Top News

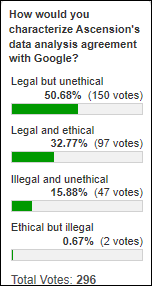
The HHS Office for Civil Rights will look into the HIPAA compliance of Google’s data-sharing arrangement with Ascension.
Google has pledged to cooperate with OCR investigators, stressing that its work with Ascension adheres to HIPAA and “comes with strict guidance on data privacy, security, and usage.”
The company added in an amended damage-control blog post that, “Patient data … is not used for any other purpose than servicing the product on behalf of Ascension. Specifically, any Ascension data under this agreement will not be used to sell ads.”
Google Cloud now knows that its parent company has a consumer image problem that, while not on the magnitude of Facebook’s, could still serve as a roadblock for its technical work that has nothing to do with search engine ads.
Perhaps most puzzling is why Google hasn’t enlisted its new high-profile healthcare hires to explain the project or to describe why it’s likely that patient data is more secure within Google’s systems than in those of any hospital or medical practice.
The odds that this deal violates HIPAA are zero. It only violates the data rights that consumers wish they had.
Reader Comments
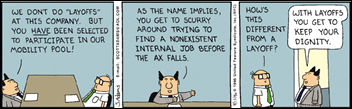
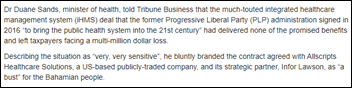
From RumorMonger: “Re: Allscripts. Reducing workforce today to cut costs, with a rumored 25-50 people let go.” Unverified, but reported to me by several readers, some of whom said weeks ago that the cutback was scheduled for November 18. Rumored areas impacted are Sunrise, support, and development.
From PizzaSlinger: “Re: Cerner layoffs. A manager apparently sent the layoff script to the associates he was laying off.” I hate that layoffs have become corporate business as usual, with companies unskillfully using them to (a) dump deadwood and high earners while dodging employment law issues; or (b) to quickly juice their financial numbers to arouse some bean counter. I get really worked up when the company cluelessly acknowledges the announcement with a cheery statement that while the valued (to a point) former associates will be missed, the company is hiring wildly otherwise. Maybe the “overall headcount increase” promise encourages investors and customers, but it throws salt in the layoff wound by clearly indicating that the affected “associates” aren’t worth retraining or reassigning. Still, I commend Cerner for sending its executioners a script – which was forwarded to me — to make the employee’s final contact with the company smooth. My summary of it:
- Schedule the appointment ahead of time using an attached link (I assume using the link automatically alerts campus security to be close by at the designated time since that wasn’t emphasized nearly enough in the script otherwise).
- “Anticipate their reaction so you can prepare.” Having laid people off myself, I don’t think you can do this with any degree of accuracy. Most employees are initially stunned, so the idea is to get them off campus without a working access badge before their Kubler-Ross’s “denial” turns to “anger.” I’m surprised that the instructions advised making the appointment ahead of time since that’s a sure sign of impending trouble, although it’s also awkward to have a layoff when some of those affected are on PTO and thus likely to hear from co-workers or a telephoning manager that they are now unemployed. It’s also a good idea to tell the survivors not to let their former co-workers into the building.
- Coordinate with the co-worker who gets the fun job of marching the employee to the “offboarding support area” and then packing up their pitiful personal effects while they are getting the axe.
- Don’t tell people their job has been eliminated while they are at a client site or driving.
- Keep the conversation short, no more than 20 minutes, but book the room for 30-60 minutes so they can compose themselves without being kicked out of the room to make way for the next execution.
- Have Kleenex on hand.
- Tell them not to return to the office, but advise them that they will remain an active employee through January 14, 2020.
HIStalk Announcements and Requests
The best lesson we can learn from the Ascension-Google controversy is that Americans are naive in thinking that HIPAA gives them broad privacy protection, so perhaps the shock – justified or not – that a company that most Americans know only for searching and serving ads is holding their medical data will open much-needed consumer privacy law discussion. Many people, even media types, seem shocked that HIPAA addresses only providers, or that they get a free pass under “treatment, payment, and operations.” I don’t question the data-sharing deal since it’s really not all that unusual other than consumers react more quickly when it’s Facebook or Google than if they found out that many, many other companies are sifting through their medical information, sometimes paying some other organization for the privilege. Bottom line – Ascension did nothing intentionally wrong, patient data is almost certainly safe, and both Ascension and Google now know they have a public trust issue that isn’t limited to just this tiny aspect of their businesses. I’m waiting to see if Ascension’s interest really is related to clinical outcomes rather than their own financial ones and whether anyone raises the issue of whether Ascension really has 50 million signed Notice of Privacy Practices forms on file (and whether those are valid if they were signed before Ascension acquired the original hospital). All this aside, the issue goes well beyond these two organizations.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

NextGen will acquire patient intake, scheduling, and payment software company Medfusion for $43 million. Medfusion will spin off its data services business into a separate entity named Greenlight Health. Steven Malik sold Medfusion in 2010 to Intuit for $91 million, then reacquired it in 2013. He owns the North Carolina FC of United Soccer League and North Carolina Courage of National Women’s Soccer League and is working to build a $2 billion entertainment complex in Raleigh.
The planned merger of Sanford Health (SD) and UnityPoint Health (IA) to form one of the country’s largest health systems is called off, with Sanford’s CEO saying that UnityPoint Health’s executives “failed to embrace the vision.”
Sales
- St. Joseph’s/Candler will implement Tabula Rasa Healthcare’s DoseMeRx precision dosing software across its facilities in Savannah, GA.
- Willis-Knighton Health System (LA) selects Meditech Expanse.
- Humana, GuideWell, and Trusted Health Plan will use Healow Insights integrated services from EClinicalWorks for interoperability among their networks.
People

Surgical software vendor Provation Medical hires Daniel Hamburger, MBA, MS (Renaissance Learning) as CEO. He replaces Dave Del Toro, who will join the company’s executive board.

Jamie Trigg (Seattle Children’s) joins Virginia Mason Health System (WA) as CTO.
Announcements and Implementations

The St. Louis Children’s Hospital and Washington University Heart Center (MO) sends high-risk infant cardiac patients home with Locus Health’s remote monitoring app.

Best Buy ups its digital health offerings with the addition of TytoCare’s at-home medical exam device and companion app. The $300 device comes equipped with attachments that can be used during a telemedicine visit with partners from several health systems and telemedicine companies.

CHI Memorial Hospital (TN) implements Epic.

WellSky develops the WellSky IO interoperability framework to help post-acute and community providers connect to patient data exchanges.

The Michiana Health Information Network, Indiana Health Information Exchange, and HealthLinc will merge operations under the IHIE brand in January. IHIE executives believe the consolidation will create new value propositions and help scale services. IHIE has played around with several business models since launching in 2004, including its ThriveHDS clinical data repository services offshoot, which shut down after just nine months. The HIE’s CEO and COO presented “Said the HIE: ‘Reports of Our Death Are Greatly Exaggerated” at HIMSS earlier this year.
Amazon Web Services launches AWS Data Exchange, giving users the ability to find, subscribe to, and use third-party data in the cloud. Healthcare use cases include subscribing to aggregated data from historical clinical trials to accelerate research activities, and subscribing to aggregated and de-identified healthcare claims and transaction data to improve care delivery.

In Canada, Ontario health officials announce a Digital First for Health strategy that will aim to give patients the ability to book appointments online, access their medical records, and take advantage of more telemedicine services within the next three to four years. Providers will be given access to interoperable records, and enhanced data integration and predictive analytics.

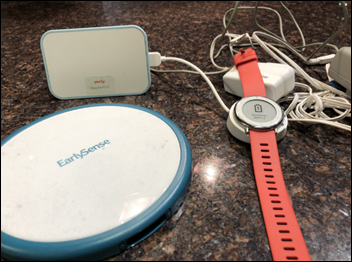
A KLAS report on remote patient monitoring finds that nearly all users get measurable outcomes, but the market is changing to demand products that are patient-centric, that engage patients, and that offer patient-provider interaction, all using consumer-based rather than proprietary medical devices. Health Recovery Solutions and Vivify Health are leading the evolution, but the report’s conclusions are incomplete because several vendors refused to participate (Resideo, Care Innovations, Medtronic, and Philips).

Patient safety groups ECRI Institute and the Institute for Safe Medication Practices will merge, with ISMP becoming an ECRI Institute subsidiary.
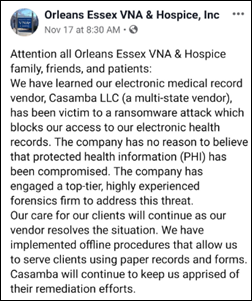
Privacy and Security
I can’t tell if this is satire or serious: Google’s alleged whistleblower takes to The Guardian to outline why he or she felt compelled to share concerns about “the Nightingale Project” with, presumably, the Wall Street Journal: “After a while I reached a point that I suspect is familiar to most whistleblowers, where what I was witnessing was too important for me to remain silent. Two simple questions kept hounding me: did patients know about the transfer of their data to the tech giant? Should they be informed and given a chance to opt in or out? In short, patients and the public have a right to know what’s happening to their personal health information at every step along the way. To quote one of my role models, Luke Skywalker: ‘May the force be with you.’”

Health Care Cost Institute CEO and former CMS Chief Data Officer Niall Brennan tries to calm the masses.
Other
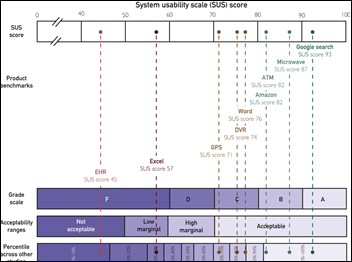
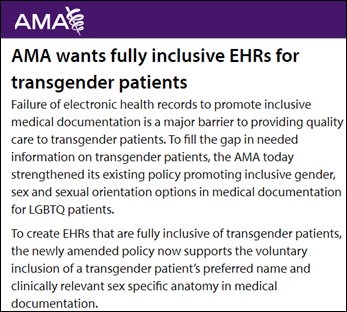
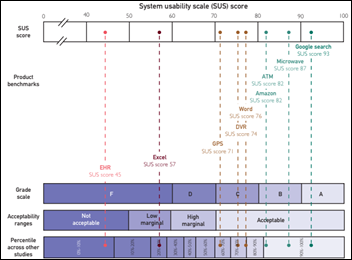
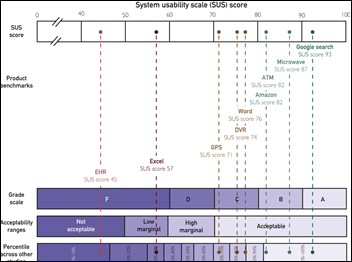
The American Medical Association co-sponsors a study that finds that perceived EHR usability is poor and contributes to physician burnout. The article is paywalled so I can see only the highlights (except for the graphic above, tweeted out by one of the authors), although I notice that response rates weren’t good. The authors conclude that EHRs scored an F with self-reported doctor scores in the bottom 9% across all industries and then correlated those scores to burnout. The correlation versus causation issue would lead me to question, do EHRs burn doctors out, or do burned-out doctors hate EHRs as a tangible manifestation of their unhappiness? Also, I’m not sure that it’s fair to compare an EHR to Amazon, a Google search, or a microwave oven, especially since those tools are voluntarily chosen for personal benefit. Doctors are frustrated with their EHR, but they’re also frustrated with nearly everything else about their jobs (and many of them must be frustrated with the AMA itself as well, given that only a fraction of US doctors are members, so maybe the EHR vendors should study that phenomenon).

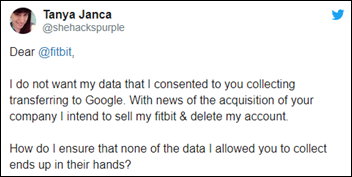
STAT looks at the integral role remote healthcare coaches play in the success of headline-grabbing digital health companies like Omada Health, Livongo, and Fitbit. Omada Health CEO Sean Duffy admits that though he’s a big fan of tech, “It’s hard to recreate human accountability.”

Results of the Apple Heart Study are in, leaving researchers with several solid takeaways regarding the Apple Watch’s ability to alert users to abnormalities. The eight month study of 400,000 users – one of the largest of its kind – found that the device notified two thousand of an irregular pulse; 84% of which were found to have atrial fibrillation. Researchers concluded that passive monitoring can be beneficial, but more work needs to be done for the Watch to be truly useful in helping at-risk, rather than young and healthy, populations. Apple just launched a separate Research app to study heart, movement and hearing issues, and women’s health.
Sponsor Updates
- Apixio celebrates several milestones including its 10th anniversary, adding 17 new provider and payer customers in 2019, and making Deloitte’s 2019 Technology Fast 500 list of fastest-growing companies in North America.
- Ellkay will exhibit at Momentum 2019 November 22-24 in Orlando.
- Ensocare will exhibit at the 2019 Leadership and Physician Advisor Conference November 15-17 in Miami.
- CarePort Health’s post-acute provider database and patient choice application, CarePort Guide, is now available in the Epic App Orchard marketplace.
- HealthCrowd will present at the Florida Association of Health Plans 2019 Connect Conference November 19 in Orlando.
- In Australia, Hyland integrates Medrefer’s referral technology with its OnBase enterprise information technology.
- InterSystems will exhibit at Healthcare Providers Transformation November 18-20 in Denver.
- Intelligent Medical Objects will exhibit at the AMIA 2019 Annual Symposium November 16-20 in Washington, DC.
- Kyruus CTO Chris Gervais will present at Salesforce’s DreamForce November 20 in San Francisco.
- AMIA inducts Clinical Architecture CIO Shaun Shakib into the 2020 Class of AMIA Fellows.
- Recondo Technology announces that bookings for its automation solution for prior authorization transactions has accelerated in 2019 to 60 health systems, most of them Epic users.
- ZDNet profiles Nuance.
- Health Catalyst appoints Julie Larson-Green (Qualtrics) and S. Dawn Smith (Cologix) to its Board of Directors.
- The Chartis Group publishes a new white paper, “Creating a Successful Physician Enterprise in Academic Health Systems.”
Blog Posts

Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.






















































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…