Agfa HealthCare

Booth 5027
Contact: Kara Clarke, director of marketing and communications
kara.clarke@agfa.com
Get ready, because the power of innovation is about to take your IT work-life balance to a whole new level. At HIMSS25, discover how Agfa HealthCare Enterprise Imaging significantly reduces IT complexity for healthcare organizations with a unified platform, user-friendly interface, enhanced security, and excellent scalability. Allowing you to focus on what matters most — helping your organization deliver exceptional patient care.
Join us at our booth, 5027, for a special client series, “Peer Perspectives: Connected Imaging Solutions for IT Leaders — Integration, Imaging, Innovation — Real Stories, Real Results.” Gain insights from IT leaders just like you who have transformed their organizations with Agfa HealthCare solutions. Uncover the strategies they used to overcome obstacles and achieve impactful results. Stay engaged with an interactive Q&A after each presentation. Learn more at www.agfahealthcare.com/himss25.
AGS Health

Contact Matt Bridge to schedule a meeting.
Contact: Matt Bridge, SVP of strategy
matthew.bridge@agshealth.com
508.523.4176
AGS Health is more than a revenue cycle management company — we’re a strategic partner for growth. Our distinctive methodology blends intelligent automation with award-winning RCM services and high-touch customer support to deliver peak end-to-end revenue cycle performance and an empowering patient financial experience. We employ a team of 13,000 highly trained and college-educated RCM experts who directly support more than 150 customers spanning a variety of care settings and specialties, including nearly 50% of the 20 most prominent US hospitals and 40% of the nation’s 10 largest health systems. Our thoughtfully crafted RCM solutions deliver measurable revenue growth and retention, enabling customers to achieve the revenue to realize their vision.
Altera Digital Health

Booth 2532
Contact: Meghan Cavanaugh, events marketing manager
meghan.cavanagh@alterahealth.com
847.790.6876
A global healthcare IT leader, Altera Digital Health develops and elevates technology that brings next-level healthcare within reach. At HIMSS25, we’re excited to showcase how Altera is addressing the challenges healthcare providers are facing today by enabling system interoperability and data sharing, ensuring financial stability, and leveraging AI to help alleviate clinical and administrative burden.
Join us in booth 2532 as EVP of AI Ben Scharfe presents the Altera vision for the future of healthcare in “Shared goals and measured results: Why Altera is doubling down on client outcomes” on Tuesday, March 4 from 12:00-12:20 pm. Additionally, Ben will present how Altera is leveraging AI to tackle some of healthcare’s most pressing challenges in “Cool, but how will it actually work?: AI complexities in a practical healthcare landscape” on Wednesday, March 5 from 12:00-12:20 pm. We’ll also be thrilled to hear CareInMotion EVP Kevin Ritter present interoperability priorities at kiosk C3318-14 in the Interop + Smart Experience Pavilion on Tuesday, March 4 from 10:30-10:50 am during his session titled, “Make your data work harder: How actionable insights enable better outcomes for your organization.”
Additionally, we’re hosting our “Viva Altera” happy hour on Tuesday, March 4 from 4:30-5:30 pm, so stop by our booth, 2532, for a beverage and to meet with our experts. For our full theater schedule and to learn more about our presence at the event, visit alterahealth.com/events.
Arcadia

Booth 3510
Contact: Drew Schaar, communications and content
drew.schaar@arcadia.io
Visit Arcadia at booth 3510 to learn how you can drive savings, improve outcomes, and identify opportunities to grow your network with one streamlined analytics platform.
Attend our general session, “Proactive and reactive strategies to minimize data disruptions in healthcare,” on Wednesday, March 5 from 3:15-4:15 pm on Venetian Level 2 in Titian 2201. In this session, learn practical steps to prevent data errors, swiftly address disruptions, and build resilient data governance frameworks that boost patient care quality and organizational efficiency.
Attend our general session, “Enhancing high-risk maternity care with advanced data analytics,” on Thursday, March 6 from 9:15-9:45 am on Venetian Level 4 in Lando 4201. In this presentation, learn how one Medicaid ACO is using advanced analytics to revolutionize the identification and management of high-risk pregnancies.
Attend Byte-sized booth talks at various times in booth 3510. Learn in a series of short, informative talks with industry experts on timely subjects, from the latest CMS policies to emergent tech tools.
Attend “Sips and Socks” happy hour on Tuesday, March 4 and Wednesday, March 5 from 4:30-5:30 pm in booth 3510. Join Arcadia for happy hour to network with peers and snag a limited-edition pair of Arcadia socks.
Learn more and view a full schedule of Arcadia’s events at HIMSS25.
Artera

Booth 2766
Contact: Elyssa Jaffe, senior director, growth marketing
elyssa.jaffe@artera.io
904.536.7790
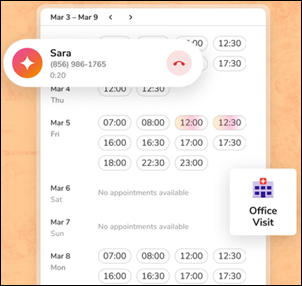
Artera is a SaaS digital health leader redefining patient communications. Founded in 2015 and headquartered in Santa Barbara, CA, the company is trusted by 800+ healthcare systems and federal agencies to facilitate more than 2 billion communications annually, reaching over 100 million patients. The Artera platform, powered by AI, integrates across a healthcare organization’s tech stack, EHRs, and third-party vendors to unify, simplify, and orchestrate digital communications into the patient’s preferred channel (text, email, and voice), in 109+ languages. The Artera impact – more efficient staff, more profitable organizations, and a more harmonious patient experience.
Our team will be available throughout HIMSS25 to share patient engagement best practices, offer product demonstrations, and answer your questions. Schedule and attend a meeting with an Artera team member and earn a $25 Amazon gift card. As an added bonus, you’ll be entered to win an iPad Pro in our post-event raffle. Schedule a meeting with our team here.
AvaSure

Booth 4672
Contact: Nicole Douglas, partner marketing manager
nicole.douglas@avasure.com
614.315.8112
AvaSure is an intelligent virtual care platform used in over 1,100 hospitals, enabling healthcare providers to engage with patients, optimize staffing, and seamlessly blend remote and in-person care at scale, addressing critical challenges in staffing shortages, rising patient complexity, and increased costs.
Join us at HIMSS in booth 4672:
Experience Innovation: Meet Vicky, the Virtual Care Assistant! AvaSure’s new patient engagement tool helps collect patient requests and uses AI to categorize, prioritize, and help the care team be everywhere they need to be.
Interactive Demos: See our latest advancements in virtual care technology, including a new dual device designed to outfit every hospital room with virtual care and AI-enabled workflows.
Expert Insights: Don’t miss us at a Brunch Briefing on Wednesday, March 5 from 10:30-11:45 am in Caesars Forum room 110 to hear from industry leaders about orchestrating virtual care success with CIO-CNO collaboration.
Visit AvaSure at HIMSS and discover how we’re innovating for the next era of care.
Cardamom

Contact Bridget Bell to schedule a meeting.
Contact: Bridget Bell, VP, business development
bridget@cardamom.health
608.658.3461
Cardamom is a minority-owned healthcare technology services company specializing in data, analytics, AI, and applications with a strong focus on EHRs — particularly Epic. With expertise in revenue cycle optimization, managed services, implementation, and flexible AI solutions, we help healthcare organizations maximize the value of their data and technology to reduce costs, enhance care quality, and improve patient engagement. Learn more at www.Cardamom.Health.
CereCore

Contact Phil Sobol to schedule a meeting.
Contact: Phil Sobol, chief commercial officer
phil.sobol@cerecore.net
615.344.4169
CereCore works behind the scenes to empower hospitals and health systems with IT services. Need to drive operational efficiency, improve financial outcomes, and uncover more bandwidth for your IT team? Our experts understand the major EHR platforms inside and out. Tap into support desk solutions that will result in happier users and providers. For the second year, we earned a top KLAS Research rating in managed IT services, and we were the only vendor whose clients responded “Yes” 100% of the time when asked if their managed IT services provider exceeded expectations.
Facing an EHR transition that requires additional expertise? CereCore partners with healthcare organizations across the US and globe to provide comprehensive EHR consulting, IT and application support, technical professional and managed services, strategic IT consulting, and advisory services. Our hospital operations experience means we can help you create customizable roadmaps for RCM optimization, overcome talent shortages, and maximize your HIT investment.
Get a healthcare IT assessment and benefit from an outsider’s perspective, because the cost of not knowing often far exceeds the investment in finding out. Connect with us at HIMSS and find meaningful change with CereCore’s healthcare IT managed services.
Clearsense

Meeting Pod 9319
Contact: Glenn Wirick, chief commercial officer
gwirick@clearsense.com
480.450.5424
Revitalize your Data with Clearsense
Experience how to revitalize your data with Clearsense at HIMSS 2025. Our Active Data Archival solution goes beyond storage — we transform your archived data into a valuable, accessible asset that enhances clinical and operational workflows. We help health systems reduce IT costs, accelerate M&A value realization, and improve clinician access to patient information — all with the industry’s fastest time to value.
Why Meet with Us?
Active Data in Action – See how our archival solution seamlessly integrates with daily workflows, eliminating the need for costly legacy systems.
Strategic Cost Reduction – Learn how top health systems are saving millions by consolidating outdated applications and streamlining IT infrastructure.
Industry Expertise – Meet with our data enablement experts to discuss your unique challenges and explore tailored solutions.
Let’s Talk Data.
Schedule a meeting with us at MP9319 and discover how Clearsense can help you maximize cost savings, boost efficiency, and unlock the full potential of your archived data.
Book your meeting now.
Clinical Architecture

Booth 1349
Contact: Jaime Lira, VP, marketing
jaime_lira@clinicalarchitecture.com
317.580.8400
Clinical Architecture is bringing back its in-booth Data Quality Theater for a second year! Visit us at booth 1349 during the show for 11 presentations from clients, industry thought leaders, and partners. Featured speakers include Stan Huff, Graphite Health; Jason Buckner, Manifest MedEx; Therasa Bell and Peter Schoch, MD Kno2; Michael Barr, MD Velox Health Metadata – and many others.
We will also be introducing the PIQXL Gateway, a tool that objectively scores the quality of patient data and pinpoints root causes of data quality problems so the information can be improved.
Be sure to join us for “PIQXL Gateway: The Key to Improving Patient Data Quality” on Tuesday, March 4 at 2:00 pm with presenter and Clinical Architecture CEO Charlie Harp.
View the full list and register for theater sessions here. Registration is encouraged but not required and the sessions are free to attend. We look forward to seeing you in Las Vegas!
CliniComp

Booth 5454 in the Venetian’s Executive Lounge, Level 3, Toscana 3610
Contact: Kem Graham, VP, growth and strategy
kem.graham@clinicomp.com
760.505.6879
CliniComp is an innovative technology pioneer serving customers globally for over 40 years with continual advancement in delivering a cutting-edge, comprehensive, EHR solution suite. CliniComp uniquely offers a System as a Service (SYaaS) model, eliminating the exorbitant cost of ownership with deployment of all system components in months, not years; with hardware, software, and 24/7 all-inclusive support, as a complete package of services for the life of the customer. The company was selected in 2024 as the winner of the “Best Electronic Health Record Service” in the MedTech Breakthrough Awards program, recognizing the breakthrough technology innovation of CliniComp’s unique and superior SYaaS model.
The CliniComp solution is an integrated, web-based EHR with an architectural framework conquering ever-evolving interoperability, scalability, adaptability, and real-time performance data challenges to provide a longitudinal patient record with Intrinsic AITM. Designed by clinicians for clinicians, CliniComp’s EHR delivers a comprehensive (inpatient, ambulatory, ancillaries, and revenue cycle) solution suite with an intuitive, seamless user interface and has earned an unrivaled record of performance and reliability with no planned downtime for decades in the most complex, high-acuity hospital environments.
For more information, please visit clinicomp.com and follow us on LinkedIn and X.
CloudWave

Booth 1373
Contact: Christine Mellyn, VP, marketing
cmellyn@gocloudwave.com
508.251.8899
Visit CloudWave, the healthcare data security experts, in booth 1373 for an interactive and informative experience! Our team of experts will be available to discuss important technology topics such as cybersecurity, cloud solutions, and more. In addition, we’re excited to offer a hands-on tabletop card game designed to immerse you in incident response and cybersecurity strategies. Using the Backdoors & Breaches deck of expertly designed cards, players will simulate real-world cyber incidents, sharpen response skills, and gain a deeper understanding of modern cyberattack techniques.
We’ve got a lot happening:
Win a Prize! – Participate in raffles at the conclusion of each day. You don’t need to be present to win!
Ask Questions, Get Answers – Visit our solution stations and speak with our experts about how CloudWave can help address your IT and cybersecurity challenges.
Meet with Our Team – Request a personal meeting (customersfirst@gocloudwave.com) with us to discuss your unique needs.
Tabletop Simulations – Join us for hands-on simulations and take home your own card deck plus a bonus gift if you complete the game.
Consensus Cloud Solutions

Booth 1361
Contact: Alyssa Beard, events director
alyssa.beard@consensus.com
319.325.2389
Despite significant advancements in healthcare technology, many providers and payers still face barriers to effective and secure data exchange. AI-powered technology offers a bridge between legacy systems and modern workflows, allowing organizations of all sizes to enhance data sharing without major financial or operational disruptions. At HIMSS25, Consensus will showcase its comprehensive product suite. Visit booth 1361 to learn how Consensus technology empowers healthcare organizations to overcome the challenges of unstructured data, achieve seamless interoperability, and boost operational efficiency.
Consensus will host several engaging customer and thought leadership panels in its booth, providing valuable insights and discussions that highlight the company’s commitment to innovation and collaboration. Attendees are also invited to Consensus’ booth for interactive demonstrations that show how its solutions work together to eliminate communication breakdowns, accelerate referrals, optimize administrative workflows, reduce provider burnout, and lower costs — all while contributing to improved patient outcomes and a more interoperable healthcare ecosystem:
- Tuesday, March 4 from 11:25-11:40 am: “Navigating the Rise to the C-Suite – Lessons for Women in Health Tech” with Propel Health Advisors co-founder and CIO Rebecca Woods and SoNE Healthcare CIO Renee Broadbent, MBA, CCSFP, CHC.
- Tuesday, March 4 from 12:15-12:30 pm: “Harnessing the Power of the Cloud to Support Growth Initiatives” with Piedmont Healthcare CIO Geoff Brown.
- Tuesday, March 4 from 2:15-2:30 pm: “Unlocking Efficiency: How AI is Enhancing Inbound Fax Workflows” with Consensus Cloud Solutions Account Director Nick Baxter and Consensus Cloud Solutions Solutions Consultant Marianne Soucy.
- Wednesday, March 5 from 11:15-11:30 am: “Leveraging AI to Accelerate Patient Intake” with Nick Baxter and Marianne Soucy.
- Wednesday, March 5 from 12:15-12:30 pm: “Elevate Fax Efficiency: Athenahealth and Consensus Partner to Integrate Cloud Fax with Your EHR” with Athenahealth Corporate Strategy Manager Mohana Nagda.
Cordea Consulting

Booth 4624 in partnership with AWS
Contact: Bill Smith, Epic practice director
bill.smith@cordeaconsulting.com
973.902.6990
Cordea Consulting provides expert IT advisory services, digital health and cloud leadership, and contemporary staffing support to hospitals and health systems globally. Healthcare IT is all we do. We use proven tools and methodologies to help organizations build and optimize EHR/ERP/EIS systems and evolve their technology portfolios. Organizations partner with us to unlock funding, accelerate innovation, and grow more competitive in their market.
Stop by the AWS booth, 4624, for some insightful demos and be sure to attend ”Unlocking EHR Excellence with AWS: The Jupiter Medical Center Story” Thursday, March 6 at noon in the HIMSS Theater. Cordea Consulting Epic Practice Director Bill Smith will share how a successful Epic direct AWS implementation delivered zero unplanned downtime and rapid patient care recovery — all while leveraging the scalability, security, and performance of Amazon EC2, S3, and RDS. Also learn how the implementation lowered operating expenses by 10%, resulted in 35% savings compared with other hosting options, and reduced Jupiter’s capital needs by nearly $4 million annually. This is a success story you won’t want to miss!
CTG

Booth 5544
Contact: Sarah Blafer, marketing business partner
sarah.blafer@ctg.com
860.942.2180
With over 35 years of expertise, CTG stands as a beacon in today’s healthcare IT consulting market. Our healthcare consulting solutions blend innovative services with cutting-edge technologies to address the unique challenges, requirements, and regulations of the healthcare market. Our comprehensive range of services includes EHR managed services (including activation, go-live, and training support), cybersecurity, ERP, cloud and infrastructure, application management, support and development, and IT support. Let’s connect at HIMSS (booth 5544) to explore how CTG’s healthcare experts can help transform your challenges into opportunities, ensuring your organization not only succeeds but thrives in a rapidly evolving landscape.
Ellkay

Booth 2825
Contact: Auna Emery, VP, marketing
auna.emery@ellkay.com
520.481.2862
Experience healthcare connectivity in action with Ellkay at HIMSS. At HIMSS25, Ellkay is bringing seamless interoperability to life. Visit our booth to see live demos of our cutting-edge data management solutions and discover how we empower hospitals, labs, payers, and healthcare IT vendors with effortless data exchange and connectivity. With integrations spanning 750+ EHR/PM systems and 1,100+ versions, we help organizations optimize workflows, fuel value-based care, and make smarter decisions.
Why Stop By?
Live Demos: See our powerful platforms in action.
Expert Insights: Learn why the industry is choosing Ellkay and chat with our team about your data challenges.
Fun and Treats: Network while enjoying our exclusive booth events.
Don’t Miss These Special Events
- Tuesday, March 4 Coffee and Tea from 10:00 am – 1:00pm
- Tuesday, March 4 Ellkay Theater session with CommonWell Health Alliance from 11:00-11:30 am
- Tuesday, March 4 Happy Hour from 3:30-5:30 pm
- Wednesday, March 5 Coffee and Tea from 9:45 am – 1:00 pm
- Wednesday, March 5 Ellkay Theater session with Meditech from 1:45-2:15 PM
- Wednesday, March 5 Ellkay Theater session with Canada Health Infoway from 2:15-2:45 pm
- Wednesday, March 5 Happy Hour from 3:30-5:20pm : Happy Hour
- Thursday, March 6 (9:30 AM – 1:00 PM): Coffee & Tea
- Thursday, March 6 Ellkay Theater session with Athenahealth from 10:30-11:00 am
Let’s talk about how Ellkay can power your healthcare data connectivity. Stop by and see interoperability in action. Learn more at Ellkay.com or connect with us on YouTube, LinkedIn, X/Twitter, or via TeamEllkay@Ellkay.com.
Elsevier

Booth 3616 and AI Pavilion Kiosk 121-14
Stop by booth 3616 at the HIMSS25 Global Conference to learn more about Elsevier’s latest product innovations that support clinicians in their work to provide the best possible patient care. This year, we’re looking forward to sharing exciting updates for ClinicalKey AI. Join us in our innovation theater at the booth to learn more about how AI tools like ClinicalKey AI can revolutionize clinical decision-making while you enjoy Birsta coffee sponsored by our sister company, Lexis Nexis Risk.
We will host two presentations at the AI Pavilion Theater. On Tuesday, March 4, Elsevier’s physician lead for evaluation, Amber Featherstone-Uwague, MD will present “Evaluation of Generative AI for Clinical Decision Support.” On Wednesday, March 5, Elsevier Physician Clinical Executive Paul Helmuth, MD will present “Industry Trends in Evidence-Based AI Adoption.”
Attending the AI in Healthcare Forum? Join us for an engaging fireside chat with Elsevier CTO Rhett Alden, PhD, Elsevier Physician Clinical Executive Paul Helmuth, MD, and Jennifer Bell, MA, PhD, director of bioethics research at the Department of Clinical and Organizational Ethics at UHN Clinical and Organizational Ethics, to discuss unpacking bias in healthcare AI.
FDB

Booth 2835
Contact: Matt O’Connor, regional sales manager
Matt.OConnor@fdbhealth.com
708.261.2996
FDB (First Databank) creates and integrates the world’s most trusted drug knowledge that, in partnership with our customers, illuminates critical healthcare decisions. HIMSS25 attendees will learn from FDB and its end users about how physicians, pharmacists, nursing, and clinical informatics leaders are improving patients’ health and safety and delivering high-quality care through FDB’s trusted drug knowledge and next-generation medication decision support, patient education, and e-prescribing network solutions that consider unique circumstances of individual patients.
Attendees will explore inspiring success stories from peers who have leveraged FDB solutions to redefine medication decision-making and transform clinician workflows. From increasing medication alert acceptance, improving Leapfrog CPOE test scores, integrating real-time pharmacogenomic (PGx) decision support, boosting medication adherence, easing operational burden for nurses and improving HCAHPS scores to enabling drug price transparency for consumers, answering consumers’ medication questions, and expediting development time – these success stories demonstrate meaningful impact.
And in the spirit of Las Vegas, attendees can test their luck, have fun, and unwind at the FDB booth. Visitors can spin the slot machine and discover the amazing benefits achieved by FDB customers in medication decision support. Each play earns a Barnes & Noble gift card, while hitting the jackpot earns even more special prizes!
HIMSS25 attendees are also invited to join FDB for a casual in-booth reception to network, enjoy complimentary wine, beer, and gourmet popcorn, and to share success stories. Details include: “Unwind with Wine, Beer, Gourmet Popcorn – & Success!” Wednesday, March 5 from 4:00–5:30 pm at booth 2835. Drawing at 5:15 pm to win one of two Amazon Kindle Paperwhite Signature Edition Readers! You must be present to win.
Read more about FDB Customer Success Stories.
Book a meeting with FDB.
FinThrive

Booth 5623
Contact: Heather Lane, VP, channel partnerships
heather.lane@finthrive.com
FinThrive is advancing the healthcare economy by addressing every transaction and patient interaction holistically through advanced, scalable solutions. Seamlessly integrating with EHRs, these solutions empower organizations to achieve growth, operational efficiency, and exceptional patient experiences. Backed by decades of expertise, our AI-driven RCM tools unlock efficiency, enhance satisfaction, and drive revenue growth. By eliminating the constraints of fragmented systems, we help healthcare providers realize their full revenue potential, ensuring reliability, compliance, and superior financial outcomes. With over $10 billion in net revenue delivered to more than 3,245 customers worldwide, FinThrive makes healthcare finance effortless.
Visit FinThrive at HIMSS25, booth 5623, to see us in person and be a part of the action!
Celebrate Our Best in KLAS Insurance Discovery Win: Join us on March 4 from 4:00-5:30 pm for champagne, cupcakes, and cookies.
RCMTAM Insights: Explore our industry-first Revenue Cycle Technology Adoption Model to assess and advance your revenue cycle.
Thought Leadership Podcasts: Watch live recording sessions with industry leaders hosted by Health Insights VP Jonathan Wiik.
Prizes and Pairings: Stop by anytime to spin the wheel for exciting giveaways and enjoy donuts and lattes on March 5 at 9:45 am.
Live Demos: Get hands-on with our innovative RCM tools and see how they streamline processes and optimize efficiency.
Discover how FinThrive’s next-generation technology can empower your organization. Visit our HIMSS25 event page to learn more about our exciting participation at the event and set up some time to meet with one of our subject matter experts onsite!
Get-to-Market Health

Contact Steve Shihadeh to schedule a meeting.
Contact: Steve Shihadeh, founder and CEO
steve@gettomarkethealth.net
610.613.4074
Optimizing healthcare technology sales: Whether a company needs to accelerate its top-line growth following an investment round or is bringing new products to market, Get-to-Market Health helps healthcare technology leaders market, sell, and create sustainable, long-term relationships with their customers.
Health Data Movers

Contact Brooke Foster to schedule a meeting.
Contact: Brooke Foster, marketing coordinator
brooke@healthdatamovers.com
847.404.0326
Join us on March 4 at 5:00 pm to network and unwind with Health Data Movers, Triyam, and the NYS HIMSS Chapter at Chica in the Venetian after the first full day of HIMSS. Enjoy drinks, tacos, and good conversation to wrap up your day. RSVP here. We look forward to seeing you there!
Health Data Movers (HDM) is a healthcare technology services firm. We are trusted partners to healthcare organizations, biotechnology companies, and digital health enterprises through our services – data management, integration, project management, and clinical and business applications. We are the smart choice for creating unique solutions that empower patients and providers by unleashing the potential of healthcare data and technology. We Make IT Happen! Visit www.healthdatamovers.com.
Healthcare IT Leaders

Booth 3017
Contact: Leslie Mitchell, events and brand manager
leslie.mitchell@healthcareitleaders.com
Healthcare IT Leaders @ HIMSS25 — Where Innovation Meets Impact
Join us at booth 3017 to learn how Healthcare IT Leaders partners with hospitals and health systems to drive innovation, streamline operations, and improve patient care. With deep expertise in enterprise consulting and workforce solutions, we can help you implement, optimize, and scale solutions from Epic, Oracle Health, Meditech, Workday, UKG, Oracle, Infor, Snowflake, and more.
Why Visit Booth 3017?
Learn more about how our Managed Services team is delivering savings and higher customer satisfaction at health systems like yours.
Discover how our EHR Advisory experts can help with everything from system selection to integration, optimization, data migration, and the latest in AI.
Network with your HIMSS25 peers at our VIP Cocktail Hour on Tuesday, March 4 from 6:00-8:00 pm at Tao Asian Bistro in the Venetian Hotel.
Plus, we’re giving away a premium Triton poker chip set inspired by Las Vegas casino nights. Take a gamble and stop by!
Med Tech Solutions

Booth 6026
Contact: Shana Tachikawa, director of marketing
stachikawa@medtechsolutions.com
Elicit greater value from your EHR investment.Take the first step to ensure the success of your EHR and maximize its full potential. Leverage skilled, flexible, EHR-certified resources to cost-effectively fill IT expertise gaps with:
- EHR Service Desk
- EHR-Certified Staffing
- Go-Live Support
- M&A Systems Alignment
Wherever you are in your EHR journey, we can help. Discover why MTS-Stoltenberg’s Partial IT Outsourcing EHR support program has been named Best in KLAS three times. Schedule an executive meeting in booth 6026 today!
Medicomp Systems

Booth 454
Contact: James Aita, director, strategy and business development
info@medicomp.com
703.803.8080
A leading provider of evidence-based, clinical AI-powered solutions, Medicomp Systems makes clinical data usable for enhanced decision-making and better outcomes. Medicomp works with physicians to deliver trusted, diagnostically relevant, actionable information to the point of care. The Quippe Clinical Intelligence Engine works with EHRs and health tech, driving intelligent clinical workflows that support the way clinicians think and work.
At HIMSS25, Medicomp is excited to introduce new technologies available to healthcare organizations to make clinicians’ lives easier, and to extend AI with interactive multi-modal workflows. Specifically, Medicomp will be showing cutting-edge capabilities that convert dictation to trusted, structured, reportable data to drive billing, interoperability, and compliance. Medicomp will also showcase support for USCDI v3 and v4 along with SDOH compliance tools. Finally, Medicomp is introducing new AI-powered tools for all healthcare organizations to clean up legacy structured and unstructured data for RCM, interoperability, risk-aversion, and reporting purposes.
For more, visit medicomp.com.
Meditech

Booth 972 and Booth C3318-02 at the HIMSS25 Interop + Smart Experience Pavilion
Contact: Rachel Wilkes, director of marketing
rwilkes@meditech.com
781.774.4555
At HIMSS25, discover how Meditech’s intelligent Expanse platform empowers a growing number of global healthcare organizations to achieve their goals with innovative, interoperable, and fiscally responsible technologies. Through first-hand clinician encounters and product demonstrations, attendees will discover how Expanse leverages AI and intelligent interoperability to improve the patient experience, reduce clinician burnout, and provide meaningful and actionable insights.
Visit our booth, 972, to see the following customer panel sessions, which include a free luncheon:
● “Patient-Driven Healthcare: How EHR Technology is Fueling the Precision Medicine Revolution” March 4 at 11:30 am.
● “From Data to Decisions: Advancing Healthcare with Smart Analytics and Intelligent Interoperability” March 4 at 12:15 pm.
● “Beyond the Bedside: Intelligent Tools for Today’s Nurses” March 5 at 11:30 am.
● “Transforming the Provider Experience: Smart Tools for Smarter Healthcare Delivery” March 5 at 12:15 pm.
Meditech will also showcase its latest interoperability projects and initiatives at the Interop + Smart Experience Pavilion — including the Traverse Exchange interoperability network, innovations enabled via smart app launches and FHIR APIs, and the resultant presentation of data to support advanced analytics and AI for workflow improvements. Joined by partners Google Cloud, Microsoft, Commure, DrFirst, Health Gorilla, and Suki, Meditech will demonstrate how embedded partner technologies supporting AI, ambient listening, and patient engagement help enhance clinician workflow and decision-making. Meditech will also headline two panels at the Interop Smart Theater alongside our customers and technology partners Microsoft (March 4 at 1:00 pm.) and Google Cloud (March 5 at 11:15 am).
Meditech’s HIMSS25 page provides more information on booth speakers, Smart Theater sessions, pavilion demonstration times, and customers presenting at HIMSS.
Nordic

Booth 5232
Contact: Gwen Cantarera, senior director, global marketing
gwen.cantarera@nordicglobal.com
484.678.0264
Join Nordic, a global leader in healthcare transformation, at HIMSS25 in booth 5232 to explore the future of healthcare technology, meet Craig Joseph, MD, author of “Designing for Health: The Human-Centered Approach,” enjoy our free coffee bar, and get exclusive insights on groundbreaking healthcare trends from the Nordic team.
Highlights:
-
Tuesday, March 4 at 12:45 pm: “Improving Appointment Capacity: Streamlining Scheduling with Physician Engagement and Technology” with Nordic Managing Director of Clinical Transformation Mary Sirois.
-
Tuesday, March 4 at 3:15 pm: “The Burnout Crisis Among Healthcare Clinicians: Contributors and Solutions” with Nordic CMO Craig Joseph, MD
-
Wednesday, March 5 at 10 am: “Strengthening resiliency against healthcare ransomware attacks” with Nordic Managing Director of IT Strategy and Cybersecurity Jason Griffin.
-
Wednesday, March 5 from 3:30-5:30pm: HIMSS Chapter Social featuring networking and drinks hosted by the Wisconsin, Greater Kansas City, and Virginia Chapters.
Optimum Healthcare IT

Contact Larry Kaiser to schedule a meeting.
Contact: Larry Kaiser, CMO
lkaiser@optimumhit.com
516.978.5487
Optimum Healthcare IT is a Best in KLAS healthcare IT digital transformation and consulting firm based in Jacksonville Beach, FL. Optimum’s comprehensive service offerings include enterprise application services, digital transformation, and workforce management, which features our skill development program, Optimum CareerPath. Backed by a leadership team with extensive expertise, we deliver tailored healthcare consulting solutions to diverse organizations.
Praia Health

Contact Jared Johnson to schedule a meeting.
Contact: Jared Johnson, CMO
jared.johnson@praiahealth.com
972.561.0025
Praia Health is the first consumer experience orchestration platform for healthcare, revolutionizing the way health systems engage and retain patients. Praia provides a digital flywheel, connecting all of the ways that a consumer interacts with a health system before, during, and after care visits based on actual data across an entire ecosystem — not just on segments, models, or clinical records. This allows health systems to provide consumers with truly personalized recommendations that reduce friction, increase engagement, and drive system loyalty.
Prominence Advisors

Contact Austin Montgomery to schedule a meeting.
Contact: Austin Montgomery, VP of partnerships
austin@prominenceadvisors.com
847.282.0109
Founded in 2011 by former Epic leaders, Prominence empowers healthcare organizations to execute strategic data initiatives with confidence. We’ve led the way in automating data pipelines and facilitating cloud migrations, delivering governed data products that enable self-service analytics, real-time insights, AI, machine learning, de-identification, and visualization. By seamlessly embedding analytics into workflows, we transform data into frictionless insights that drive action.
Recognized as the 2023 Best in KLAS for Technical Services and the 2024 Best in KLAS for HIT Staffing, our team brings unmatched expertise in maximizing your existing investments and upskilling your workforce. Our strong partnerships with leading cloud, lakehouse, analytics, AI, visualization, and governance vendors make Prominence the only firm capable of supporting every step of your data journey. Let’s unlock the full potential of your data and make healthcare smarter — together.
Prominence is teaming up with our customers and technology partners to showcase our data enablement solutions at HIMSS. Please see below for details:
“Accelerating Clinical Research with Large Language Models with Databricks” Wednesday, March 5 from 11:00-11:30 am in booth 4360. Discover how our partnership with UC Davis Health enhances clinical research productivity using Databricks’ LLM tools.
“Enhancing Healthcare Quality Insights with Snowflake” Tuesday, March 4 at 4:00 pm in booth 1670. Learn how Mass General Brigham optimized their Quality Dashboard performance and availability by migrating to Snowflake.
Rhapsody

Booth 3854
Contact: Purvi Thakur, director, growth marketing
purvi.thakur@rhapsody.health
214.727.8981
Rhapsody health solutions enable digital health innovation through interoperability for 1,700 healthcare teams around the world. The Rhapsody Digital Health Enablement Platform includes healthcare API and HL7 integration solutions, identity data management, and clinical terminology mapping and management. With Rhapsody, care providers, health tech builders, and public health teams speed time to market, improve the credibility of data, and keep engineering focused on what matters most. These API-first solutions are composable and flexible to meet you where you are; deployable in our cloud, yours, or as an iPaaS.
Visit the Rhapsody booth, 3854, for demos of these Best in KLAS integration solutions and EMPI with AI. Discover effortless EHR integration and seamless data exchange for better health.
Sonifi Health

Booth 5528
Contact: Michelle Allen, GM
mallen@sonifihealth.com
841.527.9093
Sonifi Health provides industry-leading, interactive patient engagement technology proven to improve patient outcomes and staff productivity. The EHR-integrated platform is designed to anticipate the needs of patients and clinicians, infusing the principles of hospitality into care experiences. Sonifi Health technology includes interactive TVs, digital whiteboards, digital patient door signs, and more. As part of Sonifi Solutions, Inc., the company supports more than 300 million end user experiences annually.
To learn more about the hospitality effect in healthcare and what Sonifi Health provides, stop by booth 5528 or schedule an appointment here. Join us for a happy hour at our booth Tuesday, March 4 from 4:00-5:30 pm.
Surescripts

Booth 1338
Contact: Kate Giaquinto, PR manager
kate.giaquinto@surescripts.com
603.548.5273
Surescripts, the nation’s leading health information network, will convene industry experts and Surescripts Network Alliance participants at HIMSS25 to highlight how innovative collaboration is advancing interoperability; automating prior authorizations; and enabling better informed, safer, and less costly care for patients.
Visit Surescripts at booth 1338 anytime and join us for a session (details below) to hear impactful conversations with Surescripts and healthcare leaders including:
Surescripts VP and CMIO Andrew Mellin, MD will be joined by CMIOs to share insights on technology-enabled value-based care. He will also lead a conversation with key collaborators committed to innovation that delivers a more automated prior authorization process, helping patients get the care they need sooner.
Surescripts Interoperability Affairs Manager Justin McMartin will engage with leading healthcare organizations to illustrate why advancing interoperability and joining a QHIN is key to ensuring clinicians can provide better informed, safer, and less costly care for patients.
Surescripts VP and CISO Judy Hatchett will discuss how partnering with Clear to add another layer of identity validation protections is a critical step to reinforce and further prevent fraudulent prescribing.
Symplr

Booth 4348
Contact: Ann Joyal, VP, marketing communications
ajoyal@symplr.com
866.373.9725
We will demonstrate two new innovations at HIMSS and offer additional demos, in-booth experts, and swag like tech tacos, Bluetooth trackers, and more.
Stop by to learn more about:
The launch of a new Symplr AI solution for Evidence Analysis, one of several AI-powered solutions introduced in 2025 that we’re working on with AWS.
Our new Symplr Operations Platform, offering a single integrated platform for healthcare that consolidates fragmented systems and standardizes healthcare non-clinical and administrative operations into a scalable, secure approach. Explore how this helps not only CIOs but also leaders across other areas including workforce, credentialing, supply chain, and contract management using healthcare-specific workflows and 30 years of healthcare industry know-how in partnership with customers.
Tegria

AI Pavilion (Venetian Level 2, 121-15) and Patient Engagement 365 (Caesar’s Forum, C3718-07)
Contact: Kristin O’Neill, senior director, external relations
kristin.oneill@tegria.com
617.319.5516
Tegria is a global healthcare consulting and services company created by healthcare for healthcare. We deliver customized, end-to-end solutions that deliver outcomes and drive transformation. We proudly partner with provider and payer organizations to advance care, improve performance, and address healthcare’s biggest challenges.
Be sure to mark your calendar for the following case study presentations:
“Enhancing Access and Experience: Bridging Insights and Innovations in Healthcare” Tuesday, March 4 from 12:10–12:30 pm in the HIMSS Patient Engagement Pavilion (C3718, Caesars Forum). Explore key findings from The Health Management Academy on patient access and experience. Learn how technology is shaping the future of patient-centered and provider-centered care.
“Building the Foundation for AI: SLUHN’s Journey to a Modern Data Platform” Wednesday, March 5 from 10:00–10:20 am in the Artificial Intelligence Specialty Pavilion Theatre. Discover how St. Luke’s University Health Network and Tegria built a cloud-based Azure data lakehouse to enable AI-driven healthcare advancements, streamline data management, and reduce costs.
“Lunch & Learn: Navigating the Healthcare AI Wave: Strategies for Evaluation, Decision-Making, and Implementation” (Lunch will be provided.) Wednesday, March 5 from 12:30–1:45 pm at Caesars Forum, Room 125. Learn how to evaluate AI opportunities; decide between build, buy, or hybrid models; and how to navigate IT and operational challenges. Gain practical insights through real-world use cases and interactive discussion.
TruBridge

Meeting Pod 10211
Contact: Ashley Stevens, VP, sales
ashley.stevens@trubridge.com
740.816.6717
TruBridge connects healthcare providers, patients, and communities using innovative solutions to address both financial and clinical needs, resulting in substantial value in healthcare delivery. Our revenue cycle services and technology, recognized by HFMA Peer Reviewed, stands at the forefront of the industry, enhancing productivity and fortifying the financial well-being of organizations. We advocate for data-driven patient journeys, bolstering value-based care and yielding improvements in outcomes and patient satisfaction. Furthermore, our EHR products play a pivotal role in supporting streamlined and efficient patient care by integrating data across various facility types.
Trust Commerce, a Sphere Company

Booth 2648
Contact: Ryne Natzke, chief revenue officer
rynen@spherecommerce.com
Visit TrustCommerce, a Sphere Company, at booth 2648. For over 25 years, TrustCommerce comprehensive patient payment solutions have earned the trust of the country’s largest healthcare organizations. Here are four reasons to make a visit:
- See how you can transform the way you process payments using TrustCommerce integrated solutions. Experience secure and compliant payment processing, anytime and anywhere – all while being seamlessly connected to leading EHRs like Epic, Veradigm, and athenaIDX.
- Come see a demo of Cloud Payments! TrustCommerce Cloud Payments offers healthcare providers and technology vendors an easily implementable, card-holder present payment solution giving patients and staff a more retail-like payment experience, while providing greater flexibility. The vP2PE, EMV, and NFC capable card-present solution is supported in TC Vault and is integrated with Epic, Veradigm, and others. No client-side desktop install is required.
- See our patient-friendly digital payment experience that proudly supports digital wallets such as Google Pay, Apple Pay, and PayPal.
- Learn about partnership opportunities. Ask us how to integrate TrustCommerce payment solutions with your digital health software to drive revenue, reduce risk, and increase workflow efficiencies.
Stop by for a latte, enter for a chance to win an Apple iPad, catch a demo, and join the fun at booth 2648.
Visage Imaging

Booth 661
Contact: Brad Levin, GM, North America
blevin@visageimaging.com
540.454.9670
Visage Imaging is a global provider of enterprise imaging solutions that enable PACS replacement with local, regional, and national scale. Visage 7 | CloudPACS is proven, providing a fast, clinically rich, and highly scalable growth platform deliverable entirely from the cloud. Today, 70% of Visage customers are in the cloud. Visage has not implemented a new customer on-prem in nearly five years.
At HIMSS25, Visage will demonstrate Visage 7 | CloudPACS, the new Visage Chat, and the groundbreaking Visage Ease VP for the Apple Vision Pro. Receive a demo of Visage 7 and receive a special-edition Visage SuperCar, along with a cup of gourmet Speedy’s Blend Coffee. See you in Las Vegas!
Waystar

Booth 4643
Contact: Angela Martin-Barcelona, senior manager, performance marketing
angela.martinbarcelona@waystar.com
844.593.8330
Waystar’s mission-critical software is purpose-built to simplify healthcare payments. With an enterprise-grade platform that processes over 4 billion healthcare payment transactions annually, Waystar strives to transform healthcare payments so providers can focus on what matters most – their patients and communities. Discover the way forward at waystar.com.
As healthcare continues to evolve, your challenges do, too. Stop by booth 4643 for some premium giveaways or schedule a time to talk with us about how we can help you boost productivity, deliver better patient financial care, and bring in fuller, faster payments.
Also join us on Tuesday, March 4 from 10:15-11:15 am to hear experts from Cleveland Clinic and Waystar discuss how healthcare leaders are harnessing the powerful potential of AI to revolutionize the revenue cycle to automate manual processes, combat denials, and accelerate payments.
Comments Off on HIStalk’s Guide to HIMSS25



























































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en