. According to a report originally published in the BMJ, there are four key steps for creating evidence-based practices:
By following evidence, treatment is based on research and knowledge rather than tradition or intuition. Providers must weigh the value of evidence-based interventions, which requires critical thinking and an evaluation of the quality of the research and its conclusions. Instead of relying on their own personal beliefs, it is essential that providers select evidence that is centered on what is best for the patient.
Elements of a strong care plan
A well-designed care plan focuses on the whole person, taking into account both clinical factors and social determinants of health, such as economic security, and access to food, shelter, and transportation. While the plan must include interventions to treat the current medical issues, it must also help caregivers anticipate and manage the risk of future complications, including after discharge.
Further, it is essential that care plans foster a team-based, collaborative approach that reaches across disciplines in a variety of roles, including pharmacists, social workers, dieticians, behavioral health specialists, physical therapists, and occupational therapists.
To create care plans for individual patients, interdisciplinary teams use measurements from the latest clinical summaries, physician notes, and other electronic health record (EHR) data, in addition to information gathered directly from patients. For more common conditions such as heart failure, care team members often consult templates that identify the steps patients must take to achieve certain health goals, manage comorbid conditions, and avoid complications.
The importance of current evidence
Evidence, of course, plays a critical role in the development of care plans, but staying current with the best and latest evidence-based practices is a substantial challenge for any practicing clinician. For example, a study published in the Journal of the Medical Library Association estimated the volume of medical literature potentially relevant to a primary care physician published in a single month, and found that a physician trained in medical epidemiology would need 628 hours to evaluate all the articles.
To overcome this limitation, many hospitals rely on regularly updated content libraries that are built on the best available evidence, national guidelines, and performance measures. These content libraries include medical conditions and procedures, summaries of studies, and links to evidence in support of care recommendations. Armed with a source of reliable evidence-based content that can be easily incorporated into care plans, care team members can be confident that the plans they formulate are consistent with the most current and credible standards of care.
While virtually all healthcare stakeholders agree that using evidence-based care plans supports better patient outcomes, putting evidence into practice is often easier said than done. However, by leveraging pre-populated, evidence-based content libraries, hospitals can reduce much of the heavy lifting, empowering their interdisciplinary staff to develop care plans that facilitate communication and collaboration, ease care transitions, and ultimately drive superior patient care and outcomes.
Erik Littlejohn is president and CEO of CloudWave of Marlborough, MA.

Tell me about yourself and the company.
I joined CloudWave in 2013 out of a desire to be part of a team that served a terrific market, had great potential, and allowed me to continue my career in healthcare IT. One of the things that attracted me to CloudWave is that most of the people there had devoted their careers in and around various aspects of healthcare.
I was fortunate to join it at a pivotal point in its transformation. I initially led our technology services organization that focused on the resale of on-premise technology solutions, storage servers, et cetera. I got to interact with a ton of customers and serve a ton of customers. Then over the next eight years, we continued our transformation from being a legacy reseller of those solutions to a multi-cloud services, edge, private public cloud that solved numerous challenges faced by hospitals. We are building and continuing to build something special, and we cherish the relationships that we have had with customers going back many, many years.
What does the mix of on-premises infrastructure and cloud computing look like for the typical hospital, and how is that changing?
When I joined the company in 2013, 70% of our proposals were on-prem integration types of deals and 30% were cloud-based, whether that was full hosting or disaster recovery. As we sit here today eight or so years later, it has flipped and completely inverted. I would say that 65 to 70% of our proposals and solutions are cloud-based and the remainder are on-prem, or what we now call edge solutions.
Cerner was becoming more active in hosting its own systems back then as I recall, while Epic and Meditech weren’t doing much of that. What is different now?
Cerner continues with its model and there are no on-prem Cerner solutions. All of that is hosted, and they have been successful at doing that. Epic and Meditech have been similar, in that organizations like CloudWave have provided private cloud hosting operations or solutions. Meditech has certified a number of providers like ourselves to be able to do those, and we go through certifications or testing on an annual or biannual basis. Like everyone else, Meditech has wanted to associate themselves with a public cloud offering, and about a year and a half ago, they launched a partnership with Google. Cerner has launched a partnership with AWS and Epic has certified its platform to run on Azure or AWS as well. Everyone made their claim to a partnership. We are doing the same things and trying to evolve our solutions to be not only private cloud, but to take advantage of public clouds and their evolution.
What are the practical results of hospitals moving some of their data center operations to cloud providers?
Some of it becomes a preference based on financial models, whether it helps them to have an operational expense versus a capital expense, for example. A lot of organizations prefer CapEx, so the cloud may not fit that model very well. However, clouds, public or private, offer a lot of other benefits. Think about hospitals trying to maintain talent and the number of skills that you need for various software vendors, and keeping abreast of those certifications. Complex security challenges are daunting for organizations today, and it has been tough to keep up, particularly if you are a community hospital, with all the ransomware threats coming out of any number of countries these days. Then maintaining all of that talent over time. Healthcare certainly has been slow to adopt cloud solutions over the years, but they are becoming comfortable that that cloud can help them solve some of those challenges.
How has cloud deployment helped hospitals prevent ransomware attacks and recover from them?
First and foremost, it’s ensuring that you have the basics done of clean backups, that you have recover points that you can go to when – not if – someone is impacted by a ransomware or security event. Ensuring that there are multiple copies and multiple restore points and options you can go to so that you know you have a safe recovery point, and trusting in an air gap type of solution. We have multiple sets of data or backups available for customers, and that gets pretty expensive and complex for any organization to manage by themselves. That’s another reason that working with cloud providers makes a lot of sense for hospitals.
Why do attempts to restore from backups fail so often?
We test ours on an annual basis for our customers. That in and of itself is a huge difference. You think your backups are fine and you see that all the saves were occurring, but until you actually restore that and try to run the system, you just don’t know what you have or you don’t have. We feel like doing that annual test is critically important, and it’s a big reason that a lot of customers want to do that and choose a recovery service or a backup service with us. Otherwise, they probably wouldn’t do it on their own.
It becomes a good tool for the organization to rally around. They have this recovery test over the span of a week, they get clinicians involved, and they get people to pressure test it and figure out where the kinks might reside or find issues that need to be fixed. Figuring out what didn’t go well is as important as anything else in a test so that we can make sure they have a clean, restorable backup that they can rely upon.
What do hospitals typically need to do to prepare for moving to the cloud?
The funny thing about being a cloud service provider is that your service is only as good as the end user’s perception. Looking at connectivity and service providers in the local area is important, ensuring that you have multiple paths and redundancy in case a provider has an outage, that you have the capability to fail over and have adequate bandwidth when there’s some sort of outage with Verizon or AT&T, et cetera. First and foremost, you need to make sure that’s solid and that you have redundancy. You also need to make you have adequate Active Directory permissions and user access.
It isn’t just flipping a switch and saying, “I’m going to go into the cloud tomorrow.” We spend one to two weeks assessing the readiness of our customers and remediating any issues that may exist. That holds true with any cloud service provider. You need to be thoughtful about assessing anything in the environment that may impact an end user’s ability to use the system successfully, and make sure it’s not going to be slow, that it doesn’t time out, or that you don’t encounter authentication type of issues, because that creates a downstream headache for everyone.
How do you see the company’s business and strategy changing with its recent acquisition by a private equity firm?
We are excited about the Abry Partners investment. They have a great reputation and a ton of experience in our industry. We felt like they would help position us for future growth and enhance our capabilities, grow our team, and provide meaningful strategic input or guidance. Just as importantly, we just liked their team. There is a sense of familiarity, a lack of ego, and a near-perfect alignment about the potential of our business. We couldn’t ask for a better partner, and we know that they are willing and able to invest in capabilities that we need going forward, whether that’s acquisitions or building our organic capabilities.
What were the most useful lessons you learned from being a West Point graduate and an Army officer?
One of the things that I always talk about with the team is explaining why. That may seem counterintuitive if you’re thinking about the military and you think of people just being told to take the hill, salute smartly, and go do it. But in the military, we always concerned ourselves with the commander’s intent. I had to understand what was going on to the left and the right of me, why I needed to take that hill, and how that fed it into a larger objective. It is important as leaders to always provide that context and the “why” to our teams and the people we work with. Because if you just ask a question without context, they may not give you the right answer, or they may not meet the ultimate objective that you are trying to get to.
What will the company’s emphasis be over the next few years?
We will expand our use and footprint of public cloud and make that more accessible and user friendly to our end customers. That’s an important part of our growth in the next three to five years. We will continue to diversify our capabilities and provide more services than we do today beyond hosting and recovery and backup, providing other things like service desk and security services and expanding those. We will also diversify our customer mix. We have been pretty focused on the Meditech space up to this point, or hospitals running Meditech, but we think that nearly all of our solutions translate nicely to hospitals running other EHRs. We are having some success in Cerner hospitals and Epic hospitals, and we are anxious to do that and to serve a wider mix of customers.
Do you have any final thoughts?
CloudWave will continue to be a customer-first business. Our relationships with our customers have always been at the center of what we do, and we are going to continue investing and expanding in those relationships in various ways. We can be a great partner with customers that are looking to transform their operations through the adoption of cloud. We see the whole industry being at an inflection point and more aggressively adopting cloud, and we are in a great position to do that based on our experience. We look forward to helping customers in that journey.
Two Triangle biotech companies raise cash
Duke University spinout Clinetic, whose software monitors EHR activity to identify patients for clinical trials or to suggest next steps in their care, raises $6.4 million in equity.
More than 36,000 UPMC patients’ data potentially accessed in security breach
University of Pittsburgh Medical Center notifies patients of a security breach at vendor Charles J. Hilton & Associates that may have exposed their medical records.
Infinitus emerges from stealth with $21.4M for ‘voice RPA’ aimed at healthcare companies
“Voice robotic process automation” vendor Infinitus comes out of stealth mode with a $21 million Series A funding round.
Hackers post detailed patient medical records from two hospitals to the dark web
Hackers post patient information from Leon Medical Centers (FL) and Nocona General Hospital (TX) on the dark web.
Duke University spinout Clinetic, whose software monitors EHR activity to identify patients for clinical trials or to suggest next step sin their care, raises $6.4 million in equity.
CEO Thomas Kaminski was previously SVP of corporate strategy for LabCorp, board chair Allan Kirk, MD, PhD is surgeon-in-chief of Duke University Health System, and board member Rob Califf, MD is former FDA commissioner.
Founder Erich Huang, MD, PhD is Duke Health’s chief data officer and directs its health data science center and data science accelerator.

From Frumious Bandersnatch: “Re: your HIStalk mug from 2014. I love it! So sorry I missed that HIMSS since it would have been worth the trip. I realized today that I have been following you for many years now – glad you’re still here.” HIMSS conferences blur together, but I have the advantage of being able to refer back to my super-detailed HIStalk write-ups to remember what happened way back then. Memorable events of HIMSS14 (daily details here, here, here, here, and here) include:
From Carl SPACkler: “Re: SPACS. Good for the industry or no?” It’s hard to say, but a ton of health IT SPACs are out there and they are required by law to spend their money on acquisitions within several months, which means that many of them will end up with subpar, overly expensive dance partners that had little reason to become publicly traded and that will fail to attract ongoing investment afterward. It feels to me like everybody is desperate to get a deal done before the bubble bursts. Having your long-term vendor or employer go public is like having your significant other join a cult. It could be a rough ride for hastily acquired companies that needed more time to prepare for their financial close-ups.
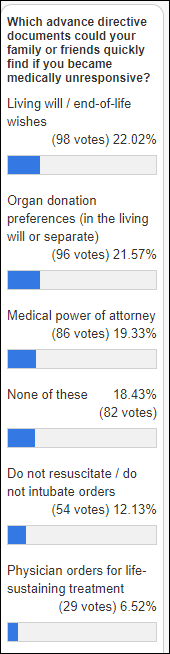
I will urge the significant number of folks who haven’t completed a living will and medical power of attorney to do it right now, then store the papers somewhere they can be easily located in a moment of need. You don’t need to spend money or hire a lawyer if that’s a barrier – you can download free, state-specific forms that you can complete in maybe five minutes and then you are set for life (or death). There’s no reason to put family members through the anguish of what you would want when it’s so easy to just tell them.
New poll to your right or here: What part of your medical record would you be most angry at having disclosed publicly? Some folks will indignantly say they need an “all of the above” option, but that’s not the point – it’s what single part of your chart is most sensitive to you. I guess mine would be credit card information since that’s the only item that would inconvenience me — the rest simply identifies me as boringly mortal like everybody else, should strangers actually care.
February 24 (Wednesday) 1 ET. “Maximizing the Value of Digital Initiatives with Enterprise Provider Data Management.” Sponsor: Phynd Technologies. Presenters: Tom White, founder and CEO, Phynd Technologies; Adam Cherrington, research director, KLAS Research. Health systems can derive great business value and competitive advantage by centrally managing their provider data. A clear roadmap and management solution can solve problems with fragmented data, workflows, and patient experiences and support operational efficiency and delivery of a remarkable patient experience. The presenters will describe common pitfalls in managing enterprise information and digital strategy in silos, how to align stakeholders to maximize the value of digital initiatives, and how leading health systems are using best-of-breed strategies to evolve provider data management.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.

“Voice robotic process automation” vendor Infinitus comes out of stealth mode with a $21 million Series A funding round. The company’s technology asks machine-generated questions in phone calls, such as for public health outreach and insurer inquiries, then tailors further questions based on responses. Most of the folks involved come from Google or Rakuten, but the standout for me is operations guy Brad Holden, who earned a Carnegie Mellon degree in mechanical and biomedical engineering; enlisted in the US Marines as a platoon commander in Operation Enduring Freedom in Helmand, Afghanistan, where his platoon cleared routes of insurgents and IEDs; and then came home to earn a Harvard MBA.


Patient engagement platform vendor PatientBond hires Justin Dearborn (ICM Partners) as CEO. He replaces Anurag Juneja, PhD, who will continue as president.
CDC’s vaccination stats: 41 million doses administered of 59 million distributed (69%). COVID-19 tests, cases, and hospitalizations are continuing their sharp trend downward, but deaths haven’t followed yet and are running more than 3,000 per day. COVID-19 cases in nursing homes are dropping off as vaccine rollout continues.
The more contagious B117 coronavirus variant is spreading in the US exactly as predicted, with cases doubling every 10 days on its way to becoming the dominant strain by March. Its spread makes the dialing back of mitigation measures by several states, such as expanding in-restaurant dining, appear unwise. It also increases the importance of getting people vaccinated quickly.
Johnson & Johnson requests FDA’s Emergency Use Authorization for its COVID-19 vaccine, although FDA’s advisory panel doesn’t meet to review its clinical data until February 26. Former FDA Commissioner Scott Gottlieb, MD says he expects J&J’s vaccine, which requires just a single shot, to be distributed through pharmacies because it does not require special storage other than normal refrigeration, while Pfizer’s vaccine will probably be limited to big distribution centers because it requires ultra-cold freezers.
Experts remind that while some of the available coronavirus vaccines have higher efficacy rates than others, all of them are 100% effective at keeping recipients from becoming seriously ill or dying.
The Multi-State Partnership for Prevention accuses CDC of misrepresenting Deloitte’s employees as their own during a demonstration of MSPP’s PrepMod vaccination software. CDC then gave Deloitte a $44 million, no-bid contract to develop a system that ended up working up much like PrepMod. The owner and only principal of the for-profit affiliate of MSPP that developed PrepMod has filed a cease and desist notice, pending a lawsuit, claiming that Deloitte stole her intellectual property and then tried to hire her to help it copy its functionality. Ten states are using the Deloitte VAMS system, which was free to them, while 28 have bought PrepMod. Another developer of vaccine information systems confirms that his company and his competitors were asked to participate in meetings with CDC and Deloitte, but then were shut out of bidding when Deloitte was contracted directly.
The White House invokes the Defense Production Act to manufacture 61 million at-home or point-of-care coronavirus tests by summer. It will also use DPA to increase the manufacturing of surgical gloves and two components that are used in Pfizer’s vaccine packaging.
Boulder Medical Center (CO) cancels the COVID-19 vaccination appointment of a 72-year-old cancer survivor because of an unpaid $244 hospital balance.
CDC confirms that US flu activity is basically zero, easing fears of a “twindemic.”
Hackers post patient information from Leon Medical Centers (FL) and Nocona General Hospital (TX) on the dark web.
Henry Ford Health System researchers find that the IPhone 12’s charging magnets can disrupt implanted cardiac defibrillators, leading Apple to issue a warning that users should keep the products 6 inches away from medical devices at all times at 12 inches away when the devices are charging.
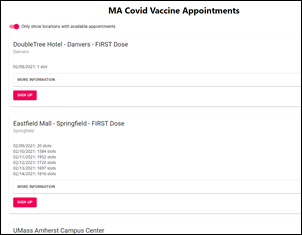
Olivia Adams, a 28-year-old software developer who is on maternity leave from Athenahealth, develops a COVID-19 vaccination sign-up website for those residents of Massachusetts who are 75 and older. She coded a site that scrapes information from a bunch of individual sites and displays available appointments in a central location. She said it was challenging because nobody asked the developers of the individual sites to make them interoperable.
Blog Posts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


A “dead” language (a proprietary one at that!) put food on my table and a roof over my head for 31 years until I was laid off in 2014. Alhough that effectively ended my coding career, I was able to apply all of the software life cycle best practices to become a Product Analyst in which I design the look, feel, and flow, and have a team of ‘modern’ developers do the magic. (Marshall)
I couldn’t agree more with Dr.Van Vert, but as a patient, I often feel woefully ill equipped to create an informed advance care plan. Besides revive or DNR, yes or no to breathing machine / feeding tube? There may be other decisions to be made, such as pacemaker, surgery, antibiotics for repeated UTI. What about relatives who disagree and fight my wishes? What about if my AD is not avail at time of crisis? IMHO, there is still much work to be done to educate patients and family members so that the conversations, once normalized, can be meaningful. (Kathy Kastner)
Ultimately though, this cannot simply be about end-of-life. You need to open the doors to patient priorities and issues throughout the entire healthcare system. We’ve got one big initiative called person-centered care. When you ask the patient upfront what they expect from the care episode, this sends that message. (Brian Too)
So, if I get this right, you were shown an internal error message as an end user (patient). One that should have gone to the user who selected the document in the first place or someone who could actually do something about the error. To say this is a poor user experience is putting it mildly. (AnInteropGuy)
I work for a CRM vendor and so I have that lens on as I read your story. What I see is that the actual test went just fine, it was your entire experience around the clinical event that caused you frustration. Imagine if through a series of coordinated text, emails, calls, chats you were guided exactly where to go, and were given the results in the appropriate context? Yes, there were some physical plant issues (CRM can’t help with dust bunnies), but aside from that, it was all communication. As one health system leader said recently, “the contact center is the new waiting room,” If your health system had a Digital Front Door, you would have had a better experience. (Brendan Ward)

Readers funded the Donors Choose teacher grant request of Ms. T from Texas, who asked for a ring light so her students can see her better while she is teaching virtually from home. She reports, “My wonderful students and I would like to thank you for your generous contribution. Teaching virtually has been a great challenge. With the light ring, my students have been able to see me much better on camera.I really, truly appreciate everything that you have done for us.”
A science futurist website questions whether the DNA information of 18 million people that is stored by Ancestry.com is safe in the hands of its private equity owner, Blackstone, which has pledged to find new ways to “package and sell data” as a revenue stream. A finance professor says, “[Blackstone] owns healthcare companies. They own insurance companies. They own retail companies. So they can identify spending behavior, health care expenses, actual health outcomes for individuals.” The article also questions how genetic information will be protected when 23andMe goes public via a SPAC that is owned by Virgin’s Richard Branson.

In the UK, a COVID-19 conspiracy theorist is banned from hospitals – except for emergencies and scheduled appointments – after filming empty hospital hallways to prove that the British government is lying about the pandemic.

A man who made money on last week’s wild ride of GameStop stock spends his profits on gifts for patients at Children’s Hospital of Richmond, where his son receives treatment for neurofibromatosis. John Theobald explains, “If a kid that’s stuck at the Children’s Hospital wants unicorn curtains, I’m going to get them unicorn curtains, as opposed to a slush fund.” Another investor, a 20-year-old student who made $30,000 in profit, donated Nintendo Switch games and consoles to his local children’s hospital.
Mother Jones finds that online nurse groups, including that of the ANA, are filled with COVID-19 vaccine disinformation. Nurses who post that they have been vaccinated are being attacked, threatened, and accused of harming their unborn children.
A 10-year-old boy and his mom’s friend head out after Monday’s snowstorm to clear the snow off cars of employees at Westerly Hospital (RI) so they could get home to their families faster.

In Canada, International Space Station astronaut and primary care physician David Saint-Jacques, PhD, MD returns to the medical front lines to work on the COVID-positive unit of McGill University Health Centre, where he completed his residency. He says, “In the space between the people who have no symptoms and the people who die from them, there are people who will get through it, but who get very sick, who really go through hell, on oxygen, pumped full of drugs, in the hospital, with an impact on their families. Now is not the time to let our guard down, even though we’ve all had enough.”

Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…