News 3/16/22
Top News

Health data integration company Lyniate will acquire patient identity management vendor NextGate for an undisclosed sum.
HIStalk Announcements and Requests
Mr. HIStalk and Dr. Jayne are busy in HIMSS-land while I hold down the fort at the virtual HIStalk hacienda. Hopefully, Mr. H has finally made it through the registration and badge pick-up line, which, based on his tweet from earlier today, doesn’t seem likely. In lieu of show-floor convos with our wonderful readers that typically involve attempts to get me to divulge Mr. H’s true identity, I’ll instead reminisce about past HIStalkapaloozas. (Is there a better party band than Party on the Moon?) I’m still saddened by the fact that my footwear over the years earned me no HIStalk accolades, though I like to think it did help me make my case for joining the team nearly eight years ago. Help me stay busy this week by emailing me any health IT news you’re afraid might get lost in the #HIMSSanity.
Webinars
April 6 (Wednesday) 1 ET. “19 Massive Best Practices We’ve Learned from 4 Million Telehealth Visits.” Sponsor: Mend. Presenter: Matt McBride, MBA, founder, president, and CEO, Mend. Virtual visits have graduated from a quickly implemented technical novelty to a key healthcare strategy. The challenge now is to define how telehealth can work seamlessly with in-person visits. This webinar will address patient satisfaction, reducing no-show rates to single digits, and using technology to make telehealth easy to use and accessible for all patients. The presenter will share best practices that have been gleaned from millions of telehealth visits and how they have been incorporated into a leading telemedicine and AI-powered patient engagement platform.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

OptimizeRx acquires EvinceMed, a Las Vegas-based company that automates specialty pharmacy transactions.
Avant-garde Health, which offers analytics for surgical and procedure-based care, raises $12 million in a Series A funding round.
Komodo Health will reportedly go public this summer. The offers de-identified patient data and analytics, has raised $314 million, and earned a $3.3 billion valuation.

Precision medicine and clinical dataset vendor Prenosis secures funding from Pace Healthcare Capital, bringing its total raised to over $20 million.
Healthcare payment analytics company Clarify Health acquires Embedded Healthcare, an analytics vendor focused on changing provider behavior to encourage value-based care. The acquisition comes a year after Clarify raised $115 million in a Series C funding round, and six months after its acquisition of Apervita’s value optimization business.

Drug knowledge and decision support company First Databank launches the Vela e-prescribing network, giving prescribers, payers, and pharmacies an additional industry option for medication eligibility and benefits information. FDB partnered with RxRevu and RxLightning to offer real-time pharmacy benefits and specialty prescription enrollment and processing functionalities as part of the new network.
Sales
- EMC Healthcare in Indonesia will implement the InterSystems TrakCare EHR across its six hospitals.
People

Kevin Schweikert (Veradigm/Allscripts) joins Cota as VP of life sciences.
Announcements and Implementations

Clinical Architecture announces GA of SeekDX, a diagnosis search and documentation tool; and Nomad, a fully managed interoperability and data normalization solution designed to help organizations comply with the 21st Century Cures Act.
Leidos will integrate Clearsense’s health data archiving and management capabilities with its managed services offerings.
Caregility announces GA of its subscription-based Inpatient Virtual Engagement service, comprising an administration portal, access point of care system, and management tool for telehealth devices.
Cape Cod Healthcare (MA) will use $1.5 million in federal funding to connect 90 providers from independent practices and community health centers to its Epic system.

InterSystems releases a cloud-based version of its HealthShare Health Connect integration engine.
Consensus Cloud Solutions develops NLP- and AI-based technology that enables providers to convert unstructured clinical content into usable data for improved decision-making.
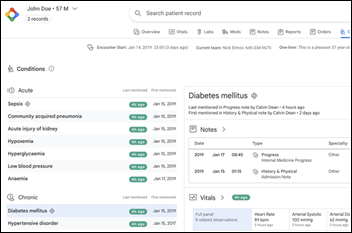
Meditech will pilot the FHIR-enabled integration of Google’s search and summarization capabilities within its Expanse EHR.
Main Line Health (PA) enhances its website with Yext’s Find-a-Doc search tool and Stericycle’s appointment-booking software.
Philips announces GA of cloud-based, interoperable, enterprise imaging technology, and performance analytics for radiology and cardiology.

Kootenai Health in Idaho has replaced 11 EHR systems with Epic.
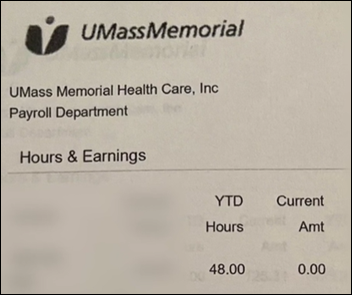
Privacy and Security
Registered nurses file a class action lawsuit against their employer, University of Massachusetts Memorial Medical Center, for allegedly depriving them of accurate wages after last December’s Kronos data breach. The cyberattack on the payroll vendor led to a payment freeze for all UMass Memorial hourly workers, resulting in inaccurate or unpaid paychecks. The suit seems to be separate from a similar filing by RNs initiated in January. Update: UMass Memorial Health EVP and CFO Sergio Melgar clarifies that, “To avoid disruption during the Kronos issue, we used the previous week as a base for pay in order to provide our caregivers with some wages. We did not freeze wages nor miss a pay period. We communicated with our caregivers that their pay might not be accurate at the time, but that we planned to go back and adjust as we worked through this national issue.”
Other

Caledonia Health Center Office Team Lead Cassie Baker and Office Manager Amy DeGood win first place in the University of Michigan Health-West’s inaugural Big Pitch competition for their idea to use Nuance’s AI-powered documentation software to develop an automated prescription messaging and approval process for patients.

Apple’s latest Iphone software update enables masked Face ID users to unlock their phones.
Sponsor Updates
- Surescripts has expanded its specialty medications solutions to enable more prescribers, pharmacists, and patients to benefit from the accelerated speed to therapy supported by these innovations.
- Availity will donate $25,000 to the UN Refugee Agency to help Ukrainian refugees, and will offer to match up to the same amount on behalf of associates who donate.
- Bluestream Health joins the N50 Project to provide virtual care and telehealth services to marginalized communities around the globe.
- Change Healthcare expands its relationship with AWS to accelerate healthcare transformation.
- Olive and NTT DATA will co-develop new Loops – applications that work on Olive’s platform to provide real-time intelligence – and new machine learning and robotic process automation (RPA) models, initially focusing on improving supply chain and IT efficiencies.
- CoverMyMeds signs on as the first employer partner in Fortuity’s Pathways Workforce Development program, which helps prepare highly qualified candidates for call center employment with local businesses.
- Elsevier Clinical Solutions publishes “Clinician of the Future: a 2022 report.”
End users give the following HIStalk sponsors top user satisfaction marks, according to a Black Book survey of specialty practices:
- Netsmart (behavioral and mental health, home health large agency & hospice, psychiatry)
- Cerner (colon and rectal surgery, general surgery, internal medicine, pediatric surgery)
- WebPT (physical therapy & rehab)
Blog Posts
- Drive Patient Volume Through Always on Automation (Actium Health)
- A Brief Introduction to Azara’s Master Patient Index (MPI) (Azara Healthcare)
- Re-Imagining Health at HIMSS: Bamboo Health Fosters Interoperable Care Coordination to Improve Physical and Behavioral Healthcare (Bamboo Health)
- EHR Change Management Tips That Help Overcome Reluctance (CereCore)
- How an open EHR advances usability for healthcare providers (Cerner)
- Opioid Prescriptions Decrease After EPrescription Mandate (ChartLogic)
- The Evolving Role of OCR and the Changing Face of HIPAA Enforcement Penalties (Clearwater)
- The Air Force Core Values: A Foundation for Optimizing Perinatal Care (OBIX Perinatal Data System, developed by Clinical Computer Systems)
- What has 1 Amazing Story and 7 Storytellers Stacked 2 Stories High? (EVisit)
- Patient-centered payments are the key to faster collections (Experian Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.













































































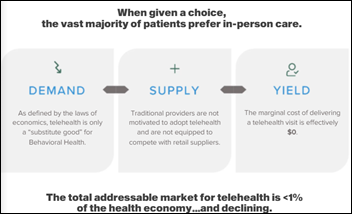









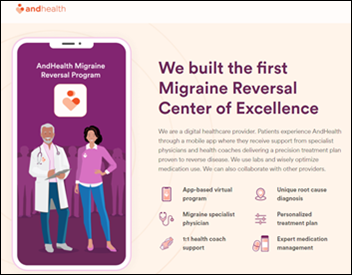


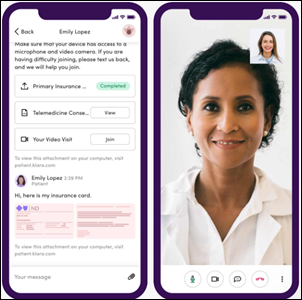










Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…