Monday Morning Update 8/7/23
Top News
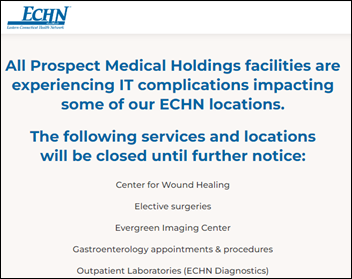
A ransomware attack on Prospect Medical Holdings disrupts or shuts down its 16 hospitals and 165 outpatient locations across five states.
The company’s hospitals are in Southern California, Connecticut, Pennsylvania, and Rhode Island. They include those of health systems Crozer-Keystone, Eastern Connecticut Health Network, and Waterbury Hospital.
Prospect Medical Holdings, which serves mostly low-income patients who are on Medicare or Medicaid, made headlines in 2020 as investigative reports detailed its operational challenges under private equity owners who made hundreds of millions of dollars by loading the acquired hospitals with debt and selling their real estate. Chairman and CEO Sam Lee made $128 million.
The FBI is investigating the cyberattack.
Reader Comments
From Indecent Explosure: “Re: HIMSS annual conference. I think that not only was the timing right for HIMSS to lighten its load and rebuild its finances, the conference will improve under outside expertise.” I agree. HIMSS did an admirable job, at least through 2019, of running a logistically complex conference that generated most of its revenue. However, it tarnished the HIMSS brand as an out-of-control boat show with few actual buyers as its CIO audience was poached and some attendees shifted to hipper, glitzier conferences that were more fun, held in more interesting cities, and that blurred the line between education and vendor prospecting. Informa, like HIMSS conference competitor HLTH, won’t have to strike a balance between commercialism and thought leadership and can instead focus on attendee and exhibitor satisfaction that is measured purely by attendance, exhibitor count, and event profit. HIMSS will need to figure out its new, somewhat diminished role, especially since the educational components were among the conference’s most obvious weaknesses. What I expect we’ll eventually see:
- More conference-sponsored social events, lunches, and entertainment.
- A better conference app that is geared around connecting exhibitors and attendees before, during, and after the conference.
- Better marketing and lead retrieval tools for exhibitors.
- Better support for live-streaming.
- A stronger emphasis on one-on-one vendor meetings in the hosted buyer format to give exhibitors more bang for the buck. Informa’s mission across its many conferences is to connect people to do business.
- The triumphant return of carpet to the exhibit hall aisles.
From Get ‘er Done: “Re: HIMSS and Informa. Did you notice in the HIMSS video interview that the terms of the conference sale haven’t been finalized?” I did notice that. Ken McAvoy, president of Informa’s South Florida Ventures division that will oversee the HIMSS annual conference, said this about a potential conference name change in a HIMSS interview last week: “Hal said we may tweak the name. We’re not changing any name. That ain’t happenin’ … I probably would normally say that only after the negotiations are over, for a number of different reasons.” Informa’s July 27 financial report lists the HIMSS conference under acquisitions, but refers to it as “exclusivity to acquire.” HIMSS coyly refers to the deal as a “strategic partnership” while providing no specifics. I don’t know why Informa was so anxious to publicly refer to an acquisition that has not been consummated and why HIMSS wasn’t better prepared to spin the news more quickly.
From JD: “Re: Optum and UHC. Massive layoff Thursday.” Unverified, but widely reported on TheLayoff.com by folks who say that more cuts are coming through August 10. Specifically named was OptumRx, which simultaneously brought over Patrick Conway, MD as CEO from Optum Care Solutions. His LinkedIn indicates that the prescription benefit manager has 30,000 employees and generates $110 billion in annual revenue.
HIStalk Announcements and Requests
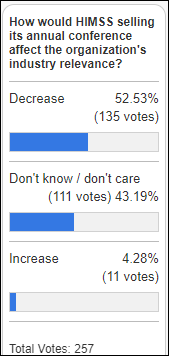
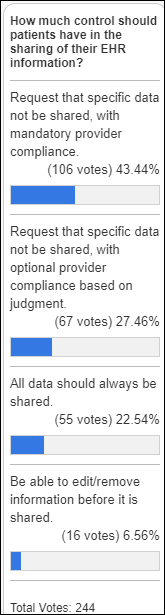
Few poll respondents predict an increased HIMSS relevance following the sale of its annual conference. Art Vandelay expressed some slightly contrarian ideas about how getting out of the conference business might end up making HIMSS more relevant and useful:
- Provide educational sessions that aren’t vendor commercials or that feature minor achievements that can’t scale to the industry as a whole.
- Use the research community connections of Informa’s Taylor and Francis, which publishes books and academic journals.
- Create less obtrusive policies.
- Consider other conference host cities.
- Provide executive and leadership tracks that would entice decision makers to attend.
New poll to your right or here: Will AI-powered systems diagnose and treat patients without direct, real-time physician involvement? See Scott Gottlieb, MD’s recent op-ed piece to learn why he thinks that will happen sooner rather than later. I specifically say “physician” since use of such a system might be supervised by PAs, nurse practitioners, or other non-physician clinicians.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Virtual primary care technology vendor TytoCare raises $49 million in growth funding, which it will use to further integrate AI into its Home Smart Clinic for diagnostic support and remote exam assistance for chronic care management.
People

Glenn Yarbrough, MBA (CommonSpirit Health) joins field care solutions vendor Coordinista as chief information and technology officer.
Announcements and Implementations
Google rolls out a new dashboard to alert users when their personal information – including medical records – appears in search results links. The enhanced “results about you” tool also allows clicking a link to remove results that contain an email address, phone number, or home address, although the company notes that the information is only removed from Google searches, not the source website or other search engines.
Government and Politics
The Drug Enforcement Administration will conduct listening sessions on September 12-13 to gain input about prescribing controlled substances via telemedicine without requiring an in-person evaluation.
Privacy and Security
Brigham and Women’s Hospital alerts 1,000 research study participants that someone used the free, online Tableau Public visualization tool to create and share graphs, which were later found to have included a publicly accessible link that displayed patient names, addresses, diagnoses, lab results, medications, and procedures.
Other
Lexington Regional Health Center (NE) decides to review rather than fire its CEO for failing to disclose to its board “a matter of potential litigation, negotiation, and resulting six-figure settlement” involving IT, which was described as “not stable.” The board secretary and treasurer referred to a recently implemented unnamed computer system and cybersecurity issues that have caused outages of computer and telephone systems. LRHC signed a contract with Cerner in October 2019
Sponsor Updates

- West Monroe employees volunteer at the Downtown Women’s Center in Los Angeles.
- Surescripts Chief Marketing and Customer Experience Officer Melanie Marcus joins the Exceptional Women Alliance.
- NeuroFlow releases a new Bridging the Gap Podcast, “Child Psychologist and Drexel Department Head Dr. Brian Daly Explores the Adolescent Mental Health Crisis.”
- KLAS Research recognizes Nym Health’s medical coding engine with a 100% customer satisfaction score in its latest Emerging Solutions Spotlight report.
- Waystar will exhibit at the HFMA Region 8 Mid-Summer America Institute August 7-9 in Minneapolis.
Blog Posts
- 3 Stats Highlighting the Impact of Healthcare Analytics on Providers (Clearsense)
- Meeting people where they are: Opioid management in the heartland (Meditech)
- The fog of more: Price transparency will increase health systems’ competition for patients (Nordic)
- Success with Specialists Training Specialists (Optimum Healthcare IT)
- From Staffing to Billing: Is Your Pharmacy Ready to Expand its Clinical Services? (OmniSys)
- Nurses of Note 2023: The District School Nurse (PerfectServe)
- Becoming great: 5 common characteristics of the best hospitals (Spok)
- Visage Breast Density AI Classifier – From Conception to Routine Use (Visage Imaging)
- Rapid Cycle Improvement Programs Deliver Speedy Results, Require Significant Effort (Zynx Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


































I've figured it out. At first I was confused but now all is clear. You see, we ARE running the…