Michael Raymer is CEO of Vitalchat.

Tell me about yourself and the company.
First, I just want to thank you for saving a lot of lives during COVID. Your post about Co-Vents, the not-for-profit that I set up to get refurbished ventilators into the field early in the pandemic, allowed us to connect with the Stryker family, which funded our efforts. We estimate that we saved 20,000 lives, and that all started at HIStalk.
I think you call me the timeless veteran of healthcare. I’ve been involved in large companies driving big innovations, such as GE Healthcare and Microsoft. I spent the early days of my career working on ventilators at Nellcor Puritan Bennett. Since I closed the days of Microsoft, I’ve been focused more on earlier-stage companies. I sold my last business, Pro-ficiency, to a publicly-traded company last summer and joined Vitalchat in October of last year.
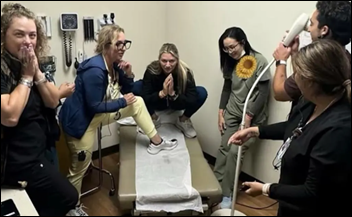
Vitalchat is a flexible, AI-driven audio and video platform that enables nurses to practice virtually, and supports procedural telehealth. I joined because video is probably the most underutilized signal in healthcare. We have all sorts of data, more data than we can use. But when you combine video with data, it can enhance the care delivery process.
I’ll also mention that I write a weekly blog post on LinkedIn for those who would like to follow my thoughts about healthcare, strategy, business, and people.
How does a health system use ambient, AI-driven monitoring to enhance nursing capacity?
We have automated nearly 70 workflows. Our implementation teams identify the workflows that are the easiest to implement with the greatest ROI, which may vary by health system. Common uses could be the safety check where you match the IV bag to the patient, which typically involves two nurses being in the room. When you use virtual technology, you can have the nurse at the bedside complemented by the virtual nurse remotely, who is able to zoom in on the IV bag and also the patient ID band to make sure right patient, right medication, right time. That’s just one of 70 workflows that we support with health systems today.
One of our key accounts is University Hospitals in Cleveland. Their first 150-bed pilot cost them $1 million to implement and they generated a $10 million savings over the first year. Now they’re on the pathway to roll it out across the entire healthcare system. Every day they are encountering a new potential use case for the product. That’s what’s so exciting about bringing in under-penetrated technology and to see all the possibilities for improving care for patients. That’s what it’s all about.
Can the technology bring nurses back into the workforce who left due to physical or geographic limitations or frustrations with floor nursing?
Absolutely. We see that the most successful virtual nurse is one who came from the floor and knows some of the other caregivers on that floor. But most importantly, they’ve seen almost everything that could happen in the care of patients. They are a steadying hand supporting the nurse on the floor.
We have heard many stories in our customer base about nurses who likely would have retired or pursued a different career, but took advantage of virtual nursing to continue to provide their unique skill set to health systems. That’s very gratifying. We have a projected shortage of almost a million nurses by the year 2030. If this can help stem the outflow of nurses outside of the hospital, that’s a great thing. We are seeing lower turnover rates and higher nurse satisfaction with having our virtual platform in place.
Do hospitals usually rotate floor staff, or are the virtual nurses people who don’t work regularly in the facility?
I don’t want to generalize, but these are not roles that are being filled by traveling nurses. They are clinicians who have worked in the healthcare system and are well trusted. Some of our sites have a rotation, where they may be three weeks in the virtual care operations center and another week on the floor. That keeps the connection with the clinician on the floor and allows them to understand how they could even be more effective in the virtual command center. That’s a good model for those who are physically able to go back to the floor.
It seems that skilled nursing facilities would be a good use case, although they have limited financial and technological capabilities.
I spent time in my career in the skilled nursing space, which is certainly economically challenged. A variety of use cases can be positive, including medication administration. You typically don’t have an onsite pharmacist, so the ability to have a remote pharmacist interacting with the patient and the physician onsite. You have issues of patients who are worried about falls, such as a movement in the room that might indicate that the patient is trying to get out of bed when they have been deemed a fall risk.
There is significant opportunity in skilled nursing. The issue is the price point. Because we’re agnostic to the hardware platform, we believe there will be an opening for us ultimately in the skilled nursing space, but we’ll probably follow that through the channel of our customers as hospitals. In fact, this week we had a great discussion with one of our customers going out into the home with that subsidiary. We can scale the hardware appropriate to the particular situation, so it could be a great fit.
The Big, Beautiful Bill will allow more money to be funneled into the rural healthcare system, where 25%-plus of the patients in this country are taken care of. The bill allocated $50 billion to technology like Vitalchat provides. Being able to allow that patient to remain in that remote facility supported by a specialist in the tertiary care academic centers was brilliant in the bill. The patient wins. The remote facility wins, because they’re able to keep that patient. The patient’s family wins, because they aren’t having to travel long distances in support of a loved one.
At the same time, the healthcare system can get reimbursed for the specialist care without them physically having to be on site. If necessary, the patient can be transitioned to that academic medical center. Fully implemented, the vision of that is particularly powerful, and you can extend that analogy to skilled nursing.
Is your technology’s footprint light enough to avoid a rip-and-replace of existing technical and physical infrastructure?
One of the technology constraints is bandwidth consumption. We have patents in video compression that allow us to be a very quiet signal on the hospital network. We move the AI to the edge and do not use cloud resources to process that video. Response time is outstanding. We wind up not being traffic on the network that’s going up to the cloud to implement AI or ambient learning from that video signal. Reusing hardware that’s already in the facility.
We recently created a solution for customers of ProConnections, a tele-ICU vendor that closed late last year and left their installed base abandoned. Because our platform is flexible and hardware agnostic, we created a solution where we provide software on their existing hardware platform so their customers can continue to use that product in monitoring patients.
What opportunities does AI offer in analyzing video without requiring human eyes?
The future of care is ambient. You see a lot of announcements in the ambient speech space. It will be more and more assistive over time. We were talking with one of our customers today about a dietary use case. Looking at the plate that’s delivered versus what it looks like when returned, then being able to assist nursing with caloric calculations and the I&O workflow sheets that nurses manually fill out today.
There is such tremendous opportunity to look at workflow as the technology improves. The AI engine, in our case, is easily trainable. I can’t even conceive of all the use cases. Today the dietary one came up and I never even thought of that as a potential use case in the acute care setting. It’s a big time-consumer for nursing. It would give them more time to spend on patient care and not documentation.
Today, it’s 70 use cases. A year from now, it will be double that number that will be proven to add value.
Are the companies working in this area of video analysis specific to healthcare? Also, how do you sort through those many use cases and decide which ones to go after first?
The platform that we built is easily trainable. In fact, we began using NLP as a test case for allowing a clinician to build the kinds of things they want to observe in the room. Our ambient AI engine will process requests by the clinician and provide them immediate feedback. There’s not a lot of software work that we have to do to enable new workflows.
A health system has super complex workflows. If you are shifting something from an in-room activity to virtual-based, everyone on the care team needs to understand that. There has to be the appropriate accountability, both for the nurse in the room and the centralized command center.
Most of those workflow challenges are not software issues for us. They are workflow challenges for the health system that are not unlike originally implementing the modern EHR. A tremendous amount of workflow design was done. The beauty of our product is we don’t have to build flowsheets. We don’t have to build order sets. We are insulated from the inherent complexity of an EHR.
We don’t see a lot of big companies in the video space. We see companies much like Vitalchat. A lot of people saw the headlines last year in Stryker’s acquisition of Care.ai and the vision of merging the device company with visual insights. We believe that being Switzerland is a better strategy, not being tied to just one vendor. It allows us to work with Epic, Oracle Cerner and devices in the patient room and in the OR.
The space is interesting. It is not just the AI ambient technology, but also the wrapper around it. The complexity of running video and audio from a patient room is non-trivial. We have been able to bulletproof our platform. I call it a self-healing technology, where our uptime is up from three nines to four nines now for our in-room cameras. If you’re going to rely upon this technology 7×24, it has to have that amazing reliability. That may have been the most difficult challenge technologically, getting the uptime to be there that is necessary to deploy at scale.
We started out talking about COVID and Co-Vents, which brought back unpleasant memories of patients dying in locked-down hospitals with families having their last moments with their loved ones via an IPad. Can technology like yours improve the experience of patients and families and not just that of clinicians?
That is a very personal issue for my wife and me. We lost my mother-in-law during the dark days of COVID. They would not allow my wife to come in the hospital to see her. There was not any kind of technology that allowed us to even have an interaction with her. Fast forward to today, that has softened the landing of this technology in patient rooms, because patients understand video consults now. FaceTiming with family members and similar tools are mainstream.
I heard a great story two weeks ago where one of our customers was able to have a patient in the hospital be a participant in a wedding. Not just viewing it, but actually having two-way audio communication with family members in the wedding while the patient was in the hospital. We hear story after story where our technology has allowed that patient to connect not just to caregivers in a health system, but also loved ones, and to have loved ones join consults at the bedside from remote across the US or across the world.
What are your plans for the company over the next two or three years?
My primary job as CEO is making sure that the rate we’re growing will allow us to have both the monetary and people capital that are required to support our customers. The good news is that I have a very big Rolodex. When we have a need inside the business, it’s easy for me to reach out to my network and plug individuals in immediately who can make a difference for our customers.
This is an exciting space. A strategist would call the inpatient virtual nursing setting a $2 billion total addressable market. You have less than 5% of the beds in the US that are penetrated with video and audio. That’s a significant opportunity for us to make a difference. It’s exciting to be early and exciting to have unique capabilities in our platform that will allow us to sustain impressive growth over time.
Comments Off on HIStalk Interviews Michael Raymer, CEO, Vitalchat



































































I find it incredibly ironic and rather hypocritical that the co-founder of an Epic-centric consulting firm is calling for the…