News 3/31/23
Top News
Senators Patty Murray (D-WA), Jon Tester (D-MT), and Sherrod Brown (D-OH) introduce legislation to overhaul the VA’s Oracle Cerner project, which would require the VA to:
- Develop metrics for deciding when and how new sites are brought live.
- Fix the patient safety issues that were listed in the VA’s March 2023 Sprint Report.
- Place further go-lives on hold until the five facilities that are live show an improvement in performance metrics compared to those they reported while using their previous VistA system.
- Bring in outside experts to renegotiate the Oracle Cerner contract.
- Develop a Plan B strategy in case Oracle Cerner rejects proposed contract terms or VA can’t get the technology to work.
- Reform its technology acquisition process.
- Add outside healthcare experts who have EHR rollout experience to its advisory committee.
Meanwhile, a group of Republican senators introduces legislation that would halt further VA go-lives on Oracle Cerner until significant improvements are made from a rigorous list of requirements.
Reader Comments
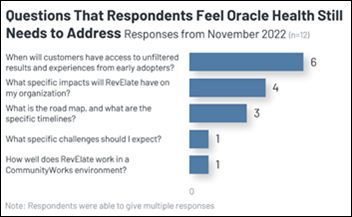
From Roky Erickson: “Re: Oracle Cerner. Our organization had a project pushed back because the company is having resource issues, and other CIOs tell me they are seeing the same. One even said that Oracle told them that VA issues are taking priority and commercial customer projects are being delayed.” Unverified. Let me know if you’ve experienced this – I won’t use names or specific details, of course.
HIStalk Announcements and Requests
I’ve added a calendar reminder to check Epic’s website Saturday for the usual April 1 shenanigans.
Last call for HIStalk sponsors to be included in my HIMSS23 guide that I’ll run shortly. Send me your details and you are in.
I’ve started tuning out anything that is written in the form of, “I asked ChatGPT to …” It was clever for about five minutes, but now it’s just tedious.
ViVE Observations From An Attendee

An HIStalk reader who is attending the ViVE conference sent these notes:
- Tuesday’s keynote by Micky Tripathi was the most substantive thing I’ve heard all week. He breaks out ONC’s work into three categories: (1) building a digital foundation via standards, IT strategy, and coordinating between federal agencies. He played up USCDI and UCSDI+; (2) making interoperability easier with FHIR APIs and TEFCA. He wants to make sure those required APIs are truly usable rather than vaporware and are extended to CDC connections; (3) encouraging information sharing, with information blocking enforcement provisions coming this year, which I am guessing means a draft rule in September.
- Other Tuesday headliners sounded like talking advertisements.
- Loving the multiple snacks through the day and the music of Chapel Hart.
- Wednesday was a light crowd, maybe 20% of peak attendance. I felt bad for exhibitors that so few buyers were around.
- I thoroughly enjoyed a presentation by Shiv Rao (Abridge) and Joon Lee (UPMC) on generative AI. They advise trusting the technology to assist a human, such as autopilot on a plane, but not to fly the plane unsupervised. UPMC’s evaluation of potential AI partners includes integration with existing workflows and systems, auditable output, a clinician-led organizational structure, a patient-centric solution, and 100% AI driven.
- While the event isn’t as grossly transactional as I feared, there is certainly an undercurrent of deal-making, which is probably intentional.
- Attendee mix will probably evolve. On the provider and payer side, you see more venture investors and innovation teams instead of CIOs and CISOs. EHR vendors are low key and on the periphery. Services-based vendors probably won’t get value from a booth since traditional IT execs aren’t going to be around much for meetings.
- Most presentations were on the ViVE floor and I liked that, with several presentation areas of varying sizes. It never felt noisy to have presentations going on, it was easy to move from one session to another, and you could follow applause to find good sessions. I wonder how the vendors whose booths were near the stages felt, however.
- The CHIME track was mostly separate with several member-only events, but participants participated in some general sessions as well.
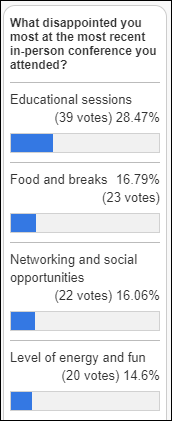
- ViVE shoots for a vibe of youth, energy, innovation, and fun in its branding, themes, opening remarks, and evening entertainment. Sounds great until you remember that your ticket cost nearly $3,000.
If you attended or especially if you exhibited, send me your thoughts about the conference and content, which I will share anonymously. Notes from the CHIME track would be interesting to readers, as would comparisons of ViVE to HIMSS.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Amazon brings its Health business to the website’s main menu, I noticed when looking for the new book “The AI Revolution in Medicine: GPT-4 and Beyond” ($15.49 for the Kindle version, which caused a collision between my curiosity and parsimony).
McKesson-owned CoverMyMeds will lay off 815 employees; close its Scottsdale, AZ patient support center; and rent out space in the $240 million Columbus, OH headquarters building that it moved into in May 2021.
Florence, which offers a patient engagement app, emerges from stealth with a $20 million seed funding round.
Sales
- Healthcare Triangle announces a $3 million cloud managed services sale to an unnamed life sciences company.
Announcements and Implementations

ViVE 2024 will be held in Los Angeles February 25-28 at the Los Angeles Convention Center downtown.
National Quality Form endorses nursing home hospitalization and re-hospitalization analytics solutions from Net Health, the first LTPAC EHR or analytics vendor to develop NQF-endorsed quality measures.
UnitedHealthcare will eliminate 20% of prior authorization items in the next few months. The insurer will also implement a Gold Card Program to eliminate most prior authorization requirements for provider groups that have been historically compliant.
Government and Politics
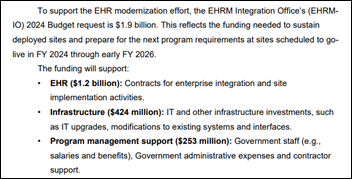
VA Secretary Denis McDonough warns that proposals to cap the agency’s budget at 2022 levels will harm its Oracle Cerner implementation. The VA’s 2024 budget request includes $6.4 billion for infrastructure modernization and $1.9 billion for the EHR project. Meanwhile, McDonough says the VA will review its contract with Oracle Cerner, which it signed in May 2018 with a five-year review built in, which he says will drive scheduling of the next go-live because “this contract may not be what we need.”
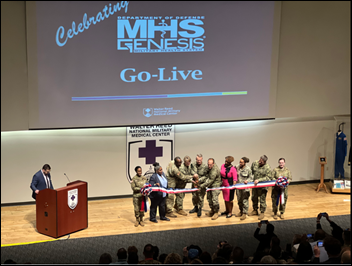
DoD will complete its Oracle Cerner deployment in March 2024, with 75% of its hospitals and clinics already live and most of the remaining sites being overseas facilities. A DoD official says the VA is where DoD was in the 2017-2018 timeframe, with challenges in infrastructure, governance, and standardizing workflows.

VA OIG says that a doctor at North Las Vegas VA Medical Center falsified patient blood pressure readings during virtual visits, always entering them as 120/80. The unnamed physician says they thought the virtual visit template required entry of a phony number and added that they had not been given virtual visit training, both of which OIG says are false. OIG also noted that the hospital didn’t report the physician to the state licensing board and falsely claimed that it had reviewed the 120/80 entries as OIG had requested.
New FDA guidance requires medical device manufacturers to submit a cybersecurity plan as part of their new product application, spelling out how they will monitor and fix newly discovered vulnerabilities. The guidance applies to any medical device that is connected to the internet.
A federal judge in Texas rules that an Affordable Care Act requirement that insurers cover some preventive services at no cost to the patient is not valid, a decision that applies nationwide.
Other
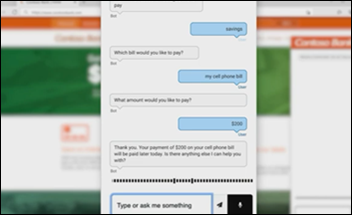
IBM Watson Health doesn’t get mentioned much these days other than as a cautionary tale for overhyping and underdelivering, but I see that IBM is now pitching IBM Watson Assistant for developing virtual agents using its conversational AI.

Walter Reed National Military Medical Center names facility dog and Hospital Corpsman 2nd Class Luke as an honorary super user for MHS Genesis, where he has attended training sessions and sign-on fairs.
Sponsor Updates
- King Faisal Specialist Hospital and Research Centre expands its use of Oracle Cerner solutions across the Saudi healthcare sector.
- Five9 announces GA of Agent Assist 2.0, which uses OpenAI to summarize customer call transcripts in seconds.
- Fortified Health Security names Brad Arnold (Wellpath) security analyst.
- Healthcare Triangle reports fourth quarter and full year 2022 results.
- Health Data Movers publishes a new case study, “Software Development Advisory for an Integrated Experience Layer (IEL) Solution Discovery.”
- InterSystems releases a new episode of its Healthy Data Podcast, “Standards, Access & Meaningful Use of Data (ft. Zafar Chaudry, Seattle Children’s).”
- Medicomp Systems releases a new Tell Me Where It Hurts Podcast featuring HSBlox COO Lynn Carroll.
- Moving to Meditech Expanse has enabled St. Luke’s Health System to implement Meditech’s Smart Pump Infusion Integration with its Baxter Spectrum IQ infusion system.
Blog Posts
- Reducing No-shows Through Simple Patient Engagement Strategies (EClinicalWorks)
- An Urgent Care Business Plan – How and Why for Startups (Experity)
- Blueprint for the Contact Center: A New Path for IT Professionals (Five9)
- Future of Healthcare Supply Chains: An In-Depth Analysis (GHX)
- 3 Ways to Optimize Your Experience at HIMSS Global Conference (Healthjump)
- Engaging Minority Populations with Health Education (Healthwise)
- The Importance of New Types of Strategic Partnerships to Drive Innovation (Impact Advisors)
- Making bank or bankrolling waste: Why surgical schedulers need healthy dictionaries (Intelligent Medical Objects)
- Overcoming Staffing Shortages in the Lab: Finding the Right Fit Consulting Firm (JTG Consulting Group)
- The Many Digital Doors of Patient Access and Engagement (Kyruus)
- Marble Data Connections – Access Hundreds of Millions of Records from Our Network (Marble)
- The Importance of Interoperability in Addressing Healthcare Disparities (Medhost)
- Hate Being Off the Grid? Offline Functionality Provides Vital Wound Care Workflow Continuity for Home Care Providers (Net Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.














































































































































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…