News 12/13/23
Top News

Oracle announces Q2 results: revenue up 5%, adjusted EPS $1.34 versus $1.21, beating earnings expectations but falling short on revenue. CEO Safra Catz said the former Cerner business, acquired for $28 billion in June 2022, produced “a drag on Oracle growth.”
Shares dropped 12% on Tuesday as investors became concerned about the company’s two straight quarters of disappointing cloud revenue.
From the earnings call:
- Total revenue for the quarter grew 4%, but would have increased 6% excluding the contribution of the former Cerner.
- Catz once again mentioned the imperative to “drive Cerner profitability to Oracle standards.” She says that Cerner’s impact on Oracle’s growth will be “sort of negative one to two points” this fiscal year, then it will end.
-
Chairman and CTO Larry Ellison says that half of Cerner Millennium customers will move to Oracle Cloud Infrastructure by February. He adds that a rewrite of Millennium will be completed next year and that HealtheIntent is now full SaaS.
Ellison says that all Millennium applications will be moved to OCI and will switch to subscription pricing. - He adds that Millennium is being upgraded and modernized “one piece at a time” and will be extended via applications for public health, pharma, and hospital inventory and workforce management as Oracle goes after a bigger piece of the healthcare ecosystem.
- Ellison says in responding to an analyst’s question about generative AI that it can create a patient visit summary from the conversation without using a human scribe, which he says “has shocked a great many people.”
Reader Comments
From Oracool Not: “Re: Oracle. The earnings report is not good news for whatever is left of Cerner.” I said a week ago that it would get ugly if ORCL shares reacted negatively to financial news that could be attributed in any way to the former Cerner business. The CEO’s reaction to Tuesday’s revenue miss was even more direct than I would have expected, where she threw Cerner under the bus for being an underperforming drag on company revenue. Given Wall Street’s quarter-by-quarter fixation and Oracle’s competitive AI and cloud battles with powerhouse tech companies, the obvious answer would seem to be cutting Cerner costs even more, and about the only ways that companies can do that is to reduce headcount, sell real estate, discontinue or sell lower-margin business, and reduce R&D. All of these actions are good for investors and bad for customers.
From Slambob: “Re: Health Gorilla. Co-founder and Chief Strategist Sergio H. Wagner has been relieved of his position and board seat following layoffs of 44% of the workforce and missing two consecutive quarters by more than 80%.” Wagner’s LinkedIn shows that he left the company this month. Health Gorilla was just named as one of the five initial QHINs.
From Banzai Bill: “Re: training doctors. Ask readers how they would shorten the training for primary care doctors.” I’ve asked Dr. Jayne to weigh in and invite physician readers to respond as well. The issues that come to my mind:
- Schools love to collect tuition and the post-graduate donations of physician graduates, but is it really necessary to earn a four-year degree and then attend a four-year medical school before beginning years-long hands-on training?
- Given the speed at which medical knowledge becomes obsolete and how little of it is used by the time a PCP reaches mid-level practice, would it be better to shorten the pre-practice education while moving to continuous learning in a CME-type model?
- Endless amounts of vetted medical data is available electronically and potentially by AI. Is rote memorization of a subset of that same information a waste of time?
- How much could the eight-year classroom time of graduate medical school – before another three or more years of residency – be shortened to create the same outcome?
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Fruit Street files a $25 million lawsuit against former partner Sharecare, claiming that the company violated the terms of their agreement by launching its own diabetes prevention program rather than continuing to offer Fruit Street’s solution to its members. Both companies offer digital health and wellness programs to employers and payers. Sharecare, meanwhile, contends that Fruit Street owes it $3 million. I had a lot to say – none of it good, but all of it fun reading – about Fruit Street in 2014 and 2021.
Private equity firm KKR opens talks to acquire a 50% stake in healthcare payment and analytics software company Cotiviti from Veritas Capital in a deal that would value the business at between $10 billion and $11 billion. Veritas, which took Cotiviti private in 2018 at a $5 billion valuation, rejected a similar deal from Carlyle Group earlier this year. KKR has invested in such healthcare technology companies as Zeus Health, Clarify Health Solutions, and Therapy Brands.
Data and generative AI company ConcertAI will acquire American Society of Clinical Oncology subsidiary CancerLinQ, which offers real-world oncology data and quality-of-care technology services.
Kaiser Permanente lays off 115 IT employees, 65 of them in Northern California.
Sales
- WellSpan Health (PA) will use Arcadia’s data analytics software to enhance its value-based care efforts.
- Nascentia Health (NY) will implement the Biofourmis Care remote monitoring and care management platform as a part of its new care-at-home programs.
People

Tushar Hazra, PhD (EpitomiOne) joins Parker Health as CTO.

UC San Diego Health names Karandeep Singh, MD (Michigan Medicine) as its first chief health AI officer.



Eagle Telemedicine promotes Jason Povio to CEO. He takes over from Talbot “Mac” McCormick, MD who will take on the role of chief physician executive. CFO Timothy Horton will take on the additional title of EVP.


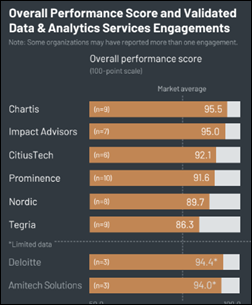
Impact Advisors hires John Lanari (Nordic) and Kristi Lanciotti, MBA (Optimum Healthcare IT) as VPs.

Howard Landa, MD (Sutter Health) joins Adventist Health as CMIO.

VCU Health hires Jeffrey Kim, MD (Loma Linda University Health) as CMIO.
Announcements and Implementations

Riverwood Healthcare Center (MN) will go live on an OCHIN-hosted Epic system next month.

Phelps Health (MO) begins offering virtual urgent care through KeyCare’s Epic-based technology.
Darena Solutions, Leidos, and SLI Compliance launch a verification process for AI applications that use SMART on FHIR to integrate with EHRs.
Mitre, the independent trusted third party for the FDA’s voluntary Medical Device Information Analysis and Sharing (MDIAS) program, announces that Atrium Health has signed on as its first health system member.
Government and Politics

ONC and The Sequoia Project officially recognize KONZA National Network, EHealth Exchange, Epic Nexus, Health Gorilla, and MedAllies as QHINs.
A Verato-commissioned survey of 197 executives finds that two-thirds of healthcare organizations aren’t ready to meet Cures Act requirements such as sending electronic patient activity notifications, obtaining consent for sharing data, managing infrastructure for secure information exchange, and sharing patient-level information with patients and other healthcare organizations. Nearly all expect to receive more data requests, and more than half expect patient data-matching to be a major problem.
A congressional investigation finds that chain drug stores are handing over patient records to police and government investigators who present a subpoena rather than a judge-approved warrant. Legal experts raise concerns that chain stores share prescriptions across all locations, creating a national “digital trail” that could be used against patients or pharmacies by states such as Texas, which has threatened to file criminal charges related to the mailing of abortion-inducing drugs to state residents.
Other

London Health Science Centre officials come under fire for spending $50,000 to send 13 IT staff to Oracle Health and Oracle CloudWorld conferences in Las Vegas last September. The Canadian healthcare provider, which is in the midst of a staffing shortage and faces a $76 million deficit, is already under government investigation for spending $470,000 to send staff to conferences in Portugal, Australia, and the UAE.
Sponsor Updates
- Frost & Sullivan recognizes Inovalon’s One real-world data and analytics platform with its 2023 North American Product Leadership Award.
- Agfa HealthCare supports Leeds Teaching Hospitals in the UK in its education initiative.
- CereCore releases a new podcast, “Ways to Overcome the Gap Between IT and Physicians.”
- Consensus Cloud Solutions achieves HITRUST risk-based, two-year recertification.
- Konza names Katy Brown director of marketing.
- EClinicalWorks announces its intent to become a QHIN.
Blog Posts
- Ways to Overcome the Gap Between IT and Physicians (CereCore)
- Leveraging Automation to Manage the No Surprises Act Dispute Process (AGS Health)
- Ripe for automation: How generative AI can enhance patient care (Arcadia)
- Meet the Clinician – Tiffany Kibbee (Ascom)
- A proven approach to reducing patient falls while driving staffing efficiencies (AvaSure)
- 1Clearsense Empowers Healthcare Organizations Across Cloud Environments (Clearsense)
- Active Incident Response Planning: Find It, Fix It, and Go Forward (Clearwater)
- You Can Have Both! How to Maintain Your Cybersecurity Framework While Undergoing Digital Transformation (CTG)
- 5 of the Hottest Digital Health Trends Predicted to Skyrocket in 2024 (Dimensional Insight)
- Reflecting on Progress: A Review of the Healthcare Technology Industry in 2023 (Direct Recruiters)
- Happy Culture, Happy M&A: Strategies for a Successful Cultural Merge (Divurgent)
- 3 Ways to Optimize Your Epic EHR (DrFirst)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.
































Re: Anthropic CEO human lifespan prediction Yeah, this isn't gonna happen. Not in the timeframe suggested, AI won't be involved,…