EPtalk by Dr. Jayne 2/22/24
Many parts of the US are starting to emerge from winter weather, and the healthcare IT folks are starting to emerge from their relative slumber to head into spring conference season. ViVE kicks off in Los Angeles this weekend, and if you didn’t register as an early bird you’ll be shelling out $2,995 for registration. Compared to that, HIMSS looks like a bargain at $1,675, although the ViVE people will remind you that their registration also includes breakfast and lunch plus its “Industry Night” celebration, although I haven’t yet seen mention of the headliner for that event.
Conferences have gotten expensive, and even the non-flashy ones will cost you a decent chunk of change. I’ll be attending a more academic/professional-focused conference later this spring, and when you add up all the costs – registration, travel, lodging, and meals – I’ll be spending at least $2,500 to attend, not to mention the cost of the time away from work. Sure, I’ll be getting some continuing medical education credits, catching up with friends, and doing some networking, but even if your employer is willing to subsidize your attendance at conferences, it’s hard for physician leaders to justify going to more than one per year. One of my local health systems still has a so-called “travel ban” in place, mostly due to finances rather than concern about infection control or staffing. Seems to me like just one more thing being attributed to the “new normal” post-COVID.

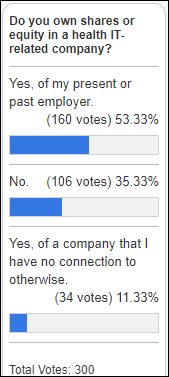
Nearly everyone around the virtual water cooler today was talking about Teladoc Health’s stock tanking Wednesday. The company released its financial results after the close of the market Tuesday, and the market provided its answer as the stock slipped lower. Like every company, Teladoc has had its ups and downs, but growth has slowed over the last three years despite a rise in consumer demand for virtual care services. As is the case with many companies, the combination of bad investments and bad management are difficult to overcome. Telehealth is a tough business to be in, especially when you’re trying to meet not only the regulations of 50+ US states and territories but also those of an international market. We’ll just have to see what the next couple of quarters brings for this company and whether its future can be salvaged.

For organizations participating in the Centers for Medicare & Medicaid Services Merit-based Incentive Payment System (MIPS) Quality Payment Program (QPP), the data submission portal is now open for the 2023 performance year. Eligible clinicians have until April 1 at 8pm ET to submit their data via the Quality Payment Program sign-in page. If you don’t already have your login information, I’d recommend starting that process now even if you don’t have your data ready for submission, as it can take a couple of weeks to get access sorted out. For those of you submitting, I’d be interested to hear how the process of data preparation is going. If you’re relying on vendors to help you get the data ready, when do they project you’ll have it? Or are you having to do the entire lift yourself? Feel free to send your anonymous feedback about the process and we’ll share it with readers.
A movie that has stuck with me over time is “Up In the Air” starring George Clooney. For those who may not have seen it, Clooney’s character Ryan Bingham works for an organization that helps companies outsource corporate layoffs. He has a variety of ways to help label what is happening to impacted employees, along the lines of “making you available to the workforce.” A reader shared a couple of examples from recent layoffs: Citi recently referred to the loss of 20,000 jobs as helping to create “a simplified operating model” and UPS described 12,000 layoffs as trying to “fit our organization to our strategy.” Other bad phrases I’ve heard include “involuntary career event” and of course the dreaded “rightsizing.” The worst I heard recently was when American Airlines labeled their January call center layoff as a way to “better serve our customers.” Anyone who has ever waited in the interminable phone queue understands what an oxymoron that is.

Here’s another solution in search of a problem: The American Board of Family Medicine has created a new Digital Credential program, designed to provide physicians with a way to share their board certification status “through a live online platform” targeted for social media, email signatures, websites, and more. It also offers the option to add the credential to mobile wallets, “allowing you to quickly share your board-certified status on the go.” The number of times that anyone other than a Credentials Verification Organization has requested proof of my board certification is zero, so I’m not sure physicians were clamoring for this. I tried to use the system’s functionality to automatically add the credential to LinkedIn, only to have it try to add my board certification with today’s date rather than the actual issuance date many years ago. I’m still shaking my head and wonder how much our professional organization spent on this.

Baptist Health South Florida is using the fact that February is American Heart Month to offer “special pricing” on CT Calcium Scoring tests. Patients without insurance (or those who have insurance that does not consider the test a covered service) can have the test for $49 as long as they have a physician order. For those of you who have insurance and have not met your deductible, you’re on your own to figure out how much it will cost. I’m in favor of making healthcare accessible to all, but I don’t like the idea of a hospital organization using this as a loss leader to attract patients who might potentially need more costly services. These are people’s lives – not a rack of rotisserie chickens at Costco.

Many of the patients I see are struggling financially, so I’m always looking for free resources that will help support their health goals. I stumbled upon this video from the National Health Service in the UK and was immediately drawn in since it promotes belly dancing as an aerobic workout that can help improve flexibility and core strength. It also advertises mood-building benefits through music and exercise. If you’ve got 45 minutes to spend on your health, it’s worth checking out. The video does include a disclaimer that the program is “suitable for most people in good health with a reasonable level of fitness” and that you should get advice from a healthcare professional before trying it if you’re not sure about your current level of fitness or if you’ve had recent injuries or health conditions such as a heart attack or operation.
What’s the best you’ve seen as far as free tools for health promotion? Is belly dancing your new breaktime activity? Leave a comment or email me.

Email Dr. Jayne.































In a nutshell, Epic says that this tortious interference stuff is getting tortuous, so let's just take a torch to…