Consultants responded to three questions:
- What kind of consulting do you offer?
- How has the pandemic affected your work, job, or firm?
- How do you think your work will change once the pandemic is controlled?
Healthcare IT consulting
My company is seeing large reductions in revenue due to clients putting projects on-hold due to COVID-19. Luckily not all projects have stopped so the company is still generating revenue. My company has put a thoughtful, deliberate financial plan in place to preserve our company and jobs. The hope is that we’ll be able to ramp up quickly when COVID-19 is over or controlled. Our company has been transparent about the plan and is keeping us updated. All non-essential expenses have been cut; we are taking pay cuts temporarily (which will be paid back at a later time); we are required to take PTO; company has worked with our PE firm to secure additional cash. With all that, morale remains positive. Company is doing a good job of supporting working from home and staying connected to clients, increasing company connectivity through virtual fun events, etc.
From an IT perspective, we anticipate more M&A work since there may be more distressed hospitals looking for a savior; more telehealth / virtual visit strategy and plans; assistance with financial optimization.
Third party Cerner consultant
Working remote from home instead of on site Monday-Thursday. Project I am on is on hold until after Covid-19 settles down. There still are minor maintenance items, busy work, and weekly meetings. Really not much going on. My client has all its IS staff working from home as well.
Unsure. If this goes on for the 12-18 months to develop a vaccine, could be long time before I take another flight/on site on regular basis. Management already told us to not plan any travel until late June at the earliest. Client is in a hot spot that still has increasing cases. Contract is up in five months, so expect if nothing has changed most likely will not get renewed.
Epic analyst. I’m Boost (consultant through Epic)
It’s affected the work I’m doing day-to-day, but nothing beyond that. I had a steady gig with a long-time customer already (six years while I was at Epic in Madison, and three years in Boost with them since then). I already worked from home except for go-lives. If anything, the fact that other employees at my customer are now working from home has made my job better and easier. Normally, I don’t hear the water cooler talk or get pulled in to help with little things because they have someone sitting right next to them who can do it instead, and that’s just easier than messaging me on Teams or calling me. But now that no one is sitting right next to another analyst who can help, I get looped in on a lot more. It’s been nice! Also, as one of the quicker learners on our team, I’ve been the one to jump in on a lot of the new, highly integrated stuff we need to do for COVID. And normally I don’t do anything with our Infection Control module, but in the past week I’ve learned most of the workflows and data elements and am helping to take the load off our already-overworked, single infection control analyst. People like me who can be flexible, coordiinate across applications, and learn quickly are always in high demand. I’ve found that during a crisis like this, that’s even truer.
I hope my customer increases the opportunity to work from home so that some of the benefits I’ve seen will stick around. But I think that’s unlikely — they already offered work-from-home for 1-2 days a week depending on tenure. So overall, I don’t think it will change once life is back to normal (or whatever our “new normal” will be).
Sales and marketing consulting for vendors
Some of the smaller vendors we serve are struggling due to providers asking to defer payments, so in order to protect their teams from layoffs, they’ve reduced or cancelled our consulting contracts. Others have asked for reduced but continued work, but have asked us to defer our billing until their cash flow improves. We’re taking the opportunity to focus on value-add content we can provide to vendors. This comes in the form of sales tips, marketing tips, or training ideas for their teams. We’re also exploring other ideas for services we could offer that would allow for a reduced presence of vendor personnel in a hospital or health system.
We expect that work will pick back up eventually, but it may take some time to get back to the client volumes we’ve been accustomed to. A lot of the work we do is remote anyway and has always been on Zoom or other video conferencing platforms, so in that regard it’s been an easy transition. It’s more about revenues stabilizing for the vendors so that they have money to spend on consulting work again.
Helping practices build high-performing remote care management
Increased: initial urgent response to expanding any existing telemed across the enterprise and/or rapid adoption from scratch. Decreased: existing chronic care management and remote monitoring have been pushed to the back burner, which is understandable. But overall, remote care management as a delivery vehicle will be a paradigm shift driven by micro and macro factors.
We expect demand to increase. Thanks to COVID, the interest in remote care has been thrust into the spotlight and the toothpaste is not going back in the tube. We believe practices and enterprises will quickly expand from simple video visits to the full suite of on-going remote care & perpetual patient management. Reimbursements are already in place, MACRA / MIPS & transition to value is already in place and COVID has put a spot light on the weaknesses of traditional episodic care. Integrating remote care into healthcare delivery will be a dominate theme in the next few years of healthcare consulting. Consider these entire categories that have multiple reimbursements each: televisits, e-visits, virtual check-ins, remote chronic care management, remote physiologic monitoring, transitional care management, principal care management, behavioral health integration, collaborative care management and oncology care management.
Clinical EHR optimization
We have less business overall, and our active projects are getting delayed. Clinical leads who normally partner with us are understandably getting called to the front lines.
There is a lot of pent up demand and we are expecting a big bounce once things get back to normal. We may have to grow our team if too many delayed projects need to re-start all at the same time.
Epic OpTime
I’ve now seen more internal emails circulating referencing lower hours or rate reductions, delayed or deferred projects, and providing information on COBRA, bench time, and offboarding. So clearly developing between just last week and this week. The firm has been communicating frequently, weekly calls scheduled presently. It seems the extended timeline of COVID is leading to more affected engagements than I realized, and presently I’m one of the lucky ones (knock on wood). Relatedly, in connecting with some former clients staff, it seems they may be seeing layoffs disguised as furloughs taking place. Last time I saw something like this was at an employer during the financial crisis last decade. Using layoffs predicated on anticipating expected financial hardship to remove staff that no one previously could be bothered to do the paperwork to track performance issues and terminate (or maybe just didn’t like them). Salaries and hiring were frozen as well, so it was a bit awkward when instead of a loss they cleared a large profit. They ended up paying bonuses to staff to make up for the bypassed annual increases. Oddly enough the staff terminated into a recession with a high unemployment job market (and were frequently still unemployed months later) never were offered their positions back when they started hiring again relatively soon after.
I find rate reductions to be sticky personally, so I wonder how much more downward pressure this might create. Working at a state institution presently I can view the staff salaries for my FTE colleagues, and, combined with the benefits they receive, we are getting progressively closer to where the risk/reward of the consulting lifestyle is rather narrow. I continue to see consultants (talented ones) take FTE roles as the margin on consulting pay shrinks. I wonder who will be left willing to travel, have generally inferior benefits, and have greatly reduced job security for only an extra 20% (after reducing for the higher insurance premiums, HSA contributions to cover that high deductible plan, and at this client anyway an actual funded generous pension!).
Epic consulting
I’m getting no engagements. Health systems have suspended their EHR projects, suspended or cancelled consulting engagements, and flights aren’t available to get people on site.
I’m guessing that at some future point in time (maybe Oct/Nov) there will be a HUGE demand for skilled and experienced Epic resources. By laying off folks and terming projects in flight, Epic users have, whether they understand it or not, chosen to upset the state of their install. Post this current world, sites with Epic will need to (very quickly) make changes to ensure they are capturing all the revenue they can AND update clinical workflows and related. AND, I suspect, they will all be reviewing most of their foundational views on the industry as a whole and how to leverage technology effectively (telehealth as an example).
Epic sites have been slow to embrace the 100% remote engagements because their mid-level managers have no idea how to work in that environment. I suspect that will change very quickly. Firms all across the country have spent countless dollars on building state of the art buildings and campuses to house their workers, yet for the last x number of weeks, those same workers have been working from home and overall the work is getting done and the world has not stopped spinning.
Managed services –tier two support
My firm has lost several big clients in the past few weeks. Some have been long existing clients. So far nobody has been laid off and they are trying to make sure that does not happen. I have a certification that is not that common, so I am hopeful that will help keep me employed.
I don’t believe things will return to normal for many months after the pandemic is controlled. As internal IT staff shifts back to the normal day to day of enhancements, quarterly updates I think our services will be as much in demand as they had been.
Interim management
Consulting gig cancelled with no plan to re-engage for the next year
Organizations are looking at priorities and margins. Telehealth has greatly disrupted how care will now be delivered
Epic
We are seeing some delays of new projects, with most existing projects converting to remote.
I think more organizations will realize it’s silly to spend the money on weekly travel to get consultants onsite. Hopefully more will consider full or partial remote arrangements.
Imaging
$15K of work evaporated in early March “postponed” until midsummer, when the clients felt they would have a better grip on available budget money would be available. Now that I am seeing layoffs left right and sideways, I am not counting on anything coming through at any time. I have also had a few potential clients ask me for an outline of what I felt needed to be done for them and how I would do it and after I submitted it for review they used what I submitted as a template to have the work done internally instead. Nice
It will easily take a year for things to settle down if not longer. Contract prices are going to be negotiated like never before with the low bidder (not necessarily he best candidate) getting the job if anyone gets it.
Implementations, optimization, and go-live support
All implementations, projects and go-lives have been delayed. Most consultants have now been moved to answer phones for MyChart and Telehealth support working remote.
Assume implementations and go-lives will move forward, still requiring support from consultants.
Epic principal trainer consultant
My most recent contract wrapped up March 31, and I was planning to travel internationally for six weeks. When I realized early-March that international travel was not going to happen, I began scrambling to try to find a new contract. A couple of projects I was submitted for are on hold, one project is going to be interviewing in the next few weeks, but there have been absolutely no new leads from my recruiting network in over three weeks. I am certified in multiple modules, have 8+ years of Epic experience and 5+ years of consulting experience, so I am used to receiving many leads if I have upcoming availability.
I think that hospitals will realize that much of the onsite work that has been done in the past can be done remotely, so there will be more remote options available. I have seen the trend shift towards that in the past three years in general. I also think that it may be more difficult for hospitals to budget money for consultants to assist with upgrades and staff aug because they will be trying to make things right with the clinical staff that had to have wages cut and were laid off due to drop in rev from surgeries, etc.
Mostly IT implementation, management and business strategy on occasion
The work is not slowed down. Clients converted their project teams to full remote work, consultants included. After reassessing priorities, all my projects will continue with no more than minor schedules changes. For one project the end users in an administrative department were converted to remote and so we will provide a remote go-live.
I anticipate that clients will go back to expecting onsite consulting support, but be more open to remote support.
Imaging: Operations, Clinical and Technology Services
Our firm has adapted to largely virtual consulting, which has had a much smaller impact to the substance of interaction as well as the quality of outcome (early feedback). In addition, the lack of need for travel buffers has RADICALLY improved our team’s focus and amount of actual work completed on a daily/weekly basis. While several clients have postponed and/or reduced scope of projects, much of the ongoing work is continuing. We believe this is due to the fact that most organizations realize that the current reduction in elective procedures will become a tsunami of work once we slowly “reopen” our businesses. Many in the ambulatory setting see this time as an opportunity to achieve important, but not previously urgent, initiatives.
I believe business as usual will be different for a very long time. Social distancing will be the norm going forward until we have all types of testing in place and ultimately a vaccine. In addition, the shift in engagement is changing people’s minds about what value face-to-face actual brings in working together and collaborating.
EHR implementations
We have switched to remote-only work. A number of clients have suspended or postponed ongoing projects, as well as a few cancellations. Furloughs have begun.
I feel that there will be some resumption of projects in the three to four months following control of COVID, but the recovery by most hospitals from the financial obligations / disaster imposed by COVID will take nine to 12 months, and non-critical IT projects will be on hold until providers are more comfortable with their finances.
Epic lab
The contracts for all of the Epic consultants with my major Canadian provincial healthcare system are not being renewed. New consulting opportunities have dried up. Normally I’m constantly being contacted by consulting firms and new roles are quick to find, especially in Beaker, but it’s been very tough right now.
Back to normal, but a rough time between now and then.
Epic clinicals
My firm has had some contracts canceled or postponed, but they’ve also continued to get requests for resources. They have implemented a hiring freeze and implemented an across-the board pay cut. My work on my current contract has not changed
Not sure. My contract runs into next year, and since my work hasn’t really changed, I don’t think that it will.
Epic analyst
Stayed the same. I already consulted entirely remotely for my customer for the past couple years. Projects (non COVID-19 related) are still moving forward, though a bit slower than normal. I am a bit worried about my contract being up soon.
I can’t imagine any org will feel that on-site consultants at the analyst level are necessary on a regular basis. Especially consultants who the org has worked with in the past (with proven results and work habits). Possibly for higher level work, where face time is a bit more important.
Epic clinical / advisory consulting
I’m an independent consultant and I’ve already lost one future contract for a project that the healthcare system deemed “elective” even prior to the pandemic. I think there’s potential to be brought on in a COVID capacity due to my relationship, but with hiring freezes, it’s all the more daunting. I always try to provide value-based consulting and I have continued to do so through the pandemic, but I have found myself trying to prove my value more so during my current contract to ensure it’s not seen as expendable. I hate this behavior in consultants, but find it all the more necessary as active implementations are halting within other spaces at my current health system. My anxiety is definitely up. I’m hearing that the health system I work at has instituted the force majeur clause for several of their IT vendors. I have a couple outstanding invoices but am taking no news as good news for now.
The run-of-the-mill Epic-certified analyst-level consultant will move to managed care or salaried positions at lower rates with the big firms. There will be a market opportunity for firms to cash in on back-to-normal type activities. I expect management consulting will win many of the larger contracts, with the Epic consulting firms scooping up the staff aug opportunities with the new, cheaper work force. There will be more open IT positions as some clinical staff will have returned to floor. Obviously more remote work and less travel. That’s a given.
Epic analyst
Personally, I have gone from 75% remote to 100% remote. They have not involved me in very much COVID-related build, and the non-COVID work has started to dry up. We have been assured that they are not planning to let us go, but I am skeptical that they will be able to keep the current number of consultants when doctors and nurses around the country are seeing layoffs and pay cuts. I know I am one of the lucky ones, but I do live in constant fear of that luck running out.
I expect to be able to return to being on-site some of the time eventually. But I also expect the client to be trying to cut costs. Travel expenses and Epic optimization projects may be easy budget cuts, so I am anticipating either my contract ending early or just not being renewed. Now that WFH has been established and the IT sky didn’t fall, I hope that clients in general will be allowing their FTEs more remote time as part of “normal life” and that will also translate to more consulting projects that are 50% or more remote. In my experience, customers who are not WFH-friendly have an issue with trusting their team to get the job done when they are not being monitored in person. Maybe now they will realize that some folks are happier and more productive when they don’t need to spend hours every day commuting and dealing with office environments. Being open to WFH can allow you to hire and retain the best workers with the skills you need, regardless of their geographical location.
Epic OpTime
So far no change in my work, but at the beginning of March, all travel was suspended for three months. I’ve started totally remote and all staff at the client are also working from home through at least May. My firm has been communicating a great deal during the pandemic and not saying much at all. We received an email addressing benefits for those whose engagement was cut short, so that isn’t a good sign. They didn’t do much for those that are finding themselves without work.
I think it’s quite likely that we’ll be seeing more remote opportunities once they have worked with staff remotely and see the cost savings.
Full practice management consulting soup to nuts, EMR specialists
Because we are not solely reliant on our EMR consulting work alone, we’ve been very busy helping private practices with their layoffs and PPP loans. In 2009 when the economy collapsed, most of my income was Centricity consulting, I had to lay off most of my staff, it was crippling. The lessons I learned from that near financial ruin: 1. Have some recurring revenue, so we resell products we were already consulting on (I used to think being a pure consultant with no financial ties was admirable, now I realize it was naive!). 2. Diversify products, don’t be a single product consultant. We consult on several and sell/support Aprima. 3. Let your best customers know what this means to your business. My larger Centricity groups did not want to lose their access to me and my team, so we worked out ways to keep working that they could afford.
Because I made the necessary changes in 2010, I think we will be pretty close to back to normal when this is over.
Epic
My client was one of the first major hot spots and I asked to stop traveling near the end of February because I was concerned. Now everyone is required to work remotely. Contract extended.
Not at all
Epic inpatient
I was brought on for a hospital implementation, and a month into the contract, I was let go. I’m lucky that I worked as a FTE for a while so I can collect unemployment. I do believe with the stimulus contractors will be able to as well. Working in the consulting space we all should have a decent nest egg as contractors end unexpectedly a lot. I’m in the process of doing house projects, selling stuff I don’t need, and hoping we get back to a “normal” in July
I think companies will shift more consulting roles to remote to help cut down on travel costs.
Epic and Cerner
Projects that had a runway for continuation with a backlog of work, such as build or testing, have continued. But all new projects have been put on hold. Once the work that is scheduled is complete, then those projects will be put on hold pending next phase.
I think it will take a while for health systems to return to normal as they assess financials and timelines for projects. The bottom line I think a lot of consultants will be on the bench for the second and third quarters.
Cerner build and training
Moved to 100% work from home/remote. Still enough work with build to sustain through end of April 2020.
Shift to more remote work
Epic upgrades
100% shut down
Slow return to work as it is unclear on how soon hospitals will allow contractors back into their physical spaces.
Epic
My contract is still on remotely, but others have been paused.
Hopefully more health systems will be open to remote work.
Safety
Most projects on hold/delay. Some remote work, but very little.
More remote work versus travel to save on costs.
IT operations, Epic and Cerner PM and clinical consulting
Working remotely the time. Doing Zoom meetings and FaceTime calls.
I’m not sure. As a clinician, we still need to physically touch patients to collect samples and administer meds / therapies / procedures. Telehealth is part of the solution, but it isn’t the complete answer. As usual, payers are lagging behind the providers.
IT strategy and project management
Clients have stopped or suspended the strategy projects all together. The project management engagements have shifted from implementation of new/upgraded technology to telehealth related projects and it is 100% remote. The work on most everything else has been suspended indefinitely, primarily due to the unknown financial situation of the organizations upon returning to “normal.”
Some of the work will return, but I believe the financial impact to healthcare is going to be very significant and longer lasting than the pandemic. Capital is going to be scarce and priorities will be on maintaining financial stability. Unfortunately that will mean fewer projects for consultants for quite some time.
EHR
I remain 50% billable working for my customer remotely, which is enough to keep my employed through my company. The other 50% of my time is spent brainstorming on how we can transform our company and offer value to our customers in the new COVID world. Implementations, upgrades etc, will pick up again and companies that can prove that that can offer value remotely will stay in the game. We are learning that we don’t need to be Monday-Thursday travelers to continue to provide value, we have to tools to be just as effective and efficient from our home offices.
I have been as efficient 100% remote as I was when I was spending $2K a week traveling on site. I think we will beef up the at home technology, Video, VPN etc. for our staff and provide customers with a cost effective, safe alternative to flying a team on site every week.
Implementations, optimization, and support with Cerner software
Project on hold, most consultants furloughed. Some were asked to stay at reduced hours.
Unsure. Most but not all things can be done remotely from home.
Large EHR implementations
Nearly all projects have slowed / suspended, delayed, some cancelled. Furloughs for employees imminent.
Remote work will continue with travel at half pre-covid levels. Existing projects will be restructured due to budget impacts and new projects will take longer to approve
Epic application analyst
Currently unemployed
Have had multiple interviews from local hospitals/IDNs prior to pandemic. No follow-up calls / meetings scheduled at this point as hiring activity has stalled.
Healthcare IT management consulting
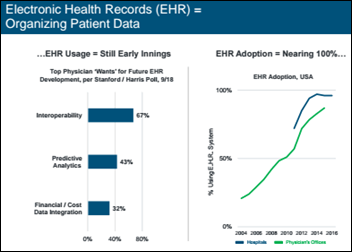
HIT consulting has already been down for the past two years given the disillusionment with the EHR investment and deteriorating health system margins. I am now on a project helping a clinical trial data management company develop AI use cases.
I don’t know. Doing work remotely is effective much of the time, but developing a deep relationship with the client still requires face-to-face time in various individual and group settings. I hope we get back to traveling and meeting as we did in pre-pandemic times but I’m not counting on it
Implementation, workflow analysis but not just for Epic
Basically, the pandemic has shut us down. We’re all working remotely, for longer hours because we’re all paranoid that if we don’t, we’ll get laid off. In the absence of consulting work, we’re doing a lot of cold calling to drum up opportunities in other areas that our firm has to offer. For example, we also offer online training that can be done remotely. This would be great for providers that are currently doing staff augmentation
I try not to think about it because it simply makes me depressed.
EMR
Delayed all projects to at least August and maybe out further. No layoffs yet
More remote work
Business and management consulting
Contracts cancelled or scope of work substantially reduced. New projects delayed.
Things will be slow to pick up. Customers will reevaluate priorities. Current project funnel will change substantially. Expect 12 to 18 months before any semblance of normalcy.
IT strategy, M&A, implementation, optimization, revenue cycle
Few projects are continuing. Expected work with post-implementation optimization and M&A conversions postponed indefinitely. University systems least impacted such as UK but that may change as states rethink budgets. Performance improvement, value-based care, PAMA AUC, and price transparency projects being pitched are not being sold.
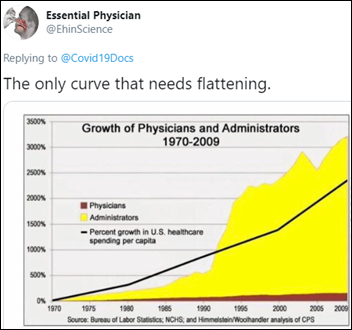
Will likely depends on how fast business and regulatory requirements re-enage. There will be a large pool of consultants competing for same work, driving cost per hour and associated wages down even further than had occurred already. Some staff aug firms that cross industries might have overhead and corporate costs covered by industries less impacted than health care, such as federal, banking or similar. Private equity backers of many of the current consulting firms may seek to shed firms during the pandemic or afterward. Some firms will be shuttered. Private equity investors will be fewer and harder to find. Public firms that had acquired firms will have large write downs of goodwill, although this already happened in last few years as HITECH dollars ended.
Part-time contracting for a health system for MIPS
Dwindling down. It was going to dry up anyway until later in the year.
MIPS reporting may be easier for 2020 so less need for my support.
Epic
Personally, busier than ever building out COVID-19 related facility structure.
Back to a less urgent routine. Upgrades, optimizations, hopefully some new installs.
Epic Bridges consultant
I took a 21% pay cut to my overall compensation
Hopefully more remote work!
Analytics project management
No client travel, working 100% from home. Hoping clients continue with projects
Regular travel to a client will no longer be required. I see travel dropping to once a month.
Pharmacy informatics
lient is occupied by COVID-19 planning and isn’t readily available for questions, etc. I was already working remotely, but because of travel restrictions, no site visits or physical assessments can be done. I don’t think there has been a significant impact to the consulting firm — yet
Hopefully, the client will be able to be more engaged with the project. I will still be working remotely but anticipate I will be working more hours.
EHR implementation project management
Working from home 100%, which I have done periodically throughout my consulting career. My projects are all still a go with the occasional delay due to COVID-19.
If the pandemic is controlled sooner, my projects should be back on track and ready to go forward. If the pandemic takes longer, there is a possibility that all work will stop.
Strategic
Evaporated
The bigger question is will it ever return at all. The tail of this is wide and long and the possibility that much will not return. Even with a willingness to return to normal, there will be no funds and resources to carry on as before. With every corner of society impacted, the available $$$ have gone. What returns will be small, focused, and highly limited. Hopefully, the majority of any future healthcare spending will be on clinical expenditure and not in non-essential administrative crap


































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…