Download a PDF version of this document here.

3M Health Information Systems
Booth 3334
Contact: Jolie Gordon, Marketing Communication Specialist
jegordon@mmm.com 801-560-4788

Best known for our market-leading coding system and ICD-10 expertise, 3M Health Information Systems delivers innovative software and consulting services designed to raise the bar for clinical documentation improvement, computer-assisted coding, mobile physician applications, case mix and quality outcomes reporting, and document management. Our robust healthcare data dictionary and terminology services also support the expansion and accuracy of your electronic health record (EHR) system. With nearly 30 years of healthcare industry experience and the know-how of more than 100 credentialed 3M coding experts, 3M is the go-to choice for 5,000+ hospitals worldwide that want to improve quality and financial performance.

Access
Booth 860
Contact: Cody Strate, Director of Sales
cody.strate@accessefm.com
303.257.3183

Access is the world’s leading electronic forms (e-forms) management, automation and workflow software provider. Our solutions transform any paper-intensive forms process into a paperless, collaborative one. Stop by HIMSS Booth 860 to see how Access can help you achieve paperless:
- Registration and consent forms on demand with electronic signatures & barcodes
- Human resources, financials and clinical processes, including new employee onboarding, capital requests, and physician referrals
- Clinical data bridge to your enterprise content management system
Learn more at www.accessefm.com.
Advisory Board Company
Booth 7310

Contact: Leah Bruch, Senior Manager Strategic Marketing
bruchl@advisory.com
202.266.6775

The Advisory Board Company is a global research, consulting, and technology firm partnering with 125,000 leaders in 3,200 organizations across health care and higher education. Through our innovative membership model, we collaborate with executives and their teams to elevate performance and solve their most pressing challenges. We provide strategic guidance, actionable insights, web-based software solutions, and comprehensive implementation and management services.
Learn more at www.advisory.com.

AirStrip Technologies, Inc.
Booth 870
Contact: Kimberly Kuzawa, Executive Assistant
Kimberlykuzawa@airstriptech.com
832.330.4419

Native applications from AirStrip Technologies securely send critical patient information from hospital monitoring systems, bedside devices, electronic health records and home devices to a clinician’s smartphone or tablet. FDA cleared, CE Mark certified and designed to meet HIPAA security requirements, AirStrip applications are powered over wired and wireless networks, delivering live patient data anytime, anywhere.

ANX
Booth 13429
Contact: Mike Nunez, Director, Healthcare Business Development
nunezm@anx.com
806.797.2923
ANXeBusiness provides innovative solutions that transform the exchange of data throughout the entire healthcare community. This solution set creates an easy, reproducible, cost efficient and secure exchange between hospitals and laboratories. This allows the hospital and laboratory to focus on what they do best; the complete patient continuum of care. To learn more about ANXeBusiness, please visit us at www.anx.com.

API Healthcare
Booth 2617
Contact: Kenny Amburgey, Vice President of Client Strategies
kenny.amburgey@apihealthcare.com
262.385.7732

Solutions designed for the unique demands of the healthcare industry. API Healthcare solutions create the crucial link that allows you to effectively balance the financial realities of healthcare with the delivery of high quality patient care. Robust integration and data driven staffing tools are what make API Healthcare workforce management solutions powerful:
- Fully integrated, single platform technology
- Complete multi-dimensional insight into all areas of an organization allow for intuitive, cost effective decisions
- Data driven staffing tools ensure the right patient and the right caregiver match, every time
- Streamlines processes, increases efficiency and optimizes every aspect of your workforce

Aspen Advisors
To schedule a meeting:
Contact: Daniel Herman, Managing Principal and Founder
info@aspenadvisors.net
800-697-4350

Aspen Advisors is a professional services firm with a rich mix of respected industry veterans and rising stars who are united by a commitment to excellence and ongoing dedication to healthcare. Our experienced team is highly skilled in all aspects of healthcare technology. We understand the complexities of healthcare operational processes, the vendor landscape, the political realities, and the importance of projects that are executed successfully – the first time. Every client is important to us, and every project is critical to our reputation. Established in 2006, we’ve grown significantly year-over-year and have earned accolades for our culture and growth.
We were named an “Up and Comer” by Healthcare Informatics in 2010 and ranked #20 in Modern Healthcare’s list of the top 100 “Best Places to Work in Healthcare” in 2011. Our hallmarks are top quality service and satisfied clients; we’re proud of our KLAS rankings and that each of our clients is 100% referenceable. For the last four consecutive years, Aspen has ranked in the Top 5 in KLAS’ “Best in KLAS Awards” report in the Planning and Assessment category and were included in the Top 20 in the Clinical Implementation Supportive market segment. Interested in learning more about how Aspen Advisors can help you address the issues on your top priority list? Or looking to join a firm where healthcare IT consultants aren’t commodities, communication isn’t curbed, and potential never gets stuck in a pigeon hole?
To learn more about Aspen Advisors – either as a prospective client or prospective associate, please consider scheduling an in-person meeting at HIMSS or visit us at http://www.aspenadvisors.net.

AT&T
Booth 3829
Contact: Deborah Sunday Marketing Director
ds823e@att.com
678.230.3440
AT&T ForHealth℠ is committed to serving the technology needs across the continuum of care — from hospitals to physicians to patients. Our suite of innovative wireless, cloud-based and networking services and applications empower clinicians by placing vital patient health information at their fingertips. Learn how to rethink healthcare delivery by visiting AT&T ForHealth in Booth #3829 at HIMSS12 in Las Vegas. Also, be sure to visit and hear AT&T speakers in the HIMSS Knowledge Centers for Mobile Health (#12928, Hall G, Kiosk 14 ), Cloud Computing (#13624, Hall G, Kiosk 5) and Accountable Care Organizations/Value-Based Purchasing (#6466, Hall D, Kiosk 8)

Aventura
Booth 8300
Contact: Brian Stern, VP of Sales
info@aventurahq.com
888.484.4643

Aventura improves the current workflow of doctors and nurses. We give clinicians the information they need, when and where they need it. Our context aware computing intelligence orchestrates technologies already in place making them responsive to the user. The result is improved clinician satisfaction, increased EMR use at the point of care, and an increased focus on the quality of care.

Awarepoint Corporation
Booth 3412
Contact: Merrie Wallace, Executive Vice President, Product Solutions and Marketing
marketing@awarepoint.com
888.860.3463

Awarepoint’s aware360Suite provides intelligent workflow solutions that meet departmental and enterprise-wide patient tracking needs. The solution visualizes patient flow without requiring personnel to manually update care status information. Patient location, movement and interactions with tagged personnel and clinical equipment trigger updates to the web-based software, which employs workflow rules to recognize patient care milestones. By improving patient visibility throughout the enterprise, Awarepoint helps administrators and clinicians to advance the QUALITY of care, the EFFICIENCY of care, the EXPERIENCE of care, and the ECONOMICS of care.

Beacon Partners
Booth 3926
Contact: Katelyn MacKay, Business Development Coordinator
kmackay@beaconpartners.com
781.681.7407
As one of the largest healthcare management consulting firms, Beacon Partners is chosen by organizations in the healthcare community to provide advisory services to improve overall operational, clinical and financial performance with the adoption of information technology. With our strategic approach and depth of experience, Beacon Partners is qualified to help organizations navigate the challenges in healthcare and optimize their potential to deliver the highest possible level of patient care.

BESLER Consulting
To schedule a meeting:
Contact: Jim Hoffman, Chief Technology Officer
jhoffman@besler.com
732.392.8214
Available at HIMSS Tuesday or Wednesday
BESLER develops software tools and provides consulting services that help acute care hospitals get paid everything they deserve. Our BVerified ™ online solutions allow our customers to manage underpayment recoveries that have traditionally been accomplished via a consulting engagement, providing typical saving of 50%. We’ve just launched our two newest products and we’re the only company with an end-user technology solution to address the Medicare IME and Transfer DRG underpayment issues.

Billian’s HealthDATA
Booth 7707
Contact: Jennifer Dennard, Social Marketing Director
jdennard@billian.com
678.569.4872
Billian’s HealthDATA is the leading provider of comprehensive market intelligence on the healthcare industry, covering facilities across the continuum of care – from Hospitals and Hospital-Affiliated Physicians to Long Term Care. Billian’s dedication to providing high-quality data via products like the Portal, coupled with partner company Porter Research’s custom market research services, provides customers with healthcare business intelligence about multiple markets in scaleable formats

Bottomline Technologies
Booth 12928 (Mobile Health Knowledge Center, Hall G)
Contact: Sarah Stevenson, Healthcare Marketing Manager
sstevenson@bottomline.com
603.380.8577

For more than 20 years, Bottomline has been focused on software applications that optimize document-driven processes. As a result, Bottomline possesses both the proven solutions and the tested domain expertise to deliver consistent customer value and significant return on investment. Bottomline’s medical forms solutions are used by 900+ hospitals to reduce costs, increase productivity & improve patient safety. Our goal is to help hospitals, clinics and practices adopt electronic medical records – from registration and consents to clinical documentation – an evolution that has been plagued by counter-intuitive approaches that aren’t as flexible and fast as paper.

CAP Professional Services
To schedule a meeting:
Contact: Chip Perkins, Managing Director
cperkins@cap.org
847.832.7280
CAP Professional Services, a division of the College of American Pathologists, works to align health care information and technology to drive performance and quality. We are advancing health information excellence by focusing on services such as: Health Information Strategies and Management, Clinical Data and Terminology Services, and Laboratory Services. For more information, call 847-832-7700 or email capsts@cap.org.

CapSite
To schedule a meeting:
Contact: Bryan Fiekers, Director of Business Development
bryan.fiekers@capsite.com
802.383.8205
CapSite is a healthcare technology research and advisory firm. Our mission is to help healthcare providers and vendors make more informed strategic decisions.The CapSite Database is the trusted, easy to use online database, providing critical knowledge and evidence based information on healthcare technology purchases. CapSite™ data provides detailed transparency on healthcare technology pricing, packaging and positioning.When it all comes to healthcare technology research, it helps to see all the details. Those details are now available with CapSite™

Capsule Tech, Inc
Main Booth 6141
HIMSS Intelligent Hospital Pavilion Booth 12442
Interoperability Showcase Booth 11000
Medical Devices Integration Knowledge Center Booth 14647
Contact: Heather Hitchcock, Vice President of Global Marketing
marketing@capsuletech.com
978.482.2337

Capsule is the leading provider of medical device integration. Capsule’s Device Connectivity Solution is the most proven, vendor neutral solution available for device connectivity. It features a patient-centric design that is completely flexible and scalable and integrates with existing technologies and clinical workflows. Stop by our booth 6141 to see why over 1000 hospitals have chosen Capsule for device integration.

Care360
Booth 2813
Contact: Joel Williams, Associate Director-Sales Support and Operations
Info@Care360.com
www.Care360.com
888.835.3409

Racing to Expand Your Physician Community? Accelerate your competitive advantage by joining our existing Care360 network of more than 200,000 physicians in 80,000 physician offices. Care360® EHR is a certified EHR solution that can be up and running in as little as 30 days, allowing physicians to transition workflow from paper to electronic management in a modular approach. Care360 EHR with Data Exchange connects hospitals to physician practices with a web-based platform to share information. ChartMaxx® DMI/ECM enables healthcare organizations to see immediate improvements through electronic document and content management, eForms and automated workflows that cross existing sytems. To learn more, visit Care360.com

Certify Data Systems, Inc.
Booth 5934
Contact: David Caldwell, Executive Vice President
sales@certifydatasystems.com
713.446.3376
Certify Data Systems, Inc., is a pioneer in health information exchange (HIE) technology. The company’s Enterprise HIE Platform has been adopted by the nation’s leading hospitals and health systems. The bi-directional HIE platform, provides true interoperability between disparate Electronic Health Record (EHR) systems, enabling hospitals and health systems, their affiliated physician practices and laboratories to exchange essential health information in real-time without changing workflow. Moreover, Certify’s “network approach” is easy to deploy, scale, manage and support. For more information, please visit http://www.certifydatasystems.com. Follow us on Twitter at @CertifyData.
Command Health
To schedule a meeting:
Contact:
Evan Frankel, Director of Product Management
evan.frankel@commandhealth.com
303.301.0430

Command Health is the leader of narrative note technology, focusing on unifying clinical documentation from disparate sources across the continuum of care. Combining verbal interaction with visual integration, Command Health enables the efficient and accurate capture of patient data that is easy to find, use, share and search by converting locked, inaccessible data into actionable, meaningful information. Using proprietary natural language processing (NLP) technology combined with human intelligence, Command Health delivers the most comprehensive clinical data available, helping providers reduce costs, assess risk and manage outcomes.

CTG Health Solutions
Booth 2070
Contact: Carl Ferguson, Jr., Managing Director
carl.ferguson@ctghs.com
214.695.4227
CTG Health Solutions is a leading healthcare IT consulting firm providing strategic, clinical, financial, operational, and technology solutions. Offering advisory services, strategic/tactical planning, vendor selection, implementation, legacy system support, program/project management and advance technology services, CTG helps healthcare organizations address regulatory mandates of meaningful use, 5010, ICD-10, HIE, electronic medical records, accountable care and evolving health reform. CTG Health Solutions is a business unit of CTG (NASDAQ: CTGX) a publicly owned IT services and solutions company founded in 1966 that generated revenue of $331 million in 2010. More information is available at www.ctghs.com.
Experience matters. Over the last 25 years, CTG Health Solutions has provided healthcare IT, and operational and strategic consulting support to over 600 healthcare organizations. Since 2008, CTG has continuously been named to Healthcare Informatics top 100 healthcare IT providers and the Modern Healthcare lists of the largest healthcare management consulting firms. CTG was also cited in the March 25, 2010, issue of Information Week as one of the top three firms for healthcare organizations looking for help in implementing EMRs and other health IT investments.

Cumberland Consulting Group
Booth 5147
Contact: Jim Lewis, Managing Partner
jim.lewis@cumberlandcg.com
615.373.4470

Cumberland Consulting Group is a national technology implementation and project management firm serving ambulatory, acute, and post-acute healthcare providers. Through the implementation of new technologies, Cumberland works with providers to advance the quality of care delivered, and improve business performance. Cumberland Consulting Group offers an invigorating, positive work environment and a commitment to superior talent acquisition, development and retention.Cumberland was named Best in KLAS for IT Planning & Assessment in the 2011 Best in KLAS Awards: Software & Services report, finishing in a first-place tie.
Cumberland Consulting Group Says: Stop by and meet some of our top implementation consultants and learn about Cumberland’s excellent delivery record, straightforward implementation methods and lean operating model that delivers big company results at a very attractive price. Be sure to catch Cumberland’s Erik Howell presenting Physician-to-Physician: Driving Inpatient CPOE Clinical Transformation, Session 184,Thursday Feb. 23 at 2:15pm.

CynergisTek
To schedule a meeting:
Contact: Stephanie Crabb, VP of Client Services
stephanie.crabb@cynergistek.com
512.402.8550 or 954.298.4702
CynergisTek is an authority in healthcare information security management services and solutions. We assist hospitals, payers, vendors and other valued business partners to the healthcare industry with the development and management of standards-based, industry-appropriate, business-driven and compliance-aware information security programs. CynergisTek is a full-service firm offering solutions in the areas of strategy and governance, compliance and risk, technical security management, managed security solutions and partner technology resales and implementation. CynergisTek was chosen to provide advisory and consulting services throughout the organization’s audit experience by one of the first 20 entities targeted by OCR for its HIPAA Audit Program. CynergisTek has led dozens of risk assessment projects for organizations attesting for Meaningful Use. CynergisTek has established its Surveyor program to provide critical third-party review of business associate compliance with HIPAA and to support organizations with independent review of IT security performance as part of their M&A due diligence activities. CynergisTek has led dozens of data discovery and data loss breach risk assessments to help organizations identify where PHI/PII reside in their organizations and how that data is being handled.
CynergisTek is working on the front lines, side-by-side, with our clients to address the most pressing IT security, privacy and data governance challenges. We are visionary. We are practical. We make our clients better.

DrFirst, Inc.
Booth 5456
Contact: Timur Tugberk, Events, Brand, and Media Coordinator
ttugberk@drfirst.com
301.231.9510 ex. 2835
Founded in 2000, DrFirst is the nation’s leading e-prescribing and solutions platform provider to physician practices, major health plans, health systems, hospitals, and EHR vendors. Through its Open Borders Program, DrFirst solutions integrate with over 200 EHR, practice management and HIT systems. A Surescripts Gold Certified solution provider for four consecutive years with its award-winning Rcopia electronic prescription management system, DrFirst utilizes the Surescripts network for pharmacy connectivity, health plan information, and patient medication history. For more information, visit www.drfirst.com.

eClinicalWorks
Booth 531
Contact: Heather Caouette, Marketing
heather.c@eclinicalworks.com
508.836.2700
eClinicalWorks offers ambulatory clinical solutions consisting of EMR/PM software, patient portals and a community health records application. With more than 180,000 providers and 370,000 healthcare professionals across all 50 states using its solutions, customers include physician practices, out-patient departments of hospitals, health centers, departments of health and convenient care clinics. At HIMSS, please visit the eClinicalWorks booth to see the latest in iPad and patient applications, community analytics and ACO capabilities.

Elumin Healthcare Solutions
To schedule a meeting:
Contact: Mark Williams, CEO & President
mwilliams@eluminhs.com
425.369.8211
Elumin works with healthcare organizations across the country to improve quality, efficiency and their bottom line through the use of information technology throughout the continuum of care. Our work ultimately leads to greater clinician, physician, staff and patient satisfaction. Many of Elumin’s consultants are clinicians, and many have worked in hospitals and physician practices as business and clinical leaders. Many are certified and experienced in premier technologies such as Allscripts, Epic, Cerner, NextGen and Siemens. On average, our consultants have more than 15 years of experience. We strive to achieve 100% referenceability among our clients. Elumin is 100% focused on healthcare.
Elumins services include: advisory services, system implementations, data conversions, clinical optimization, revenue cycle management, legacy platform support, ICD-10, 5010 migration, and interim staffing. Our team of experienced healthcare professionals thrives on implementing best practices, optimizing technology and guiding clients through the change management process.
Elumin representatives will be attending the 2012 HIMSS conference Monday Feb. 20 – Friday, Feb. 24. They look forward to meeting new healthcare industry leaders and sharing insight on trending topics. Let us help you bring light to the best of healthcare technologies’ promise.

Encore Health Resources
Booth 123
Contact: Randi Fiedler, Director, Sales Operations
rfiedler@encorehealthresources.com
832.289.0923
Encore Health Resources helps implement and optimize EHRs and complex clinical systems to get value from the data. We do this through our tools, knowledge base and proprietary approach, and by employing healthcare IT professionals with deep operational experience.
Encore was formed by healthcare IT veterans Dana Sellers and Ivo Nelson. We are one of the fastest growing independent consulting firms in the history of our industry. That rapid growth is attributed to our principles’ sterling reputation, our staff’s depth of experience, and our commitment to remaining 100% referenceable with each and every one of our clients. Encore has consistently been named one of the “Best Places to Work in Healthcare” by Modern Healthcare magazine.
ESD
Booth 4616
Contact: Jessica St. John, Director of Business Development
jstjohn@contactesd.com
419.841.3179
ESD is a leading healthcare IT consulting firm that assists organizations implement new or updated heathcare information technology. Experienced clinical consultants provided by ESD work closely with hospitals, clinics and health systems to evaluate current capabilities, establish clinical transformation strategies and assist clinicians in the transition to new or updated solutions, with the end goal being a successful transition to new technology. ESD’s headquarters is located in Toledo, Ohio and has five satellite offices located in Atlanta, Detroit, Cincinnati, New York and Houston.
Whether it’s time to implement a whole new system throughout your organization or just a component to one department, we have the experience and resources to both complement your team, and meet your goals.

Etransmedia Technology, Inc
Booth 13635
Contact: Craig Cane,VP, Business Development
craig@etransmedia.com
845.594.7247

Etransmedia Technology, Inc is a premier provider of information solutions to the healthcare industry, delivering comprehensive integrated software, service and connectivity solutions to simplify critical functions in the healthcare community. Etransmedia is committed to providing the right solutions to build an effective community of care, driving revenues and efficiencies for ambulatory, acute and diagnostic facilities, and increasing the availability of information to providers making critical care decisions.

First Databank (FDB)
Booth 2338
Contact: Denise Apcar, Brand Communications Manager
dapcar@fdbhealth.com
800.633.3453
First Databank (FDB) provides drug knowledge that helps healthcare professionals make precise medication-related decisions. With thousands of customers worldwide, FDB enables our information system developer partners to deliver a wide range of valuable, useful, and differentiated solutions. As the company that virtually launched the medication decision support category, we offer more than three decades of experience in transforming drug knowledge into actionable, targeted, and effective solutions that improve patient safety and healthcare outcomes. For a complete look at our solutions and services please visit fdbhealth.com

Fulcrum Methods
Booth 13247 Kiosk 6
Contact: Rick Beberman, Corporate Programs
rbeberman@fulcrummethods.com
510.287.3927

Fulcrum Methods has developed toolkits to assist hospitals and health systems with project management and meaningful use. We deliver work plans, guidebooks, libraries of deliverables, and online assessment tools to help organizations with vendor selection, systems implementation, long-range planning, establishing a program management office, managing organizational change, and meeting meaningful use requirements.
We have a great client list – Stanford University Hospital & Clinics, Lucile Packard Children’s Hospital, University Hospitals, MaineHealth, University of Kentucky HealthCare, John Muir Health, Community Medical Centers, and NorthBay Healthcare, among others. Our tools are encyclopedias of best practices and designed to develop core competencies, reduce execution risk, accelerate project rollout, and keep organization knowledge in-house.

GetWellNetwork
Booth 7910
Contact: Tony Cook, Vice President Marketing
tcook@getwellnetwork.com
202-321-9396
GetWellNetwork entertains, educates, and empowers patients throughout the patient journey using the bedside TV in the hospital, mobile devices, Web or Cable TV at home. Our patient-centered approach improves both satisfaction and outcomes for patients and hospitals. Additionally, the company extends the value of existing IT investments by integrating seamlessly to leading HIT systems including Cerner, McKesson, Epic, Meditech, GE and Siemens.
GetWellNetwork is recognized by KLAS® as the leader in Interactive Patient Systems and is exclusively endorsed by the American Hospital Association. More information about GetWellNetwork can be found at www.GetWellNetwork.com.

Harris Corporation
Booth 834
Contact: Amy Ferretti, Vice President, Marketing
amy.ferretti@harris.com
925.518.9895
Harris is advancing healthcare for more than 300,000 users at over 2,000 provider organizations delivering care to nearly 13,000,000 patients – by delivering proven solutions that enable healthcare organizations to constantly improve quality of care while containing costs, increasing revenue, and addressing the new world of accountability and value. We provide a portfolio of solutions that promote interoperability, streamlined workflow, and analytics; all of which are adaptable to our customer’s specific care delivery setting and the unique requirements of their physical, technical, and user environments.
- Health Information Exchange
- Patient Portal
- Provider Portal
- Business Intelligence
- Workflow Management
- Image Management
- Managed Services
- Systems Integration Communications

Hayes Management Consulting
To schedule a meeting:
Contact: Bill Gannon, Director
bgannon@hayesmanagement.com
541.647.0825

Hayes Management Consulting is currently helping clients prepare for Meaningful Use, ICD-10 migration, and other initiatives by providing strategic guidance and hands-on expertise in EHR system implementation and optimization, project management, project resources and more.

Healthwise
Booth 4627
Contact: Dave Mink, Account Executive
dmink@healthwise.org
208.331.6971

Healthwise leads the way with ONC–ATCB-certified patient education that contributes to improved care quality. Helping hospitals meet Meaningful Use criteria today, and tomorrow’s ACO goals, the Healthwise Patient Education Solution seamlessly integrates into EMRs, PHRs, and websites. Ask about our new shared decision-making tools and patient response. www.healthwise.org.

Holon Solutions
Booth 12214
Contact: Sandra Schafer, Vice President of Marketing and Business Development
sschafer@holonsolutions.com
678.324.2039

At Holon we believe that collaboration improves lives. Holon’s CollaborNet™ facilitates collaboration among healthcare providers by creating secure networks that manage the assembly, packaging, routing and delivery of vital health information. Holon’s CollaborNet connects providers regardless of their level of technological sophistication, using the systems in place and with or without standard communication protocols. CollaborNet is flexible and adaptable and can support changes to communication standards and methods as they develop. CollaborNet builds value from the bottom up by delivering information WHEN, WHERE and HOW you need it. For more information please visit us at www.HolonSolutions.com.

Iatric Systems, Inc.
Booth 7905
Contact: Judy Volker
Judy.Volker@iatric.com
978.805.3191

If you’re attending HIMSS12 to find ways to get the most out of your HIS, be sure to visit Iatric Systems booth. There you’ll learn about solutions that can be integrated with your HIS in order to help you achieve interoperability, meet Meaningful Use objectives and support your ACO initiatives.
Recognized by Inc. 5000 as one of the fastest growing privately held companies for the past four years, Iatric Systems helps hospitals and health systems leverage their HIS investment with software, interfaces and reporting services. Since 1990, more than 1,000 hospitals worldwide have implemented Iatric Systems solutions; optimizing patient care and staff workflow in clinical, financial and administrative areas. Iatric Systems was acknowledged on the Healthcare Informatics Top 100 Healthcare IT Revenue list in 2009/2010/2011 and the Modern Healthcare Top 100 Best Places to Work in Healthcare IT in 2009/2010/2011.
Get your chance to win an iPad 2 during the HIStalk Booth Crawl: Be sure to stop at the Iatric Systems booth for the chance to win the perfect, portable tool for checking e-mail, surfing the Web, playing games, reading books and visiting important Websites like Iatric.com.

ICA
Booth 4831
Contact: John Tempesco, CMO
john.tempesco@icainformatics.com
615.866.1465

ICA’s CareAlign® care management solutions connect the healthcare community with proven interoperability technologies enabling health information exchange and improved care delivery. This patient-centered modular approach offers immediate value and return-on-investment to communities, IDNs, hospitals and physicians through the delivery of clinical information to the point-of-care improving quality while reducing costs. Visit booth #4831 for a demonstration of the CareAlign solution suite.

iMDsoft
Booth 4215
Contact: Steve Sperrazza, Vice President, North America Sales
sales@imd-soft.com
866.4 iMDsoft, 781.449.5567
iMDsoft is a leading provider of Clinical Information Systems for critical and perioperative care. The company’s flagship family of solutions, the MetaVision Suite, was first implemented in 1999. It captures, documents, analyzes, reports and stores the vast amount of patient-related data generated in a hospital. Over 125 hospitals worldwide use MetaVision to support their workflow, and arm their healthcare professionals with timely, accurate, and actionable information. iMDsoft products demonstrate 100% implementation success rate and a 100% customer retention rate.
Come visit our booth to find out why 4 of the top 10 US hospitals have decided that MetaVision is the best choice for improving care quality and financial performance. Providing an integrated edge where it matters most, MetaVision delivers high-impact results such as 30% fewer mortalities, 100% billable anesthesia records, total elimination of prescription errors, 99% compliance with PQRS measures and doubled protocol compliance.
Learn more about how MetaVision interoperates with the latest technologies and seamlessly integrates with hospital systems at the HIMSS12 Interoperability Showcase held in collaboration with Integrating the Healthcare Enterprise (IHE), from 21-23 February.

Imprivata
Booth 3160
Contact: Jim Whelan, VP of NA Healthcare Sales
jwhelan@imprivata.com
508.395.2235
Learn directly from hospital CIOs on how they saved their clinicians more than 15 minutes per day and improved workflows with Imprivata OneSign. Hospital CIOs and Directors using Epic, McKesson, Siemens, Meditech and Healthland will be available to answer your questions. After the presentations, you can try a hands-on demo of No Click AccessTM to applications and roaming virtual desktops throughout the Imprivata booth. Imprivata is also raffling off 30 Kindle Fires, which will be raffled off after each theater presentation!

Informatica
Booth 9107
Contact: Jonathan Shafer, Senior Customer Marketing Campaign Manager
jshafer@informatica.com
650.385.5000
Informatica Corporation is the leading independent provider of enterprise data integration software and services. Using Informatica solutions, healthcare organizations can access, discover, cleanse, integrate, and deliver all enterprise data to improve health outcomes, meet compliance mandates, streamline operations, increase agility, and refocus energy on the consumer. More than 4,100 companies worldwide and hundreds of healthcare companies rely on Informatica for their end-to-end enterprise data integration needs.

Ingenious Med
Booth 4663
Contact: Laura DePeters,Marketing Manager
laura.depeters@ingeniousmed.com
404.786.2340

Ingenious Med’s Inpatient Physician Management Platform is the leading charge capture and physician performance solution in the health care industry today. Our cloud-based, charge capture and analytics platform provides real-time data that helps hospital systems and physician groups maximize revenue, improve physician productivity, enhance quality of care, and increase diagnosis and billing accuracy and compliance.

Intelligent Medical Objects Inc.
Booth 1256
Contact: Dennis Carson, Director, Marketing & Tradeshows
dcarson@imo-online.com
636.477.8710

Interoperability For Healthcare Institutions IMO® Vocabulary products provide a common linkage across all electronic patient records, regardless of the standard needed for that particular data set (ICD9-CM, SNOMED® CT, HCPCS, RxNorm, ICD-10-CM). Most code mappings are updated several times per year, including regulatory updates. IMO® removes the burden of managing updates for you. Terminology Mapping For EMR Software Vendors IMO® Vocabulary products let you focus on what you do best: provide great software to the healthcare industry. We furnish up-to-date code and terminology mappings, with expanded search capabilities, across standards needed for EMRs, EHRs and PHRs (ICD9-CM, ICD10-CM, SNOMED® CT, HCPCS, RxNorm). Get ready for ICD-10 now!

Intellect Resources
To schedule a meeting:
Contact: Stowe Blankenship,Business Development Executive
336.790.8724 x 303
sblankenship@intellectresources.com
http://www.facebook.com/IntellectResourcesFan@wespeakHIT

We speak the language of Healthcare IT. Intellect Resources is proud to offer comprehensive consulting, recruiting and hiring solutions within the Healthcare IT market. Our talent offerings include recruiting, project management, implementation, upgrading and optimization of EMR systems, training and go-live support and the revolutionary Big BreakSM hiring process. Big BreakSM is patent-pending American Idol style audition process where candidates compete to become a healthcare IT trainer and instruct healthcare personnel on the use an EMR program. Big Break offers hospitals systems a unique and innovative talent pool at a fraction of the cost of traditional solutions.
For more information visit www.intellectresources.com or www.irbigbreak.com.

Intelligent InSites
Booths 12217, 12442-18
Contact: George Sun, VP of Sales
george.sun@intelligentinsites.com
972.567.2114

Intelligent InSites helps hospitals improve care and reduce costs by transforming automatically-collected data into actionable insights.Through its interoperable, hardware-agnostic, healthcare real-time location system (RTLS) software platform, Intelligent InSites gathers data from real-time location, condition sensing, and other systems; then delivers meaningful information to the right person, at the right time, on the right device.
By leveraging this real-time data and InSites’ applications, such as asset management, patient flow, temperature monitoring, and business intelligence, healthcare organizations are able to achieve meaningful and measurable hard-dollar cost savings while improving patient satisfaction and patient care. The InSites RTLS solution for Patient Flow enables hospitals to improve capacity management and key metrics such as Left Without Treatment (LWOT) and Length of Stay (LOS). It also improves rounding management, along with ED and OR workflow. With the InSites solution, hospitals can monitor patient flow and progress from admission to discharge, analyze throughput and proactively react to potential bottlenecks – all in real-time. The InSites RTLS solution for Asset Management enables hospitals to optimize equipment inventories and equipment procurement, as well as reduce rental expenses. By eliminating time needed to find available equipment, hospitals can increase value-added time for nursing staff, clinical engineering, and facilities management, leading to improved patient and staff satisfaction.The InSites Business Intelligence (BI) solution enables easy-to-use data mining of vast quantities of contextual data stored in the InSites Business Intelligence database, allowing healthcare users to analyze trends, identify process improvement opportunities, and report on Key Performance Indicators (KPIs). This enables hospitals and healthcare systems to achieve powerful and flexible enterprise-wide visibility into their processes and make transformational impacts on their organization’s performance.

iSirona
Booth 12414
Contact: Peter Witonsky,President & CSO
peter.witonsky@isirona.com
610.772.7648

iSirona helps clinicians make more informed decisions about patients by providing an easy to use approach to medical device integration. Using iSirona’s software solution, hospitals can connect virtually any medical device to their CIS, providing clinicians with faster access to more accurate patient information. In 2011, iSirona was ranked #1 by KLAS for medical device integration systems.

Levi, Ray and Shoup, Inc.
To schedule a meeting:
Contact: John Runions, Director, Worldwide Business Development / Alliances
john.runions@lrs.com
217-725-4017. John Runions
Does your hospital struggle with printing issues? For more than three decades, LRS has been helping hospitals meet the need for reliable document delivery of critical healthcare documents. LRS works directly with leading Electronic Medical Records (EMR) software providers to provide a seamless platform for assured delivery of any document from any system — to any destination in your environment. This all managed from a secure central point of control designed to save effort, money and time when seconds count.

Lifepoint Informatics
Booth 153
Contact: Lee Barnard, Chief Business Development Officer
lbarnard@lifepoint.com
201.560.3802

Lifepoint Informatics is a leader in health IT focusing on laboratory outreach connectivity, health information exchange and clinical data interoperability to deliver on its mission to help healthcare providers improve patient care and lower costs through the use of information technology. Since 1999, Lifepoint Informatics has enabled over 200 hospitals, clinical labs and anatomic pathology groups to grow their market share and extend their outreach programs through the deployment of its ONC-ATCB certified Web Provider Portal and its comprehensive portfolio of ready-to-go EMR/EHR interfaces.
For more Information please visit www.lifepoint.com.

Macadamian
To schedule a meeting:
Contact: Didier Thizy, Director of Healthcare IT
didier@macadamian.com
613.219.5708
Macadamian is a global UI design and software innovation studio with significant sector expertise in healthcare and life sciences. We work with Healthcare and medical device companies to create visually stunning, intuitive, and commercially-successful software products. We can help you transform your ideas into market-ready products that will stand out from your competition.

MED3OOO
To schedule a meeting:
Contact: Nicole Contardo, Corporate Marketing Director
Nicole_Contardo@MED3000.com
919.794.5881

Since its founding in 1995, MED3OOO has grown to become a leading provider of healthcare management, operations, and information technology services across the United States. With over 2,100 employees, MED3OOO provides sophisticated management services and innovative technology products which differentiate its physician, hospital, employer, government, and payer clients. The company provides a complete platform of clinical and business performance solutions, including PM, EHR, RCM, population health management, and smart communication systems, along with management, knowledge and operations, and affiliation strategies which help its clients improve clinical and financial outcomes. MED3OOO partners with organizations across the healthcare spectrum who truly understand that Outcomes Matter.

MedAptus
To schedule a meeting:
Contact: Jennifer Crowley, Marketing Director
jcrowley@medaptus.com
617.896.4099

MedAptus is the Gold Standard in the healthcare revenue cycle for achieving effective charge management, compliance and workflow efficiency. With our powerful and easy-to-use Intelligent Charge Capture, many of the nation’s most prestigious healthcare organizations rely on MedAptus for financial optimization. Our solutions increase revenue, enhance EMR investments, re-engineer manual processes and yield substantially improved productivity. For more information about how MedAptus can help you improve your financial performance while helping you prepare for ICD-10, visit www.medaptus.com.

Medicomp Systems
Booth 855
Contact: James Aita, Sr. Product Manager
jaita@medicomp.com
703.803.8080×221

Medicomp Systems innovates and continuously improves medical information technologies that provide clinicians with the power and freedom to focus on the patient. Medicomp’s EHR tools are dynamic and easy to use, based on the way clinicians think and work, and provide immediate access to the total patient picture. At the heart of every product is the powerful MEDCIN® Engine, a robust clinical data engine used by clinicians and hospitals throughout the world.

MEDSEEK
Booth 1345
Contact: Mandi Coker, Director, Corporate Marketing
mandi.coker@medseek.com
205.982.5821
MEDSEEK’s digital health solutions help healthcare organizations predict patient health requirements, plan capital investments, influence patient behavior, activate patients, expand business and manage patients across the continuum of care to find new cost savings and revenue streams. Find out how to strategically engage and manage your patients today – 888.MEDSEEK or sales@medseek.com.

MedVentive
Booth 6466-1, ACO Knowledge Center
Contact: Nancy Brown, Chief Growth Officer
nbrown@medventive.com
781.290.2511

MedVentive provides the tools and experience you need for two key issues faced in evolving into an ACO: understanding patient populations and being financially at risk for the quality and cost of care. MedVentive Population Manager provides the IT infrastructure needed to support FTC required Clinical Integration and overall population management. MedVentive Risk Manager provides the analytic platform to manage your multi-payer risk contracts.

Merge Healthcare
Booth 1023
Contact: Brenda Stewart, Director, Marketing Communications
brenda.stewart@merge.com
773.726.8901

Merge Healthcare is a leading provider of enterprise imaging and interoperability solutions. Merge solutions facilitate the sharing of images to create a more effective and efficient electronic healthcare experience for patients and physicians. Merge provides enterprise imaging solutions for radiology, cardiology, orthopaedics and eye care; a suite of products for clinical trials; software for financial and pre-surgical management, and applications that fuel the largest modality vendors in the world. Merge’s products have been used by healthcare providers, vendors and researchers worldwide to improve patient care for more than 20 years. This year, we are thrilled to showcase our comprehensive enterprise imaging solutions that allow you to image enable your EHR. You will also have the opportunity to register for FREE image sharing via our new cloud platform, Merge Honeycomb™, and learn how to earn Meaningful Use incentives with our specialty EHR solutions. Additional information can be found at www.merge.com.

MyHealthDIRECT
To schedule a meeting:
Contact: Zac Fritz, SVP of Sales and Marketing
zfritz@myhealthdirect.com
262.309.2090

MyHealthDIRECT provides the nation’s only ‘healthcare scheduling exchange’ (HSE) for health plans, hospitals, health systems, ACOs and HIEs.Their SaaS-platform is proven “commercial-grade” and “enterprise-ready” and is scalable, flexible, and secure. The MyHealthDIRECT HSE-platform is the industry’s only technology with proven application across the entire care continuum: from care coordination efforts and call centers to mHealth initiatives or Direct-to-Consumer (D2C) strategies and ACO referral management. MyHealthDIRECT: The nation’s only ‘healthcare scheduling exchange’.

NextGate
Booth 7000
Contact: Richard Garcia, VP Marketing
richard.garcia@nextgate.com
626.262.4010
Information is good. Knowledge is better! The NextGate® Registry Suite for Healthcare goes beyond standard integration to satisfy today’s intricate, multi-entity healthcare data exchange requirements. HIEs, ACOs, IDNs and similar organizations need a dynamic, sophisticated framework to coordinate information from diverse sources to support coherent and meaningful data exchange. The registry suite uses the leading MatchMetrix® data integration platform to analyze and integrate the different data elements of a complex activity, promoting greater efficiency and insight. The suite includes an EMPI, Provider Registry and Directory, Location Registry, Activity Registry, Code Set Registry, Enterprise Transaction Registry, and a Relation service to define associations between objects. With over 75 million unique identities managed by MatchMetrix and hundreds of registry implementations, NextGate offers unequalled expertise in deploying master index and data integration solutions. Be certain about the data you exchange!

Nordic Consulting Partners, Inc.
To schedule a meeting:
Contact: Drew Madden, President
drew.madden@nordicwi.com
608.268.6900
Nordic was founded by former Epic consultants, and is the largest Epic-only implementation firm in the country.We focus exclusively on Epic software implementations. We’re located in Madison, WI, home to Epic Systems, Inc., which gives us access to some of the top EMR experts in the industry. Our team of senior consultants average 6-year of Epic implementation experience; 80% are former Epic employees with an average of four certifications each. They’re seasoned professionals who have worked with hundreds of hospitals and clinics nationwide. Whether you need help with a short-term project, or a team of consultants to oversee implementation from start to finish, our staff will be valuable members of your team.Nordic works with healthcare organizations in 14 states, with clients that include Children’s hospitals, University hospitals and community healthcare providers of all sizes. We understand their dedication to patient care and the high standards their EMR projects must meet. Nordic will help you build the right team for your organization.

NTT DATA Healthcare Technologies (formerly Keane)
Booth 3064
Contact: Larry Kaiser, Senior Marketing Manager
lkaiser@keane.com
631.824.5318
In business since 1975 and based in the United States, NTT Data Healthcare Technologies offers complete IT solutions to hospitals and long-term care facilities throughout the country. NTT DATA’s proprietary software and services help health organizations increase efficiency, reduce medical errors, meet regulatory requirements, and enhance the revenue cycle. An electronic health record (EHR) solution, the Optimum suite of fully integrated certified clinical applications helps hospitals and healthcare facilities reduce medical errors, increase efficiency, and improve the delivery of care.
Stop by for a cup of cappuccino and find out how NTT DATA Healthcare Technologies can help you today.

Nuance Communications, Inc.
Booth 3523
Contact: Mark Erwich, Senior Director, Marketing
mark.erwich@nuance.com
781.565.5000

Nuance Healthcare, a division of Nuance Communications, is a market leader in providing clinical understanding solutions that accurately capture and transform the patient story into meaningful, actionable information. Thousands of hospitals, providers and payers worldwide trust Nuance voice-enabled clinical documentation and analytics solutions to facilitate smarter, more efficient decisions across the healthcare enterprise. These solutions are proven to increase clinician satisfaction and HIT adoption, supporting organizations to achieve Meaningful Use of EHR systems and transform to the accountable care model. Recognized as “Best-in-KLAS” 2004-2011 for Voice Recognition we invite you to learn more at booth #3523.

Orchestrate Healthcare
Booth 4269
Contact: Charlie Cook, President
charlie@orchestratehealthcare.com
970.963.0251

Orchestrate Healthcare won the 2011 Best in KLAS – Technical Services award. Come speak with us about why our KLAS score keeps rising every year and why we continue to win Best in KLAS awards. Orchestrate Healthcare was founded on the principals of: honesty, integrity and hard work.These key principals have lead to triple-digit growth since day one. Orchestrate Healthcare has also had tremendous success with our client feedback to KLAS Research. Orchestrate Healthcare won Best in KLAS – Technical Services in 2008. In 2009, we improved our KLAS score by a full point over our 2008 score, and placed 2nd in the 2009 Best in KLAS – Technical Services category. In 2010, Orchestrate Healthcare again increased our KLAS score to 94.2, but took 2nd place by 1/10th of a point. In 2011, we increased our score to 96.4 and won Best in KLAS – Technical Services for the 2nd time in the last 4 years. Out of 19 companies in the KLAS Technical Services category, Orchestrate Healthcare is the ONLY company to have 100% positive client commentary for the past 24 months. Orchestrate Healthcare has a philosophy of “do what’s right for the client” every day, and the management of the company stands behind you to do whatever it takes to exceed the client’s expectations.The KLAS scores and all the positive client commentary reflect that commitment to quality.

PatientKeeper Inc.
Booth 1045
Mobile Health Knowledge Center booth 12928
Contact: Cristina Christy,Senior Events Manager
cchristy@patientkeeper.com
781.373.6378
PatientKeeper® Inc., the leading provider of physician healthcare information systems, offers hospitals and practice groups highly intuitive software that streamlines physician workflow to improve productivity and patient care. PatientKeeper’s CPOE, physician documentation, electronic charge capture and other applications are used by over 40,000 physicians nationwide, and run on desktop and laptop computers and popular handheld devices and tablets. PatientKeeper’s software integrates with existing healthcare information systems at hospitals and practice groups to create the most effective solution for driving physician adoption of technology, meeting Meaningful Use and transitioning to ICD-10. (www.patientkeeper.com; Twitter: @patientkeeper)

Practice Fusion
Booth 4074
Contact: Kimberly Okazaki, Marketing Coordinator
kokazaki@practicefusion.com
415.992.6462

Practice Fusion provides a free, web-based Electronic Health Record (EHR) system to physicians.With charting, scheduling, e-prescribing (eRx), lab integrations, referral letters, Meaningful Use certification, unlimited support and a Personal Health Record for patients, Practice Fusion’s EHR addresses the complex needs of today’s healthcare providers and disrupts the health IT status quo. Practice Fusion is the fastest growing EHR community in the country with more than 130,000 users serving 30 million patients. The company closed a $23 million Series B round of financing led by Founders Fund in 2011. For more information about Practice Fusion, please visit www.practicefusion.com.

Quality IT Partners, Inc.
To schedule a meeting:
Contact: Donna Eversole, MBA, BSN, RN, CPHIMS, Director Healthcare Practice
deversole@qitp.com
904.610.7933
Quality is a hands-on, technology-driven consulting company. We assist healthcare organizations with complete end-to-end systems planning, acquisition, customization, implementation and maintenance including technical and operational support. We specialize in assisting clients in transitioning from dated, expensive legacy technologies to modern, cost-effective solutions using leading-edge implementation practices. Our implementation professionals are experienced clinicians and financial consultants and have experience with all major HIS vendors. We view each assignment as an opportunity to transfer our knowledge and experiences to our clients’ staff.

Shareable Ink
Booth 7100
Contact: Suzanne Cogan, Vice President, Sales and Marketing
scogan@shareableink.com
877.572.7423 x802

Shareable Ink is the enterprise cloud-based platform that incorporates natural input tools, including iPads and digital pen and paper technology. Clinicians can continue documenting in the fastest, most efficient manner. The resulting structured and clinically-encoded output populates the EHR with discrete data, as if typed in directly. Built-in analytics give hospitals and practices insight into their operations – from a clinical, quality, and efficiency standpoint.
Information Week recently named Shareable Ink one of 12 EHR vendors that “stand out” – out of 1,300 Meaningful Use-certified systems. Visit us at HIMSS for an interactive demo featuring our Physician Progress Notes with Charge Capture and Patient History & Signature Capture solutions. We’ll also have a special unveiling of our iPad App – you won’t want to miss it! For everyone who mentions ‘DOCTOR’ at our booth, we’ll be making a donation to one of our favorite charities, Doctors without Borders.

SRSsoft
Booth 12721
Contact: Evan Steele, CEO
esteele@srssoft.com
800.288.8369
SRS is the leading provider of productivity-enhancing EHR technology and services for high-performance physicians—with a successful adoption rate unparalleled in the industry. Offered via the Unified Desktop™, the robust EHR, SRS CareTracker PM, SRS PACS, and SRS Patient Portal increase speed, boost revenue, free physicians’ time, and heighten patient care and satisfaction. For more information on SRS, visit www.srssoft.com, e-mail info@srssoft.com, fax 201.802.1301, or call 800.288.8369.

Software Testing Solutions
To schedule a meeting:
Contact: Maegan Scarlett, Marketing Specialist
himss@sts-healthcare.com
877.765.0100 ext. 1
You’re not still running those old terminal based legacy applications in your institution for CPOE, lab, blood bank and anatomic pathology – so why are you still testing them the same way? Now you can achieve a predictable time, cost and quality for your upgrades. Software Testing Solutions’ (STS) innovative automated testing & validation products for hospital software systems including Epic, Sunquest and SCC Soft, deliver exhaustive testing quickly and efficiently, saving time & money while reducing risk, increasing patient safety and ensuring regulatory compliance. Contact us today for more information.

Streamline Health
Booth 2058
Contact: Rick Leach, Senior Vice President and Chief Marketing Officer
rick.leach@streamlinehealth.net
513.794.7112
Streamline Health provides healthcare information technology solutions that help hospitals and physician groups improve efficiencies and business processes across the enterprise to enhance and protect the revenues. Our enterprise content management solutions transform unstructured data into digital assets that seamlessly integrate with disparate clinical, administrative, and financial information systems. Our business analytics solutions provide real-time access to key performance metrics that enable healthcare organizations to identify and manage opportunities to maximize their financial performance. Our integrated workflow systems automate and manage critical business activities to improve organizational accountability to drive both operational and financial performance. For more information visit www.streamlinehealth.net.

Sunquest Information Systems, Inc.
Booth 423
Contact: Kymberly Calvo,Marketing Communications Specialist
kymberly.calvo@sunquestinfo.com
408.702.1151
Sunquest Information Systems is committed to patient safety, workflow excellence, predictive medicine, and physician & patient affinity. Utilizing this dedication, Sunquest proudly offers global diagnostic IT solutions that transform the delivery of healthcare for more than 1,400 organizations and 380,000 users worldwide. Come by Booth 423 and discover the value Sunquest’s products deliver to our clients every day. Experience Sunquest’s community-based outreach tour featuring our fully integrated suite of products built on technology that enables and supports business growth and operational efficiency. Sunquest’s closed-loop collection and transfusion management tour will highlight solutions designed to virtually eliminate patient identification, labeling and transfusion errors at the bedside, in the ED or in the surgical suite. Sunquest is your path to the heart of healthcare.

Surgical Information Systems
Booth 1339
Allscripts Booth 3016
Siemens Booth 2423
Interoperability Showcase Booth 11000, Hall G
Contact: Emmy Weber, VP of Marketing
weber@sisfirst.com
678.507.1706

Surgical Information Systems (“SIS”) provides software solutions that are uniquely designed to add value at every point of the perioperative process. Developed specifically for the complex surgical environment, all SIS solutions – including anesthesia – are architected on a single database and integrate easily with other hospital systems. SIS offers the only surgical scheduling system and the only anesthesia information management system endorsed by the American Hospital Association (AHA), and both a rules-based charging system and analytics module that has been granted Peer Reviewed status by the Healthcare Financial Management Association (HFMA). Visit SIS at HIMSS12 to see the latest in perioperative IT including anesthesia, patient tracking and analytics modules.

Transcend Services and Salar
Booth 4674
Contact: Donna Rhines, Director of Marketing
donna.rhines@trcr.com
678.808.0680

Transcend/Salar delivers clinical documentation solutions that are flexible to fit the needs of our clients. We offer the industry’s only physician-centric, single-source solution for advanced electronic clinical documentation. Our full spectrum of services and products include: full- to partial-outsourced transcription services, a world-class transcription platform, dynamic clinical documentation templates and physician charge capture.
Transcend/Salar products have highly-customizable physician interfaces that integrate easily with existing electronic medical record systems. Clients that utilize Transcend experience increased physician adoption through flexible solutions that fit the physician workflow. With Transcend/Salar, physicians and hospitals alike achieve notable productivity, financial and patient safety improvements. Encore™, Transcend’s powerful backend speech recognition transcription platform and Salar’s transformational, physician-centric, inpatient documentation and billing products (TeamNotes™, TeamRelay™, TeamQuery™ and TAP Charge Capture™). Experience a demo or a presentation and see how you can benefit.
- Substantial cost savings
- Improved efficiency and significant productivity increases
- Expedited physician workflow and optimized physician billing
- Real-time physician query and concurrent documentation review + Increased inpatient revenue
- Meaningful Use Stage 1 certification

Trustwave
Booth: 8805
Contact: Dan Kunkel, Healthcare Solutions
jvickery@trustwave.com
312.873.7659
Trustwave is a leading provider of information security and compliance management solutions to businesses and government entities throughout the world. Trustwave provides a unique approach with comprehensive solutions such as the award-winning TrustKeeper® and other proprietary security solutions including SIEM, WAF, EV SSL certificates and secure digital certificates. Specifically for hospitals, IDNs, insurers and physicians, Trustwave Healthcare Solutions offer customizable data protection, and help safeguard PHI and address HIPAA requirements. For more information, visit www.trustwave.com/healthcare.

T-System
Booth 4012
Contact: Ann Baty,Senior Marketing Coordinator
abaty@tsystem.com
469.791.2445

T-System, Inc. sets the industry standard for clinical, business and IT solutions for emergency medicine, with approximately 40 percent of the nation’s emergency departments using T-System solutions.To meet the individual needs of hospitals, T-System offers both paper and electronic systems. These tools help clinicians provide better patient care, while improving efficiency and the bottom line. Today, more than 1,700 emergency departments rely on T-System’s gold-standard content and workflow solutions. For more information, visit www.tsystem.com. Follow T-System on Twitter (@TSystem) and like T-System on Facebook.
Stop by our “virtual” emergency department at Booth 4012 to see and try our solutions in action. Find out how The T SystemEV has helped more than 42 hospitals attest to Stage 1 Meaningful Use. Learn about how our new revenue cycle management services can boost your bottom line. Document a patient encounter with DigitalShare and T Sheets or try T-System clinical decision support. Answer a question about Continuity, our new ACO solution, for a chance to win an iPad 2.
We will also be demonstrating at the Interoperability Showcase (Hall G, Booth #11000) how the emergency department might contribute information that would enable a smoother transition of care. T-System Vice President of Solution Development Bill Hall will give a presentation, “Interoperability and the ED: Replacing Care Transactions with Transitions,” at the Showcase on Tuesday at 1:15 p.m. Additionally, two T-System clients will be presenting the senior executive session, “Emergency Medicine EHR Helps Drive Meaningful Use Readiness” on Tuesday at 11 a.m. in Marcello 4506. To learn more about these presentations and our industry leading ED solutions, visit us at Booth 4012.

Versus Technology
Booth 5852
Contact: Stephanie Bertschy, Director of Marketing
skb@versustech.com
231-946-5868
Versus gives healthcare institutions the power to locate patients, staff and equipment in real-time, and automate a multitude of clinical tasks. The result: optimized workflow, improved patient care and streamlined processes that set a higher standard in healthcare. Since 1988, hundreds of hospitals have strengthened performance with Versus locating advantages.

Virtelligence Consulting
Booth 720
Contact: JoAnn Simon, Vice President
jsimon@virtelligence.com
952.548.6611
Founded in 1998, Virtelligence is a privately held premier Healthcare IT consulting firm that offers solution advisory and Healthcare IT consulting services to payers, providers, and life science organizations nationwide. In today’s competitive Healthcare IT marketplace Virtelligence stands as one of the most trusted Consulting partners in the industry. Our success comes from a solid understanding of our client’s business and access to the best Healthcare IT resources available. Our personalized approach has given us the competitive edge in providing innovative advice and world-class service to our clients.

Vitalize Consulting Solutions, an SAIC company
Booth 3338
Contact: Cyndi Cahill, SVP Marketing and Sales Support
ccahill@getvitalized.com
610.444.1233
Vitalize Consulting Solutions, an SAIC company (VCS) provides diversified clinical, business, and IT solutions for healthcare enterprises nationwide and in Canada. VCS’ comprehensive programs and services lineup includes system implementation, integration, optimization, project management, custom reporting, education, and knowledge transfer expertise. To facilitate clients’ strategic IT initiatives, our consultants first listen to, then advise, and ultimately strengthen their customers’ IT team. Primarily engaged with Allscripts™, Cerner, Epic, McKesson, MEDITECH and Siemens users, and the Ambulatory and Practice Management arenas, VCS cultivates enduring relationships by supplying experienced professionals who consistently exceed clients’ expectations. Since being acquired by Science Applications International Corporation (SAIC) in August 2011, VCS is now able to provide expanded service lines to its current and future clients, ultimately strengthening our solutions. Please visit us at www.getvitalized.com for more information.

Vocera Communications, Inc.
Booth 2245
HIMSS Interoperability Showcase
Contact: Diana Cropley, Marketing
info@vocera.com
800.331.6356
Vocera provides mobile communication solutions focused on addressing critical communication challenges facing hospitals today. We help our customers improve patient safety and satisfaction, and increase hospital efficiency and productivity through our Voice Communication, Secure Messaging, and Care Transition solutions. Exclusively endorsed by the American Hospital Association, the Vocera solutions are installed in more than 800 hospitals and healthcare facilities worldwide.

Winthrop Resources
To schedule a meeting:
Contact: Dan Many, Director of Business Development
dmandy@winthropresources.com
952.656.7687

Winthrop provides custom technology leasing solutions allowing hospitals to remain independent of technology providers, to refresh technology when needed, and to preserve cash. We believe that spending cash or bank financing to buy technology assets doesn’t make sense since those assets lose value quickly, require increasing expense to keep running, and need to be upgraded and changed to support organizational goals and regulatory requirements.

ZirMed
Booth 3638
Contact: Kent Rowe, VP Sales
sales@zirmed.com
877.494.1032
We’re ZirMed, a leading provider of healthcare revenue cycle technology and information solutions. Serving 113,000 healthcare providers across all care settings who in turn provide services to more than 1 in every 10 Americans, we are a nationally recognized leader in understanding the flow of money and information in healthcare. Addressing the entire revenue cycle, our offerings include eligibility verification, claims management, patient payment estimation, patient payment processing, online bill pay, online and offline statement delivery, innovative lockbox services, analytics, coding compliance, and more. Delivered via a SaaS model, our solutions are compatible with any industry standard Healthcare Information or Practice Management System, and can be used directly within the ZirMed domain or embedded within partner software applications. ZirMed received a “Best in KLAS” ranking for 2011 from independent healthcare IT research firm KLAS, and ranked #1 in overall satisfaction three years in a row. For more information about how our solutions simplify the complexities of payments for providers and patients visit www.zirmed.com.
![]() From Don Pablo: “Re: data breaches. I saw where you are not relaying the stolen laptop breaches since they have become commonplace. I used to work in financial services and watched for reports of breaches. This was my favorite site to check a couple of times a week. I bring it to your attention as not every breach is easily found.”Great site to check out, unless you are obsessively worried about your personal data getting into the wrong hands, because lots of organizations seem to be losing our data.
From Don Pablo: “Re: data breaches. I saw where you are not relaying the stolen laptop breaches since they have become commonplace. I used to work in financial services and watched for reports of breaches. This was my favorite site to check a couple of times a week. I bring it to your attention as not every breach is easily found.”Great site to check out, unless you are obsessively worried about your personal data getting into the wrong hands, because lots of organizations seem to be losing our data.![]() From WellHeeled: “HIStalkapalooza. I just want to be sure it is as black tie and glamorous as last year (so I pack the appropriate Red Carpet attire)…is that the case?” There may not be a red carpet this year, but readers have assured me they are packing their sequins, high heels, and more than one black tie. SmyrnaGirl, for example, tweeted that she is bringing her A game with these hot shoes.
From WellHeeled: “HIStalkapalooza. I just want to be sure it is as black tie and glamorous as last year (so I pack the appropriate Red Carpet attire)…is that the case?” There may not be a red carpet this year, but readers have assured me they are packing their sequins, high heels, and more than one black tie. SmyrnaGirl, for example, tweeted that she is bringing her A game with these hot shoes.![]() From Lucky Jackson: “Best dressed at HIStalkapalooza. Tell me what I have to do to win one of Mr. H’s big prizes.” In the fashion categories, we have HIStalk King (best-dressed man), HIStalk Queen (best-dressed woman), Best Elvis Impersonator (based solely on attire, so choose your favorite young or old Elvis outfit and don’t worry about the singing), and Best Left-in-Vegas Attire (think showgirl or over-the-top glitz; Mr. H is hoping for a lot of showgirls.) If you want to be in the running for the fashion or the shoe contests, arrive early because our judges will be selecting finalists between 6:30 and 7:30 pm.
From Lucky Jackson: “Best dressed at HIStalkapalooza. Tell me what I have to do to win one of Mr. H’s big prizes.” In the fashion categories, we have HIStalk King (best-dressed man), HIStalk Queen (best-dressed woman), Best Elvis Impersonator (based solely on attire, so choose your favorite young or old Elvis outfit and don’t worry about the singing), and Best Left-in-Vegas Attire (think showgirl or over-the-top glitz; Mr. H is hoping for a lot of showgirls.) If you want to be in the running for the fashion or the shoe contests, arrive early because our judges will be selecting finalists between 6:30 and 7:30 pm.
![]() From Former CIO: “Re: booth crawl. I hope the sponsors will have the answers readily available in the booths. With 50+ answers to get in around 11 hours of booth time, there won’t be much time for sales pitches.” We’ve asked the sponsors to have their booth crew prepared with the answers. I expect some will just post the answer on their wall. As a refresher to the detailed instructions: (a) download the form here and print it off, (b) get your answers from the booths and Web pages listed; (c) post them to the online entry form by Wednesday evening at 7:00, and (d) watch HIStalk Wednesday evening to see if you won. At minimum, you get good exercise and flaunt a confident, purposeful stride as you move from one booth to the next on a Apple-seeking mission instead of just meandering around following the scent of some vendor’s freshly baked cookies. With luck (and the odds should be decent), you’ll pack home one of 55 iPads. And as I mentioned last time, I’m the one grading the entries, and if you miss a question or two, I’ll most likely be lenient because I really want you to have an iPad. I was indifferent to the device when I won mine at HIMSS last year, but it has totally replaced my iPod Touch for around-the-house stuff: checking the weather, looking at e-mail, doing a quick order on Amazon, and reading Kindle books.
From Former CIO: “Re: booth crawl. I hope the sponsors will have the answers readily available in the booths. With 50+ answers to get in around 11 hours of booth time, there won’t be much time for sales pitches.” We’ve asked the sponsors to have their booth crew prepared with the answers. I expect some will just post the answer on their wall. As a refresher to the detailed instructions: (a) download the form here and print it off, (b) get your answers from the booths and Web pages listed; (c) post them to the online entry form by Wednesday evening at 7:00, and (d) watch HIStalk Wednesday evening to see if you won. At minimum, you get good exercise and flaunt a confident, purposeful stride as you move from one booth to the next on a Apple-seeking mission instead of just meandering around following the scent of some vendor’s freshly baked cookies. With luck (and the odds should be decent), you’ll pack home one of 55 iPads. And as I mentioned last time, I’m the one grading the entries, and if you miss a question or two, I’ll most likely be lenient because I really want you to have an iPad. I was indifferent to the device when I won mine at HIMSS last year, but it has totally replaced my iPod Touch for around-the-house stuff: checking the weather, looking at e-mail, doing a quick order on Amazon, and reading Kindle books.![]() From Elaine: “Re: HIMSS. Any word on a McKesson event? It would be fun to let loose a bit after hours.” I’ll be honest in saying that I don’t even open any of the HIMSS-related mail I get (sorry, companies who pay big bucks to send it) so I don’t know anything about their event. The only ones that have risen above the noise for me were from companies that contacted me directly: a cool-sounding Cerner event at the Bellagio (called me at work), a great-sounding Iatric Systems lunch (e-mailed), and and SCI Solutions get-together (sent to my Mr. HIStalk e-mail). I’ll make this offer: for companies throwing an event that’s open to anyone (and that includes vendor people, just to be clear) let me know and I’ll mention it here, as long as you’re OK with the possibility that gregarious HIStalk readers will overwhelm you with interest, which we have to re-learn every year with HIStalkapalooza. Everybody ought to have a party invitation or two, don’t you think?
From Elaine: “Re: HIMSS. Any word on a McKesson event? It would be fun to let loose a bit after hours.” I’ll be honest in saying that I don’t even open any of the HIMSS-related mail I get (sorry, companies who pay big bucks to send it) so I don’t know anything about their event. The only ones that have risen above the noise for me were from companies that contacted me directly: a cool-sounding Cerner event at the Bellagio (called me at work), a great-sounding Iatric Systems lunch (e-mailed), and and SCI Solutions get-together (sent to my Mr. HIStalk e-mail). I’ll make this offer: for companies throwing an event that’s open to anyone (and that includes vendor people, just to be clear) let me know and I’ll mention it here, as long as you’re OK with the possibility that gregarious HIStalk readers will overwhelm you with interest, which we have to re-learn every year with HIStalkapalooza. Everybody ought to have a party invitation or two, don’t you think?![]() From MJOG: “Re: GE Centricity Advance. Discontinued with no warning and very little time to transition. They are offering Centricity CPS, but at $1,500 it is too pricey for the small practices that used Advance. Even their own VARs can’t guarantee a transition within GE’s timeframe. Practices that went live with Advance in January 2012 have to pay in full for implementation of dead software. GE is really out of touch.” I think what you are seeing is what lots of people predicted: when EMR certification turned out to be too easy to achieve and everybody earned it, that left it up to the market to weed out those products and companies that have a less than a fully competitive position in the face of disruptive companies that are happy to sell hosted, easily implemented systems for a few hundred dollars per month. The MU carrot is forcing practices to choose their dance partners nearly simultaneously, so the consolidation writing is on the wall as the rich get richer. It’s painful for existing customers, but is both desirable and inevitable over the longer term. Maybe we should have a mandatory Y2K every 10 years to thin the herd.
From MJOG: “Re: GE Centricity Advance. Discontinued with no warning and very little time to transition. They are offering Centricity CPS, but at $1,500 it is too pricey for the small practices that used Advance. Even their own VARs can’t guarantee a transition within GE’s timeframe. Practices that went live with Advance in January 2012 have to pay in full for implementation of dead software. GE is really out of touch.” I think what you are seeing is what lots of people predicted: when EMR certification turned out to be too easy to achieve and everybody earned it, that left it up to the market to weed out those products and companies that have a less than a fully competitive position in the face of disruptive companies that are happy to sell hosted, easily implemented systems for a few hundred dollars per month. The MU carrot is forcing practices to choose their dance partners nearly simultaneously, so the consolidation writing is on the wall as the rich get richer. It’s painful for existing customers, but is both desirable and inevitable over the longer term. Maybe we should have a mandatory Y2K every 10 years to thin the herd.![]() From All Hat No Cattle: “Re: electronic problem lists. What do you think of this idea?” Reported in a JAMIA article, Brigham and Women’s sets up EHR alerts to prompt the physician to review the problem list if patient data in the EHR suggests that any of 17 specific conditions (asthma, hypertension, diabetes, etc.) might be present but undocumented. The alerts were accepted 41% of the time, more problems were documented, and interventions and quality improvement work could presumably be more specifically targeted. I like the idea only because it has the potential (although modest, I expect) to improve the care of individual patients, unlike the similar adverse drug event triggers that have always seemed to me to be a complete waste of time except as a learning tool that nobody ever seems to learn from. On the other hand, pestering docs with alerts that are not helpful almost 60% of the time indicates a need for algorithm refinement. That’s where these projects end a lot of the time – the available information just isn’t good enough to improve the hit rate.
From All Hat No Cattle: “Re: electronic problem lists. What do you think of this idea?” Reported in a JAMIA article, Brigham and Women’s sets up EHR alerts to prompt the physician to review the problem list if patient data in the EHR suggests that any of 17 specific conditions (asthma, hypertension, diabetes, etc.) might be present but undocumented. The alerts were accepted 41% of the time, more problems were documented, and interventions and quality improvement work could presumably be more specifically targeted. I like the idea only because it has the potential (although modest, I expect) to improve the care of individual patients, unlike the similar adverse drug event triggers that have always seemed to me to be a complete waste of time except as a learning tool that nobody ever seems to learn from. On the other hand, pestering docs with alerts that are not helpful almost 60% of the time indicates a need for algorithm refinement. That’s where these projects end a lot of the time – the available information just isn’t good enough to improve the hit rate.
![]() Thanks to Streamline Health, supporting HIStalk as a Platinum Sponsor. The Cincinnati, OH-based company offers the AccessAnyWare document management system, which supports hybrid document-electronic hospitals (which is the vast majority) by organizing their information to streamline processes and improve patient care. Its OpportunityAnyWare business analytics solution aggregates information from disparate systems so that users can perform data mining and collaboration using dashboards that can include an unlimited number of key performance indicators, metrics, and alerts. Its Patient Access solutions integrate document workflow related to referrals, pre-op documentation, and financial forms to eliminate delays and process barriers, accelerating the billing process and increasing employee productivity. They even have a solution (CharityWare) to manage the need-based financial assistance screening process. Before and after stats for several clients are here. The executive team has a ton of healthcare experience and the company’s chairman of the board is our old HIStalk friend Jon Phillips of Healthcare Growth Partners, who I interview once a year or so because his healthcare IT business predictions are uncanny (and it’s about time to do that again.) Thanks to Streamline Health for helping us do what we do.
Thanks to Streamline Health, supporting HIStalk as a Platinum Sponsor. The Cincinnati, OH-based company offers the AccessAnyWare document management system, which supports hybrid document-electronic hospitals (which is the vast majority) by organizing their information to streamline processes and improve patient care. Its OpportunityAnyWare business analytics solution aggregates information from disparate systems so that users can perform data mining and collaboration using dashboards that can include an unlimited number of key performance indicators, metrics, and alerts. Its Patient Access solutions integrate document workflow related to referrals, pre-op documentation, and financial forms to eliminate delays and process barriers, accelerating the billing process and increasing employee productivity. They even have a solution (CharityWare) to manage the need-based financial assistance screening process. Before and after stats for several clients are here. The executive team has a ton of healthcare experience and the company’s chairman of the board is our old HIStalk friend Jon Phillips of Healthcare Growth Partners, who I interview once a year or so because his healthcare IT business predictions are uncanny (and it’s about time to do that again.) Thanks to Streamline Health for helping us do what we do.![]() I realized today that I have listed the exotic recipe for the IngaTinis to be served at next week’s event, but forgot to mention the other custom-created specialty cocktails that will be served (the bartenders at First are seriously legendary craftspeople of the alcoholic arts.) The Mr. H Incognito is a rum punch with ingredients that are, like its namesake, best left undisclosed. For you root beer fans – and you know who you are – the ESD Activation Sensation is a mixture of IBC root beer with whipped cream vodka (who knew?) with a brandied cherry garnish. And while I’m on the topic, I should repeat that we are ecstatic to host those lucky folks who received an invitation, but we regretfully cannot accommodate anyone who didn’t (guests, co-workers, hastily propositioned showgirls, etc.) You are welcome to swing by at 8:00 p.m. to see if no-shows have freed up space, but otherwise we’re packed to the rafters.
I realized today that I have listed the exotic recipe for the IngaTinis to be served at next week’s event, but forgot to mention the other custom-created specialty cocktails that will be served (the bartenders at First are seriously legendary craftspeople of the alcoholic arts.) The Mr. H Incognito is a rum punch with ingredients that are, like its namesake, best left undisclosed. For you root beer fans – and you know who you are – the ESD Activation Sensation is a mixture of IBC root beer with whipped cream vodka (who knew?) with a brandied cherry garnish. And while I’m on the topic, I should repeat that we are ecstatic to host those lucky folks who received an invitation, but we regretfully cannot accommodate anyone who didn’t (guests, co-workers, hastily propositioned showgirls, etc.) You are welcome to swing by at 8:00 p.m. to see if no-shows have freed up space, but otherwise we’re packed to the rafters.![]() Thanks and welcome to HealthMEDX as a new HIStalk Platinum Sponsor. The Ozark, MO company offers an integrated clinical and financial system that covers all post-acute care settings: long-term care, home health, hospital, rehab, and Continuing Care Retirement Communities (if you’re a hospital person and think this doesn’t pertain to your organization, it definitely does – the comfortable lines between acute care hospitals and all these other important venues of care are getting blurrier by the minute.) When ACO-type arrangements put you on the hook to coordinate care with these other providers, solutions from HealthMEDX ensure that best practices are followed to meet regulatory requirements, reduce cost, reduce errors, and (pay attention here) reduce those hospital readmissions that come right out of your pocket. Every one of HHS’s favorite programs requires unheard-of levels of data-sharing and coordination to give patients coordinated care at the most cost-effective location. HealthMEDX has solutions running in more than 3,000 facilities and has earned CCHIT certification for Home Health and SNF in addition to ONC-ATCB modular certification for both hospitals and EPs. And lastly, if you’re thinking, “I know I’ve heard of HealthMEDX somewhere,” it’s the company that former McKesson Technology Solutions President Pam Pure joined as CEO right before Christmas. Thanks to HealthMEDX for supporting HIStalk.
Thanks and welcome to HealthMEDX as a new HIStalk Platinum Sponsor. The Ozark, MO company offers an integrated clinical and financial system that covers all post-acute care settings: long-term care, home health, hospital, rehab, and Continuing Care Retirement Communities (if you’re a hospital person and think this doesn’t pertain to your organization, it definitely does – the comfortable lines between acute care hospitals and all these other important venues of care are getting blurrier by the minute.) When ACO-type arrangements put you on the hook to coordinate care with these other providers, solutions from HealthMEDX ensure that best practices are followed to meet regulatory requirements, reduce cost, reduce errors, and (pay attention here) reduce those hospital readmissions that come right out of your pocket. Every one of HHS’s favorite programs requires unheard-of levels of data-sharing and coordination to give patients coordinated care at the most cost-effective location. HealthMEDX has solutions running in more than 3,000 facilities and has earned CCHIT certification for Home Health and SNF in addition to ONC-ATCB modular certification for both hospitals and EPs. And lastly, if you’re thinking, “I know I’ve heard of HealthMEDX somewhere,” it’s the company that former McKesson Technology Solutions President Pam Pure joined as CEO right before Christmas. Thanks to HealthMEDX for supporting HIStalk.![]() Inga is interviewed by the folks from Dodge Communications, in which she downplays her role in HIStalk and makes me seem way more interesting and virtuous than I really am. Feeling uncharacteristically affectionate after reading it because she was so sweet in her comments, I wanted to have Valentine’s Day flowers delivered to her, but the florist reacted with a combination of a contemptuous laugh and and annoyed snort when I called up Tuesday morning and cheerfully asked if they could deliver that same day (I may offer her and Dr. Jayne a spa day at HIMSS instead.) Anyway, here’s a quote, which I can verify as accurate because I’ve hung out with her at HIMSS:
Inga is interviewed by the folks from Dodge Communications, in which she downplays her role in HIStalk and makes me seem way more interesting and virtuous than I really am. Feeling uncharacteristically affectionate after reading it because she was so sweet in her comments, I wanted to have Valentine’s Day flowers delivered to her, but the florist reacted with a combination of a contemptuous laugh and and annoyed snort when I called up Tuesday morning and cheerfully asked if they could deliver that same day (I may offer her and Dr. Jayne a spa day at HIMSS instead.) Anyway, here’s a quote, which I can verify as accurate because I’ve hung out with her at HIMSS:![]() GE Healthcare and Microsoft announce the name of their new joint venture as Caradigm, also announcing company executives and a board of directors comprised of company insiders. We cited a Geekwire article on February 3 speculating that Caradigm would be the name. The companies confirm that they’re working with the CenCal Regional Health Authority in Santa Barbara, CA to obtain permission to use the Caradigm name, which that organization trademarked years ago (their website still comes up at caradigm.com.) GE and Microsoft admit that they invested a lot more due diligence in choosing the Caradigm name than did CenCal RHA, which picked it in an employee “pick a name for our new company” contest 2002. The employee who came up with it got $50 and a pizza party.
GE Healthcare and Microsoft announce the name of their new joint venture as Caradigm, also announcing company executives and a board of directors comprised of company insiders. We cited a Geekwire article on February 3 speculating that Caradigm would be the name. The companies confirm that they’re working with the CenCal Regional Health Authority in Santa Barbara, CA to obtain permission to use the Caradigm name, which that organization trademarked years ago (their website still comes up at caradigm.com.) GE and Microsoft admit that they invested a lot more due diligence in choosing the Caradigm name than did CenCal RHA, which picked it in an employee “pick a name for our new company” contest 2002. The employee who came up with it got $50 and a pizza party.![]() A New York Times piece says that Essence Healthcare, financially backed by legendary Silicon Valley investor John Doerr, is finally bearing fruit. Two of its holdings are ClearPractice (EMRs) and Lumeris (analytic software.) Lumeris was just announced as one of the purchasers of healthcare communication network provider NaviNet, where Lumeris software will help physicians answer administrative questions sent via NaviNet.
A New York Times piece says that Essence Healthcare, financially backed by legendary Silicon Valley investor John Doerr, is finally bearing fruit. Two of its holdings are ClearPractice (EMRs) and Lumeris (analytic software.) Lumeris was just announced as one of the purchasers of healthcare communication network provider NaviNet, where Lumeris software will help physicians answer administrative questions sent via NaviNet.![]() Meditech kills its contested $65 million project to build an office complex in Freetown, MA, moving on to other location possibilities after a protracted archaeological fight with the state’s historical commission. Freetown gets to keep an empty lot that may or may not contain Native American remains, while somewhere else gets 800 high tech jobs.
Meditech kills its contested $65 million project to build an office complex in Freetown, MA, moving on to other location possibilities after a protracted archaeological fight with the state’s historical commission. Freetown gets to keep an empty lot that may or may not contain Native American remains, while somewhere else gets 800 high tech jobs.
![]() The VA wants a 7% increase in its FY 2013 IT budget, looking for $3.37 billion. It wants $169 million to continue development of a shared EMR with the Department of Defense, $53 million to develop a Virtual Lifetime Electronic Record, and $1.45 billion for hardware maintenance. The VA seems to be less optimistic that it seemed previously about turning over its VistA data centers to DoD, saying that unless DoD carves out specific space within its data centers to allow VA personnel to run its own systems, they will pursue setting up interim data centers. Nice digging by the folks at Nextgov.
The VA wants a 7% increase in its FY 2013 IT budget, looking for $3.37 billion. It wants $169 million to continue development of a shared EMR with the Department of Defense, $53 million to develop a Virtual Lifetime Electronic Record, and $1.45 billion for hardware maintenance. The VA seems to be less optimistic that it seemed previously about turning over its VistA data centers to DoD, saying that unless DoD carves out specific space within its data centers to allow VA personnel to run its own systems, they will pursue setting up interim data centers. Nice digging by the folks at Nextgov.![]() In Canada, the illegally accessed medical records of a high-ranking member of the country’s Veterans Review and Appeal Board are used in a smear campaign by fellow agency members who disagreed with his review decisions. Up to 40 officials accessed the files of the decorated veteran in order to use his service-related disabilities to discredit him.
In Canada, the illegally accessed medical records of a high-ranking member of the country’s Veterans Review and Appeal Board are used in a smear campaign by fellow agency members who disagreed with his review decisions. Up to 40 officials accessed the files of the decorated veteran in order to use his service-related disabilities to discredit him.![]() A Bloomberg article says that TV cable carriers are building up their broadband revenue from hospitals and practices, offsetting declining residential cable subscriber counts by charging medical users higher prices for using their networks. Cox says telecommunications companies such as AT&T and Verizon have 80% of the healthcare business, which it estimates at $460 million in the areas it serves. Comcast says healthcare represents a big chunk of the business services market that it estimates is worth $10-15 billion per year. Cable companies can offer lower prices through bundling, but they are less competitive in the areas of data security and wireless communications. AT&T says its healthcare revenue is $5 billion per year.
A Bloomberg article says that TV cable carriers are building up their broadband revenue from hospitals and practices, offsetting declining residential cable subscriber counts by charging medical users higher prices for using their networks. Cox says telecommunications companies such as AT&T and Verizon have 80% of the healthcare business, which it estimates at $460 million in the areas it serves. Comcast says healthcare represents a big chunk of the business services market that it estimates is worth $10-15 billion per year. Cable companies can offer lower prices through bundling, but they are less competitive in the areas of data security and wireless communications. AT&T says its healthcare revenue is $5 billion per year.![]() This isn’t really healthcare related, but it’s too funny not to mention. A Marshall University student files suit against a fraternity and one of its members after a party at the fraternity house, in which the allegedly intoxicated fraternity brother tried to shoot a bottle rocket out of his rear. The plaintiff says the bottle rocket exploded in the brother’s rectum, which according to the suit, “startled the plaintiff and caused him to jump back” and fall off the deck, with the resulting injuries costing him playing time with the baseball team.
This isn’t really healthcare related, but it’s too funny not to mention. A Marshall University student files suit against a fraternity and one of its members after a party at the fraternity house, in which the allegedly intoxicated fraternity brother tried to shoot a bottle rocket out of his rear. The plaintiff says the bottle rocket exploded in the brother’s rectum, which according to the suit, “startled the plaintiff and caused him to jump back” and fall off the deck, with the resulting injuries costing him playing time with the baseball team.



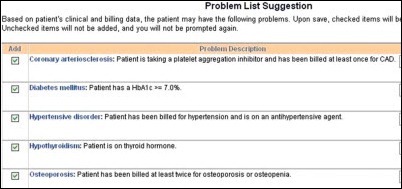













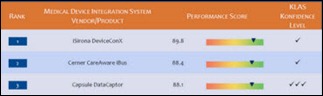




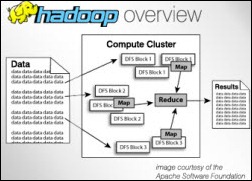


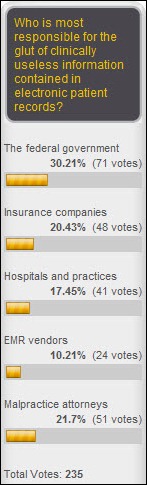















































































































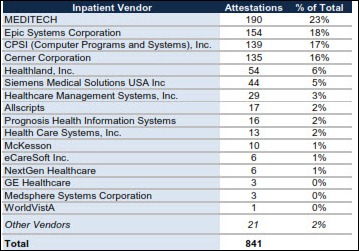
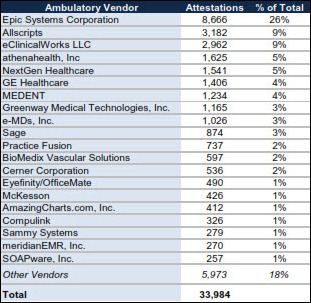



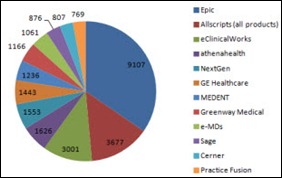












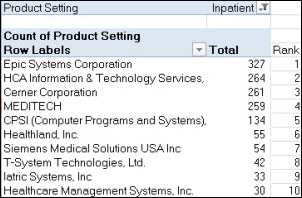
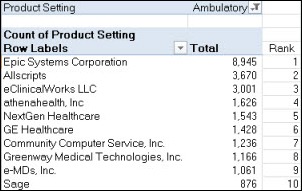






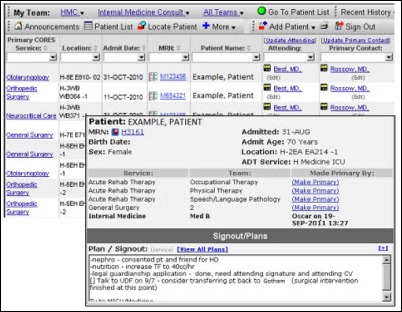












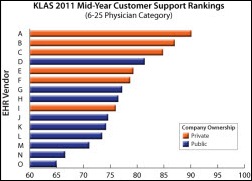














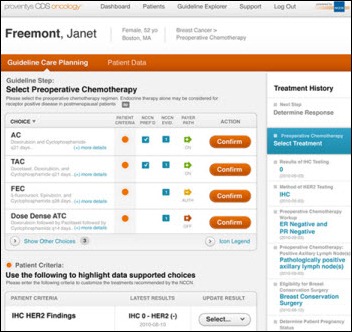





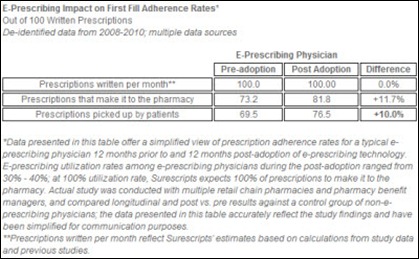






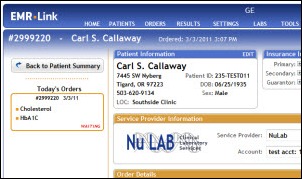






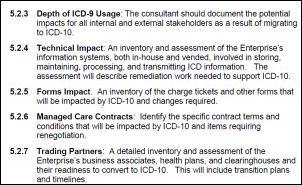


















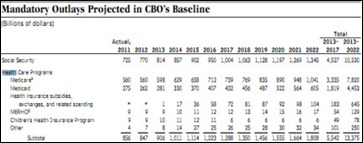
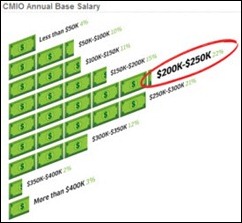


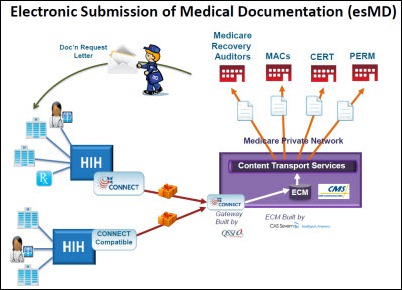
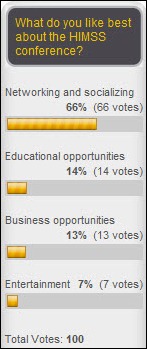





















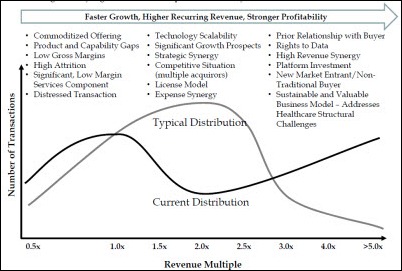























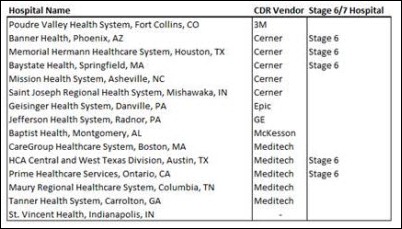
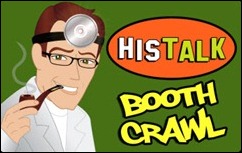

















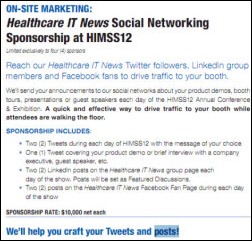
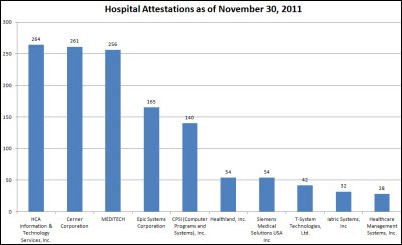
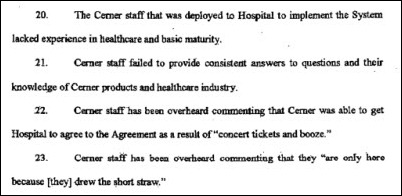









































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…