Top News
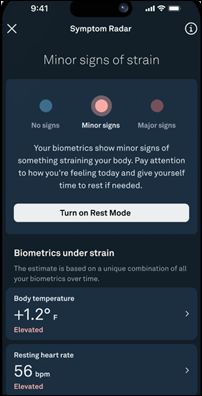
Apple CEO Tim Cook repeats his previous assertion that health apps will define the company’s legacy.
Cook says in an excellent Wired interview that enabling AirPods as hearing aids for moderate hearing loss is “the democratization of health.”
He summarizes that Apple is “pouring all of ourselves” into health, such as real-time biometric data analysis.
HIStalk Announcements and Requests
Two former HIStalk sponsors rejoined the fold this week, in both cases because employee turnover had left them unaware that they had unintentionally departed in the first place. Other potential prodigal sons and potential new sponsors can contact me directly and I’ll either answer your inquiry myself or send you over to Lorre. I can also confirm your sponsorship status if you aren’t sure.
Listening: Teenage Fanclub and 311, both of which having been playing guitar rock for 25 years. I discovered them from my recent infatuation with REM and my request to ChatGPT to find other bands that I would like. I’ve been watching REM concert videos for at least a half hour every night to catch up on their body of work, from which I note the contributions of retired drummer Bill Berry (he played multiple instruments and added another layer of harmony with Mike Mills in addition to orchestral drumming), replacement drummer Bill Rieflin (he died in 2020 at 59), and “fifth member” Scott McCaughey (I can’t get enough of his licks in the live version of one of my favorite REM songs “Supernatural Superserious,” which also has a fine contribution by Rieflin). My favorite concert video is from an appearance in Athens, Greece, although they did a great show at the other Athens in Georgia at the 40-Watt Club. I would choose REM as the best rock band in American history, perhaps nostalgically since now the “band” concept is passé in favor of computers, collaborations, and outsourced songwriting.

If you attended the ASTP annual meeting in person this week, let me know what you thought was important or interesting. They livestreamed it, but the hallway conversations are the good stuff.
Reader Vicki’s generous donation on Giving Tuesday allowed me to stack up a bunch of matching funds, including the matching money that was donated by my Anonymous Vendor Executive, to fully fund these Donors Choose teacher needs:
- Whiteboards and equation solving supplies for Ms. D’s middle school class in Kerens, TX.
- Headphones for Ms. G’s elementary school class in Pharr, TX.
- Math learning tools for Ms. C’s elementary school class in Brooklyn, NY.
- STEM learning kits for Ms. C’s elementary school class in Chino, CA.
- Geometric transformation supplies for Ms. S’s middle school class in Chicago, IL.
- STEM kits for Ms. B’s kindergarten class in Sacramento, CA.
- Headphones for Ms. N’s elementary school class in Greensboro, NC.
- Podcasting equipment for Ms. P’s high school Podcast News class in Santa Rosa, NM.
- Headphones for Ms. J’s elementary school English as a Second Language class in Fridley, MN.
- A printer for college applications for Ms. N’s high school class in Hollywood, FL.
- Motivation awards for Ms. S’s elementary school class in Ontario, CA.
- Research project tools for Ms. P’s middle school class in New York, NY.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Black Book Research lists nine countries that its expert panel says are poised for significant EHR adoption in 2025.
Aya Healthcare, which operates a travel nurse staffing service and job-matching website, will acquire staffing company Cross Country Healthcare for $615 million in cash.
Marketing firm Supreme Group acquires health tech and life sciences PR and marketing agency Amendola Communications. Amendola will keep its name and founder Jodi Amendola will remain as president. I interviewed her a month ago.
Publicly traded Embecta, which earned FDA clearance for its first insulin patch pump in September with plans to add a dosing algorithm, will lay off 118 employees and end that program to focus on its core business of making pen needles and insulin syringes.
Sales
- Moorfields Eye Hospital NHS Foundation Trust will implement Meditech Expanse.
People

Frank Forte, MBA (Anatomy_IT) joins EnableComp as CEO.

Chris Paton, DPhil, MBA is named editor in chief of BMJ Digital Health & AI.

Retired Vanderbilt informatics professor and health tech pioneer Edward Shultz, MD, MS died last week at 76.
Announcements and Implementations
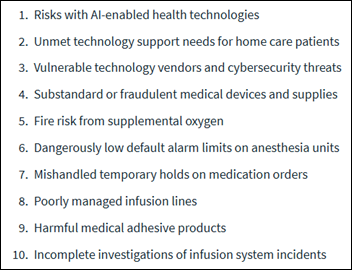
ECRI names the use of AI in healthcare as the most significant health technology hazard for 2025. The patient safety non-profit emphasizes the need to balance innovation with privacy and safety.
Vanderbilt University Medical Center’s IT department goes live on alert tool that can send messages directly to the computer displays of employees who will be affected by upcoming changes. The software is from Lakeside.
University of Central Florida offers students in its Health Informatics and Information Management BS degree program training on Epic, with materials and a simulated environment provided by Orlando Health.
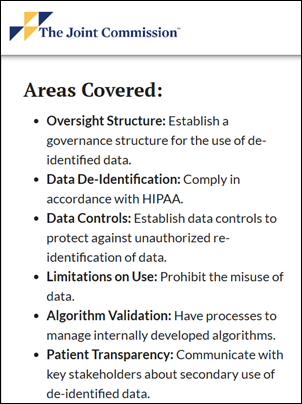
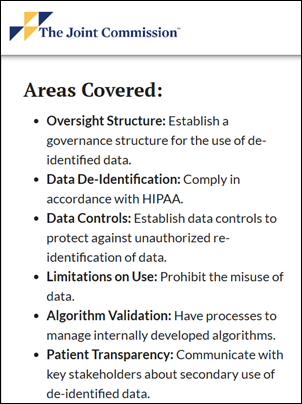
The Joint Commission recognizes Inova as the first health system to earn its voluntary Responsible Use of Health Data certification.
Government and Politics
The Indian Health Service becomes the first federal health agency to go live on TEFCA, selecting EHealth Exchange as it designated QHIN.
FDA publishes recommendations for a smoother process for manufacturers to update their AI-enabled devices.
ASTP issues its first AI contract to Audacious Inquiry, a PointClickCare company, for technology to improve efficiency in its core areas. The reasoning behind using the technology of a care collaboration company to automate back-office government processes wasn’t stated.
Privacy and Security

Mount Nittany Health offers to pay $1.8 million to settle a lawsuit over its use of pixel tracking software on its website and patient portal.
Kevin Holland dives into Meta policy changes that will affect healthcare and health tech advertisers, as the company will restrict tracking of form fills and retargeting based on medical information starting in January. He concludes that condition-specific products or marketing campaigns will face significant restrictions and that direct conversation tracking will disappear as a campaign metric.
The Sequoia Project publishes a free Information Blocking Rule educational toolkit.

Three-hospital PIH Health takes its systems, network, and phone system offline following a ransomware attack Sunday.
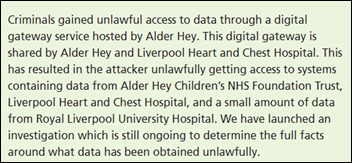
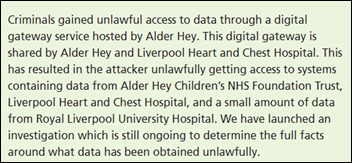
In England, two NHS trusts continue their restoration of systems following ransomware attacks.
Other
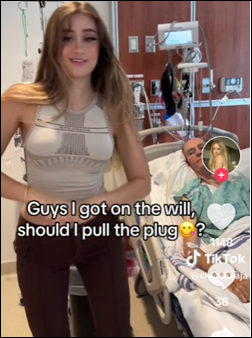
Only mildly health tech related, but eye-catching as a societal observer. A 22-year-old OnlyFans model earns Internet scorn after sharing a TikTok of herself in the hospital room of her 85-year-old boyfriend, dancing and joking about speeding up her inheritance. She describes their relationship as, “He takes me to Cartier, I take him to pound town.” Meanwhile, a fellow OnlyFans adult content creator has made $43 million so far this year, leading me to ponder society’s valuation of a 20-year-old — who claims that she is a devout Christian and a virgin, which I can see would draw a certain demographic whether accurate or not — as equal to a couple of hundred doctors. She says that one smitten follower has made it rain nearly $5 million for her in the past few months.
Sponsor Updates

- Healthmonix team members support Ann’s Heart in Phoenixville, PA.
- Agfa HealthCare integrates Rad AI’s reporting and FHIRcast solutions with its enterprise imaging platform.
- Meditech Alliance triples its membership to 37 solution members whose products complement, enhance, or extend Expanse.
- FindHelp welcomes CenCal Health, Maryland Physicians Care, BronxCare Health System, and Central Iowa Shelter & Services to its network.
- Commure’s Augmedix achieves Oracle Validated Integration with Industry Healthcare Expertise for its full suite.
- Five9 announces that SVP Jake Butterbaugh has been named a Channel Futures Top UC/Contact Center Leader for 2024.
- Fortified Health Security names William Hicks EOD security engineer.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Contact us.





































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…