Monday Morning Update 2/10/25
Top News
The FDA warns users of diabetes devices — including continuous glucose monitors, insulin pumps, and automated insulin dosing systems — that critical alerts may be missed due to their phone settings.
Reported issues include misconfigured app permissions, use of “Do Not Disturb” or focus modes, apps going to sleep from inactivity, Bluetooth connections altering volume settings, and OS updates that are incompatible with the device’s app.
Reader Comments
From P.S. “Re: MyChart. A friend was looking for results for her daughter from a hospital that went live on MyChart in February. MyChart pulled up another patient’s records with their name, birthdate, and medical record number. Has anyone seen this or is it a one-off? I am interested because we are moving to Epic soon at my hospital.” I’m guessing that it’s a problem with the source system that sent the results to Epic rather than Epic itself. I say that because Googling “mychart wrong patient” brings up a few examples, most commonly attributed to an outside lab or practice and a hospital error in patient matching. Readers, have you ever seen someone else’s information in your MyChart?
From Adhesion: “Re: Oracle Health non-compliance with Section 508 disability requirements. How did the VA miss that federal requirement?” The VA should have been aware of Section 508 compliance given its long history with its previous patient portal My HealtheVet, which it boasted was fully compliant. However, federal software accessibility compliance is often more aspirational than fully realized because it’s a lot of work to retrofit support for assistive technologies and keyboard-only operation. Supposedly around 75% of software that is used by the federal government isn’t fully compliant. Related: Epic was sued a few years ago by a blind advocacy group who said that disabled people could no longer perform their jobs when their employer went live with Epic, but the case was dismissed and it addressed only employees, not outside users. Epic demonstrated Nuance-powered voice navigation at HIMSS17 that it said would meet the requirements for Section 508 compliant self-scheduling, but that was part of the VA’s MASS scheduling system that the VA walked away from in choosing Cerner.
HIStalk Announcements and Requests
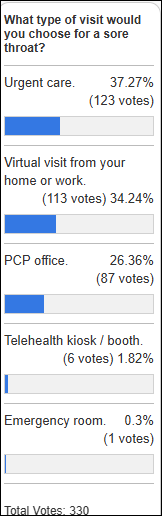
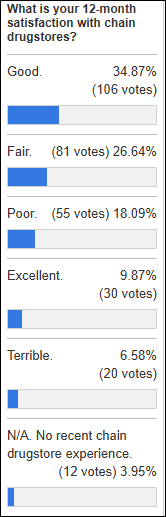
Sore throat probably wasn’t a great choice for a treatment venue preference poll given the strep swab confounder, not to mention that self-managing symptoms is also an option.
New poll to your right or here: How did you schedule your most recent non-emergency, in-person medical encounter? I listed the options that I could think of, but it’s likely I missed some.
A long-term sponsor will soon be vacating the stratospheric ad aerie way up there at the top of the column because they’ve been acquired. New or upgrading sponsors, get in touch with Lorre to move up there to the penthouse, even in time for the HIMSS conference if you are ready.

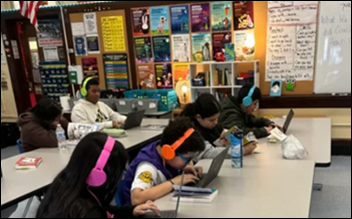
Dr. H from Bronx, NY provided an update to a reader’s donation that funded his Donor’s Choose request for help covering the $150 cost of having a PBS documentary filmmaker conduct a virtual workshop and screening for his early college class. He says, “The presentation and workshop have made an incredible impact in the classroom. The students have been working on short films of their own creation and direction. Students have also been composing their own film music on keyboards. Students computer literacy has improved with greater exposure to the workshop. We will have a screening in May where every student screens their film shorts for the entire school and local community.” Health system executives, technologists, and radiologists can help fund similar projects by completing this quick AI purchasing survey, which triggers a donation from Volpara Health.
Sponsored Events and Resources
Instant Access Webinar: “Successfully Navigating Post-Acute Rev Cycle Challenges.” Sponsors: Inovalon and KanTime. Presenters: David Swenson, senior manager of sales engineering, Inovalon; Lucy Lopez, VP of product management, KanTime. Learn how to speed up your revenue cycle processes and avoid the common RCM and eligibility errors that cause delays and denials. Discover strategies to boost your bottom line: streamline eligibility verification, simplify complex processes, and optimize denial management for improved cash flow.
Instant Access Webinar: “How AI Addresses Resource Constraints Within Identity Data Management.” Sponsor: Rhapsody. Presenters: Lynn Stoltz, MS, director of product management, Rhapsody; Drew Ivan, MS, chief architect, Rhapsody; Michelle Blackmer, chief marketing officer, Rhapsody. Discover how to overcome the toughest challenge in identity data management: resource constraints. The presenters will cover how Rhapsody EMPI with Autopilot solves resource challenges like limitations in time, talent, and budget; Reduces costs and risks associated with inaccurate data; and boosts identity data accuracy through 98% decision-making precision.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock

Teladoc Health shares popped on Thursday and Friday after an analyst gave it a glowing recommendation as a back door AI play, noting that shares have shed 96% of their 2021 value because of lower growth but the company still enjoys high margins and cash flow. I was surprised to learn that Teladoc has 5,600 employees.
Sales
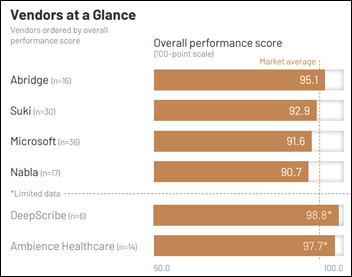
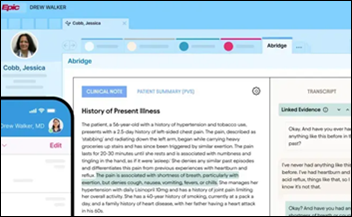
- Tanner Health will implement Abridge’s ambient documentation.
People

Bamboo Health hires Ross Armstrong, MSHA, MBA (Biofourmis) as chief commercial officer.

Stephen Fischer, MD, who developed the SpringCharts primary care EHR 25 years ago, died last week at 68.
Government and Politics


Health tech is represented on Elon Musk’s DOGE team. Industry long-timer Amy Gleason most recently worked for primary care operator Main Street Health and the White House’s US Digital Service. Brad Smith is chairman and CEO of Main Street Health, co-founder and former CEO of Aspire Health (sold to Anthem / Elevance in 2018), and co-founder and former executive chair of CareBridge (sold to Elevance in October 2024 for $2.7 billion). Smith also ran CMS’s Center for Medicare and Medicaid Innovation from 2020 to 2021.
Sponsor Updates
- Vyne Medical announces the expansion of its cloud fax services and email-to-fax technology in a major academic medical center.
- Nordic celebrates its 15th anniversary.
- Hearst Health-owned care and membership management software vendor MHK will integrate its CareProminence platform with Findhelp’s closed-loop social services referral system.
- Nym publishes a new guide, “10 Questions to Ask Autonomous Medical Coding Vendors.”
- Prominence Advisors will sponsor CDO Healthcare Exchange 2025 February 11-13 in Fort Lauderdale, FL.
- Redox prepares to launch its Shut the Backdoor Podcast about healthcare security.
- Sectra releases a new episode of its “Let’s Talk Enterprise Imaging” podcast, “Greater Manchester’s path to AI in chest x-ray imaging.”
- Primary Venture Partners recognize SmarterDx co-founders Michael Gao, MD and Josh Geleris, MD as startup honorees at the NYC Tech Awards.
- Waystar will exhibit at the EClinicalWorks Day Show February 12 in Dallas.
- The Overland Park Chamber of Commerce honors WellSky Chairman and CEO Bill Miller with its Nova Award for fast-growing and innovative companies.
Blog Posts
- 2025 Readiness: 8 Enhancement Considerations for Human Services & Post Acute Teams (Netsmart)
- Addressing cybersecurity challenges in rural healthcare (Nordic)
- Top 2025 Healthcare Trends and Predictions (PerfectServe)
- Should You Build or Buy Your Consumer Experience Orchestration Platform? (Praia Health)
- Building Better Community Care with Tailored Solutions (TruBridge)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Contact us.












































































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…