Stuart McLean, MBA is CEO of Nordic Global.

Tell me about yourself and the company.
I’ve been in healthcare for about three decades now. I started by doing merger work for what is now Northwell. I did that for half a dozen years as we built that system, which led me to have a deep appreciation for the importance of scale and operating efficiency. I co-founded my own turnaround firm and merged it into Alvarez and Marsal. I’ve been focused for the last couple of decades on strategic financial operational strength for healthcare providers.
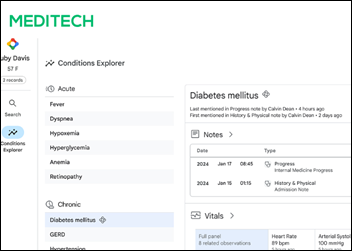
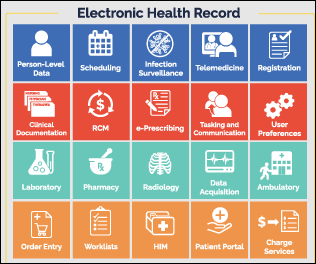
Nordic has been in place for about 15 years. We’ve greatly evolved over that time. We have a handful of areas of strength, certainly EHR – Epic, Oracle, and Meditech. We are increasingly working as implementation partners for Workday and Infor and seeing that as an important part of what our client healthcare systems need.
We’ve also developed a real strength in cloud, working with our partners AWS and Azure. The healthcare industry is moving to the cloud, at least on a hybrid basis, so it’s an important question about how best to do that. Finally, I would want to highlight the transformation that we have taken on to move in the direction of a full-service, end-to-end managed information technology company for our clients.
How do you characterize the health tech consulting market and how do you differentiate Nordic within it?
I think it’s getting increasingly crowded. Private equity views this as an important part of the healthcare transformation, so there’s a bit of a rush into this business.
We have maturity and a deep team. We have 3,300 professionals who have been at this for a while. We began 15 years ago with a deep expertise in the implementation, optimization, and integration of EHR systems. We think that makes a significant difference.
What are the benefits and drawbacks of being such a large organization that also provides services in Europe?
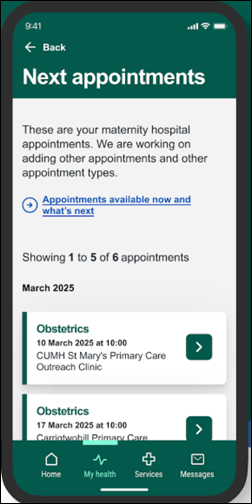
The expansion into Europe has been interesting. We operate in four countries in Europe — England, Ireland, Switzerland, and the Netherlands. We are growing pretty rapidly in that market as those markets recognize the benefits of the EHR platform as part of their strength. Because of our focus on managed services, we do a good bit of outsourcing work both in Ireland and in the Philippines.
How far along is the move to the cloud? Are health system worried about the cost or vendor lock-in?
This is a very early game. We just published an e-book that is available on our website where we dive into that a little bit deeper. We think it’s important to have a comprehensive evaluation so that we understand the benefits from an integration perspective and the concerns with regard to security since health systems are, and should be, risk-averse with regard to patient care information. That’s an important element of the response that health systems must make to the financial pressures that they are feeling.
Oracle Health has a lot of resources when it comes to cloud and technology and general. How will that influence its position in healthcare?
We are all going to benefit from that competitive dynamic between Epic and Oracle Health. Each company comes from a slightly different place. Both companies see the massive market size here and are pursuing it. They are pursuing it thoughtfully. I don’t pretend to have a clear crystal ball into who will be the winner here. They both will survive. They both will thrive. Here again, the health systems will benefit from that kind of competitive dynamic.
How much do health systems margins, M&A, and changes in staffing patterns affect your business?
As somebody who knows the health system industry really well, I’m surprised at the government’s response to the desire and the need for scale with health systems. I’m really surprised by it. When you compare UnitedHealthcare or any number of these large, national, fully consolidated insurers and the desire by the US government to keep healthcare pretty fragmented, it makes the work that Nordic does even more important. Those health systems are simply unable to access the scale economies that they would if they were allowed to be $20 to $50 billion super-regional health systems. We at Nordic can deliver the benefit of that scale.
How are health system IT departments affected by cloud adoption and the challenge to find and keep employees with specific skills?
It’s a little overwhelming. Without naming or getting into any competitive information, we have clients who are very concerned about the competition for their IT talent. That’s where I think we can be beneficial, because of the size that that we have, for those clients that choose to establish an outsourced relationship with us.
Two things happen. One, they no longer have to worry about access to talent, because we have it on a national and international basis. Secondly, we think we’ve struck the right mix of offshore, lower-cost delivery and onshore capacities.
Will the shift from onsite consulting to remote services last?
I think so. I’m an individual on this question, but also we at the leadership level have given some thought to this. We see efficiencies from non location-specific delivery of these services.
Will AI change your business?
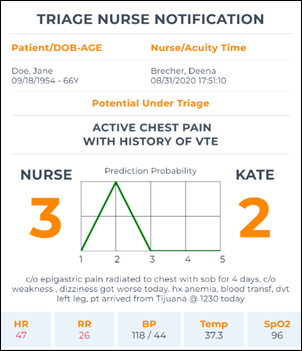
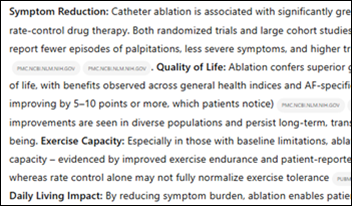
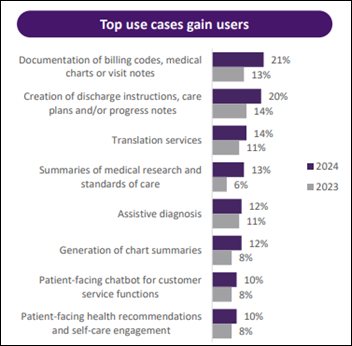
For AI adoption to be successful, it’s a balance. It’s technology, but also humanity and empathy. The focus in the health systems space today is principally around decision support, predictive analytics, and workflow optimization.
We don’t see a revolutionary impact in the near term, in the next year or two. To your earlier question, with regard to Epic and Oracle, those organizations are spending a tremendous amount of energy and effort in this area and are working with early adopters to beta test and refine these capabilities.
I think the AI promise is very real, but it’s more likely three to five years away than one to two years.
Will it deliver tangible ROI to health systems in the short to medium term?
I don’t see it in the short term. I’m not even sure that this will ever be an ROI topic for health systems. It’s about the quality of care and population health, with the ability to become more proactive, more targeted, and more precise with regard to patient- specific situations.
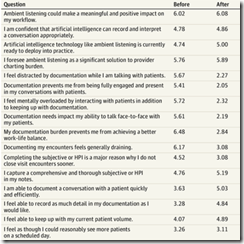
How much of an AI driver is clinician satisfaction and wellness?
It’s not a primary ask from our clients at this point. It’s a bit more of an evolutionary component of this. The clinician and physician wellness part of it will be supported by the healthcare heuristics element. Have you asked this question? Have we considered this diagnosis? Rather than the AI providing the answer, it will offer help with going down the decision tree in the pursuit of the answer.
Shifting to business climate, what kind of companies will be winners and losers now that cheap financing is gone and investor demands have changed?
I think there will be a fair bit of chaos in this space. Nordic is in a very strong position. W are owned by Bon Secours Mercy Health, and their ownership interest is strategic and long-term. We’re not worried about capital structure and those sorts of things. We are focused on the strategic value of the work that is delivered by Nordic to our clients. We have a longer and more patient horizon, and that will make us stronger over time. There is money pursuing quick earnings, and this business requires patience.
Does General Catalyst’s acquisition of Summa Health foretell significant industry change?
I don’t follow General Catalyst closely, but I’m aware of that situation. I think they see the health system ownership as platform, almost a laboratory, for innovation that could then be deployed and delivered to others. I think that Bon Secours Mercy Health is in a better, stronger position as an independent, not-for-profit. long-term that’s less interested in capitalizing and creating dollars than they are in supporting the quality of care over long periods of time.
What factors will be important to Nordic in the next three to five years?
Strategic partnerships with other large health systems. We’ve been a contractor and we remain a contractor, largely. We’re hired by a health system to run a project to implement the EHR or optimize the EHR. We see our benefit increasingly in long-term, five-plus year agreements with health systems to be their technology partner. Not developing technology, which is the role of Epic and Oracle and others, but managing that technology cost-efficiently because the pressure is real. We think that we can be worth 25 to 30% over time in terms of the technology spend while still ensuring a strong, durable, consistently available platform.












































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…