News 5/19/23
Top News
The VA and Oracle Cerner complete their scheduled five-year contract renegotiation.
The VA’s next five-year renewal period will be changed to five, one-year terms.
The revised contract will also include stiffer financial penalties if the Oracle Cerner system fails to meet specific performance metrics.
Reader Comments
From MmSEC Observer: “Re: Veradigm. This is how private equity firms steal shareholder value in taking public companies private. They are pillaging companies that misstep software accounting rules. See Avaya.” Publicly traded digital communications vendor Avaya filed bankruptcy a few weeks ago in a deal that allowed two private equity firm lenders to take control of the company, leaving Avaya’s shareholders with nothing. The company’s problems came to light after executive changes and delays in filing earnings reports that followed a previous bankruptcy filing in 2018. A bondholder class action lawsuit accuses Avaya’s board of “massive fraud” in misleading investors. MDRX shares have lost 34% in the past 12 months versus the Nasdaq’s 4% gain, valuing the company at just over $1 billion.
HIStalk Announcements and Requests
Reminder: if your company sponsors HIStalk and is participating in the MUSE conference, give me details for my conference guide.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
RCM automation vendor Adonis raises $17 million in a Series A funding round.
Virtual care management platform vendor HealthSnap raises $9 million in a Series A funding round.

CVS Health will close the clinical trials business that it launched in May 2021. The service provided technology-drive patient recruitment, real-world data collection, and clinical trial delivery.
A Business Insider piece says that Oracle is “crushing morale” among former Cerner employees since its $28 billion acquisition of the company by these actions:
- Laying off 3,000 of 28,000 employees.
- Freezing raises and promotions.
- Vacating Cerner’s former buildings in Kansas City.
- Sidelining former Cerner CEO David Feinberg to a “ceremonial” role as chairman of Oracle Health.

Doximity reports Q4 results: revenue up 18%, adjusted EPS $0.20 versus $0.21, beating expectations for both. Shares dropped 6% on the news to their year-ago price, valuing the physician networking company at $6 billion.

NextGen Healthcare reports Q4 results: revenue up 18%, adjusted EPS $0.31 versus $0.19, beating analyst expectations for both but sending shares down on the news. NXGN shares have lost 16% in the past 12 months versus the Nasdaq’s 4% gain, valuing the company at $1 billion.
Sales
- Gundersen Health System will implement cloud-based Visage 7 Enterprise Imaging Platform in its seven hospitals and 65 clinics.
- SUNY Downstate Health Sciences University will implement Memora Health’s care delivery platform.
Announcements and Implementations

Executives for Health Innovation, which was known as EHealth Initiative through 2021, will shut down, 22 years after it was founded.
UF Health will acquire Flagler Health+ (FL), with one of Flagler’s goals being to upgrade its IT systems. Flagler chose Allscripts Sunrise in 2011, while UF Health uses Epic.
UnitedHealthcare takes heat for its decision to require prior authorization for colonoscopies starting June 1, a move that left the American Gastroenterological Association “profoundly alarmed and disappointed.” The insurer says approval will be immediate for procedures that follow evidence-based guidelines and within two days otherwise.
OpenAI launches ChatGPT for the IPhone on the Apple App Store.
Government and Politics
A judge orders Theranos founder Elizabeth Holmes to report to prison to begin serving her 11-year sentence for investor fraud, rejecting her last-minute bid to remain free while she appeals. Holmes and former Theranos COO Sunny Balwani, who is serving a 13-year sentence, were also ordered to pay $452 million in restitution to 12 defrauded investors and former partners Walgreens and Safeway.
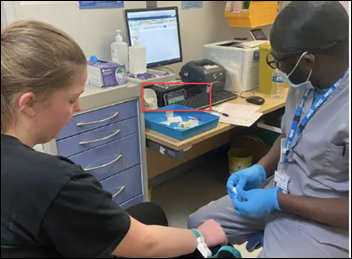
An Oklahoma doctor and pharmacist are charged with manslaughter in the death of a 75-year-old rehabilitation center patient from a methotrexate overdose. The physician admitted that he didn’t order correctly, while an investigation found that the pharmacist ignored the computer’s red-letter warning that the prescribed dose of 20 mg of methotrexate daily for seven days – instead of the intended 20 mg every seven days – was excessive.
Privacy and Security
A proposed Federal Trade Commission order would bar ovulation tracking app Premom from sharing user health data in charging the company with making unauthorized disclosures to third parties when its privacy policies claimed it doesn’t. The company will also pay $200,000 in federal and state fines.
Related to the Premom order, FTC seeks comments on its intention to extend the Health Breach Notification Rule to cover health apps.
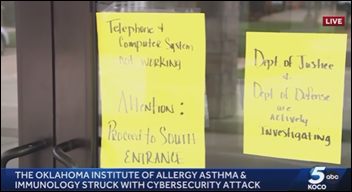
An Oklahoma allergy clinic shuts down permanently following a cyberattack. The clinic’s physician owner says all of the practice’s technology was impacted when she and her husband downloaded an unspecified IPhone app, locking them out of all of its systems even as patients were receiving appointment reminder text messages. The owner says that the FBI, Department of Justice, and Department of Defense are investigating, but the FBI says it has received no reports about the issue. Social media comments claim that the same doctor abruptly shut down other clinics, including a medical spa, for reasons unrelated to technology.
Sponsor Updates
- Divurgent releases a new episode of The Vurge Podcast, “Digital Mental Health Insights: Breaking the Stigma with Data.”
- Fortified Health Security names Candace Manning (Lifeway) client success manager.
- Loyal wins Best Patient Registration and Scheduling Solution in the MedTech Breakthrough Awards.
- Consensus Cloud Solutions partners with Hyland Software to offer a digital cloud fax solution that integrates with OnBase.
- AvaSure, which offers acute virtual care and remote safety monitoring solutions, establishes a chief nursing executive advisory board with 10 inaugural members.
- CereCore will recruit and train hundreds of EHR and clinical informatics staff over the next one to three years to support HCA Healthcare’s deployment of Meditech Expanse.
- Nordic releases a video titled “The Download: Valuing IT as an Asset to Improve Patient Care.”
Blog Posts
- What does Consensus CTO, Jeffrey Sullivan, have to say about Generative AI? (Consensus Cloud Solutions)
- Can AI Replace Your Doctor? (Dimensional Insight)
- HIPAA: 4 Enforcement Discretions Expire with End of PHE (Experity)
- The key to better, faster innovation: Healthcare data standardization (Intelligent Medical Objects)
- Demystifying Compliance: How Interoperability Solutions Can Simplify Healthcare Regulations (Medhost)
- In Healthcare, an AI Pause Isn’t Feasible. But, an AI Strategy Is. (Lucem Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.






























I've figured it out. At first I was confused but now all is clear. You see, we ARE running the…