Frank Harvey, RPh, MBA is CEO of Surescripts.

Tell me about yourself and the company.
I am privileged to have been in healthcare for over 40 years now. Initially as a practicing pharmacist, then in the life sciences industry with Eli Lilly and Hoffman-La Roche, and with a number of health technology companies servicing healthcare. I was CEO of Liberty Medical, which was the largest diabetic testing supply company in the country. I had the privilege of being CEO of a company called Mirixa, which is a medication therapy management technology company. I ran my own venture fund for about three years. Now I have the privilege of being on the Surescripts team as CEO.
Surescripts is a trusted health information sharing company. We support the movement of clinical data between clinicians, physicians, nurses, and pharmacists across the nation. We are the e-prescribing backbone for the country. Our 24 billion transactions that we do in the movement of clinical data across our networks each year empowers clinicians to not only e-prescribe, but to get price transparency information and to make sure that they are making the right choice for each patient. The medication history information that goes across our network empowers physicians to make the right medication choices based on what a patient’s history has been historically. We are a mission-driven company focused on improving healthcare, reducing the cost of care, and improving patient safety.
How do you see the big picture of interoperability and the business and clinical opportunities that it might create?
The most important thing about clinical interoperability is how it’s going to empower the clinicians to be even more effective at treating patients. It gives them the full clinical history, the important information for what they’re working with the patient on. Last year we had 24 billion transactions across our database from virtually every physician, every pharmacy, every health system, and every EHR we are connected to, across all of healthcare working together.
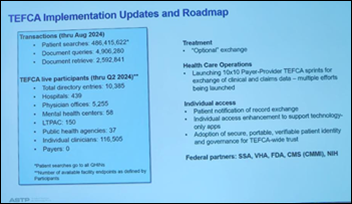
TEFCA, the Trusted Exchange Framework and Common Agreement, and the QHINs, the Qualified Health Information Networks, will make data more readily available for the clinicians to make sure they get a complete clinical record. Historically, patients move from health plan to health plan, and sometimes from physician to physician that may be on different EHRs. Many times the clinician didn’t have a complete clinical history to make the right choices. QHINs will help solve that issue and make it transparent to the treating pharmacist, physician, nurse, or physician’s assistant, giving them right clinical information that they need to make more appropriate clinical decisions for patients.
How does the use of an e-prescribing network empower patients compared to paper prescriptions?
The most effective prescription is the one that the patient will actually pick up and take. Many times historically, patients weren’t aware of the price of medication. A physician would write a prescription, the patient would take it into the pharmacy, and then it would be like, well, I can’t afford that. Pharmacists would have to take time to call back the physician’s office, or the patient would just abandon the prescription.
Real-time prescription benefit provides a number of things around transparency. It’s meant to be when the physician is right there writing the script with the patient. They can see not only the prescription that they are thinking of writing, but also the therapeutic alternatives. What medications could be used in place of that? What’s the cost of that prescription based on the patient’s benefit? What’s the cost of that prescription at different locations? Mail order versus retail versus preferred retail? All of those factors are now at the physician’s fingertips.
We have over 800,000 physicians in the US utilizing a real-time prescription benefit product. Having all of that information at their fingertips helps them make the right choice for the patient, because it’s not just a clinical decision. If the patient can’t afford the medication, there may be other medications that will be more therapeutically appropriate because the patient can actually afford to pick it up and take it.
What are the technology approaches for improving the efficiency of processing prior authorizations?
The concept around prior authorization was smart. It was to ensure that patients were taking the right medications and the right sequence to make sure they received the best treatments. Often it’s not just the most expensive medication that would be the best, but the most appropriate. There may be step therapy that a patient could go through. Since historically physicians didn’t always have complete medical records for patients, that was one additional way to help inform the treatment decisions.
What has happened with prior authorization is that it is much too cumbersome for the physicians and their offices and the pharmacies that have to delay things and step back. Most importantly, it is much too cumbersome and delays treatment for the patient. It’s really the patients that are being hurt by the delays that take place in the prior authorization process.
Fortunately, we are at the forefront of working on new technology to help solve a number of those issues. We’ve just published our pilot results with Optum and Cleveland Clinic Fairview, looking at what we’re calling no-touch prior authorization. It’s our ability to end the workflow for the physician to get that prior authorization approved while they are prescribing the medication. Because we are connected to every EHR, we have clinical history on these patients. We can reach out across those clinical records in a matter of seconds, pull that record back, and complete that prior authorization so that it goes through smoothly. The medication isn’t delayed for a couple of days because the pharmacy hasn’t received authorization.
New technology and our new advances are helping patients, most importantly, but also cutting down on clinician and staff burnout that is caused by all of this faxing, calling, and delaying work.
Are payers embracing the gold card type program, where prescribers who have history of responsible prescribing aren’t required to go through the same level of prior authorization scrutiny?
The gold card program is helpful for physicians who have proven that they always go through the right step therapy and put the appropriate medications first for their patients. It’s important since all that information is not always available to a physician and the cost of medications is extremely important to the overall system as well. It isn’t always the most expensive medication that is the most appropriate. Prior authorization was trying to solve some of the issues around that and to try to keep healthcare costs at a minimum while still providing good clinical care to patients.
Our real-time prescription benefit product shows what a patient’s coverage is, what their benefit is, and whether a product is covered or not. But in addition, our newest advances in prior authorization are showing those and filling out those electronic forms for physicians in a matter of 30 to 35 seconds in the prescribing process. That’s really freeing up a lot of time. It’s taking a lot of the burden off of the physicians having to do a lot of that work.
Physician offices have a number of people who are working on prior authorizations. Then there’s a whole host of people at the health plans and PBMs who are taking those calls and working through them as well. Creating efficiency through our new technology will help remove a lot of that provider burnout and get patients on therapy quicker.
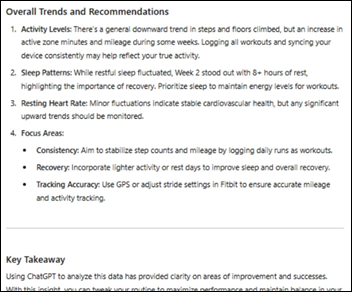
How do you build a business plan around the possibility of incorporating AI into products and strategy?
We’re just starting to scratch the surface on the benefit that AI is going to be. Surescripts technology has been built around machine learning from the beginning of the company. Generative AI carries some surprises, and caution is needed because it can have hallucinations and make stuff up if it doesn’t have the right answer. Because of that, whenever you have generative AI involved in a recommendation or decision, it has to have human intervention in there as well. It has to be checked. You have to make sure that what that generative AI is coming back with is right. You have to have human intervention in that. I don’t see that going away anytime soon.
Where I think AI generative AI is going to have the most impact is with administrative functions, prior authorization and others, where it can help pull in that information from the notes fields and from other areas to show what a patient has been on. But again, always needing that human intervention to confirm what the generative AI is coming back with.
Does your network offer new opportunities to add value or improve care?
A good network takes a long time to build. We’ve been at it now for over 20 years. The Surescripts Network Alliance is all of our partner companies across that multi-sided network working together on these hard systemic problems. These problems that we are focused on are systemic across all of healthcare. When you find a solution or come up with a solution, it helps everyone in the process, including the patient. As we continue to build out the networks, QHINs are a great example of additional networks being added to the framework. Being attached to every prescribing physician, pharmacy, health system, and EHR lets us see the value that the network can bring to the patient.
What are the technology implications of the Drug Enforcement Administration’s recent warning about the security of e-prescribing systems?
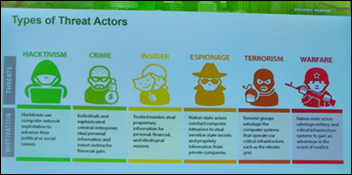
It’s a multi-pronged effort. Bad actors are getting more and more sophisticated. They are looking for new ways every day, and you have to be vigilant.
At Surescripts, it starts with the rigorous standards that it takes to become a part of the Surescripts network. We at times have heard complaints from some new health technology companies that are trying to get on our network. But once they understand that we’re responsible for protecting the security of this across the nation, and so it’s not easy to become a part of the Surescripts Network Alliance. But when you do, you’re sure that it’s at a level of security that is beyond reproach.
It’s also the standards that you put in place. At Surescripts, we follow the National Institute of Standards and Technology, NIST, Identification Assurance Level 2. This is a higher level of security than is required in general. Every health technology company and EHR on the Surescripts network has to comply with that higher standard.
We work hand in hand every week with the DEA or the FBI as they are investigating cases of prescriber fraud. Physician identities will be stolen and you’ll have somebody sending out 1,000 scripts in a matter of minutes. Our systems catch those sort of things. The tough ones are the onesies and twosies that don’t rise to the top. That’s why we have to continue to be diligent working with the pharmacy operating systems, pharmacies, the health technology vendors, and our systems to make sure that we are staying on top of that.
There will always be bad actors out there and they will always be looking for new ways. The DEA is wise to recommend that you stay vigilant around that. We require our health technology vendor partners to be vigilant and to have a standard of what’s required of their prescribers on the network. We just announced a new partnership with Clear, which will add another level of ID proofing.
As a pharmacist, how has the profession evolved and how might it change going forward?
I graduated 40 years ago. I’m a Bachelor of Science pharmacist. We had a couple of PharmDs when I was going through school, but most of them were going into hospital practice. Now every pharmacist is graduating with a PharmD. The rigor of their clinical training is beyond reproach. They are critical members of the overall healthcare team.
The other thing that is driving the need for pharmacists to become even more active is a lack of primary care providers. We know there’s going to be a shortage of about 130,000 primary care providers by 2030. Pharmacists are well equipped from a knowledge standpoint to step into that gap to be a part of that collaborative care team to help make life better for patients. That is the most significant advance I’ve seen in those 40 years, the role that pharmacists are playing as a critical part of that primary care team.
If you look three to five years in the future, I think that at most pharmacies, you’ll see pharmacists spending 70 to 80% of their time interacting with patients in that clinical interaction. Not just immunizations, but working with patients on insulin dose adjustments or with patients who have hypertension or CHF in those in-between visits when they would normally go to a primary care provider in the past where their primary care provider may now not be available.
The role of the pharmacist is going to continue to expand as the legislation expands the pharmacist’s authority. During the pandemic, the federal government stepped in with the PREP Act that allowed pharmacists to give immunizations and to be more active in a number of ways. The federal government just extended that I believe to 2029, maintaining the authority of the pharmacist to do those other clinical functions. We need to continue state by state, because it is a state-mandated or state-allowed monitoring of the practice of pharmacy and medicine. We need to have the states continue to authorize pharmacists to work across the full scope of their training, because they are critical to the care team. The physicians we speak with say they are so much more effective when there’s this collaborative care arrangement with the physicians and the pharmacist working together for what’s best for the patient.
Private equity firm TPG recently took a majority position in the company. How does that change your business?
I can’t overstate how important that is to us. We started about two years ago working with our board to say, what are the opportunities that Surescripts needs to focus on in the future? Those opportunities continue to focus on things like prior authorization, extending clinical practice for pharmacy and empowering them with the right information, and increased interoperability. All those things take a lot of financial wherewithal.
We met with almost 100 equity companies over the last two years, narrowing it down to what we believe is the finest healthcare technology-focused private equity company in the world. TPG is really there with us, enabling us, providing the financial backing that we will need to continue to not only build organically, but to look at the right acquisitions that make sense for Surescripts to add to our technology in areas that we focus.
What are complementary areas that you might consider?
We are focused on things that can help take out that administrative burden for patients, for physicians, and to help patients. Prior authorization. Thirty percent of the pharmaceutical spend goes through the medical benefit, which is another area that’s important. Also, the data and data insights as we look at 24 billion transactions a year. There’s so much value that can help with patient care in that, in the midst of all those data elements, helping us refine and look at the best recommendations that we can help make to providers on the patient’s behalf based on all the clinical data that we have. All of those are areas that TPG is excited about.
One of the things we like best about them is that we share a similar culture. We know that we’ll do very well as a company by doing good — doing good for patients, doing good for providers. In one of the first meetings we had with TPG, they echoed that we’ll do well by doing good, and the financials of the company will take care of themselves. We share that same vision of healthcare and the impact that we can have in healthcare.
What does the health tech investment climate look like?
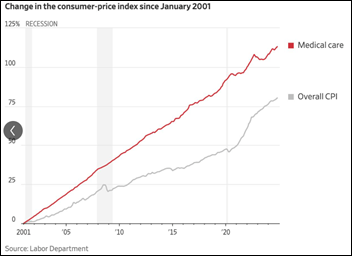
The last 18 months has been a little slower on technology investment. I think you will see that start to ramp back up again. The impact of AI in the short term is going to be less than people are stating, but in the long term, I think people are underestimating AI’s real impact on healthcare and on multiple industries. It will help us continue to reduce the cost of healthcare. The climate is favorable for that investment.
Healthcare is such a large part of our overall economy. Healthcare is still broken in a number of areas, and it needs fixing. We don’t need just little point solutions, because many times a point solution solves one problem, but it can create a problem upstream and downstream from that point solution. We need larger, systemic solutions that can solve across the whole healthcare spectrum. That’s what we’re focused on as a company.
What are your priorities over the next few years?
The most important priority is what it has been historically, which is to continue to have the best employees that you can have. I am so proud of our team, the quality of the individuals on our team, and the caring nature that our culture has. We’re really focused on what’s best for the patients and the providers, and that comes through in the quality of the work. Continuing to have the best members of the Surescripts family will always be job one for us. Then it’s continuing to partner across the Surescripts Network Alliance, which is how we will go further faster in working with all of our partners in healthcare to solve these big systemic issues.
A lot of the parts of healthcare are still broken. We need to work as a collaborative across all the healthcare technology companies, the EHRs, the PBMs, the pharmacies, the physician groups, and the health systems. Working on these problems together, we can help fix that healthcare system, take a lot of cost out of that healthcare system, and do what’s best for the patients.
Comments Off on HIStalk Interviews Frank Harvey, CEO, Surescripts

























Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…