Monday Morning Update 7/8/24
Top News

Oregon Health & Science University shuts down its Connected Care Center, the 16-nurse telehealth nursing unit that it launched at the beginning of the pandemic.
OHSU is eliminating 500 positions as it pursues an acquisition of Legacy Health, which would expand its footprint to 10 hospitals and 32,000 employees.
Reader Comments
From Peds MD: “Re: Epic Care Everywhere. A baby had a very high newborn screen for a condition where confirmatory testing and treatment need to be done urgently. The baby was tested within an hour at a local hospital, using the father’s last name. Not having access to the other hospital’s Epic, I logged into the baby’s birth hospital record (Epic), which still had ‘Baby Girl’ and the mom’s name. I asked Care Everywhere to find the baby’s results. Epic said no match even though the date of birth, sex, address, and phone number were the same. Luckily the ED clinician at the testing hospital sent me the results via text. Just to get the records connected officially, the next day I got the Care Everywhere ID from the testing hospital and plugged it in. Again, no match! Learning lesson for Epic — if you have the Care Everywhere ID, which is an amazingly long set of numbers and letters, you should at least be asked ‘Is this the right person?’ And you shouldn’t even need that if other information is the same. I called it in to IT and got the famous ‘working as designed’ answer.”
HIStalk Announcements and Requests
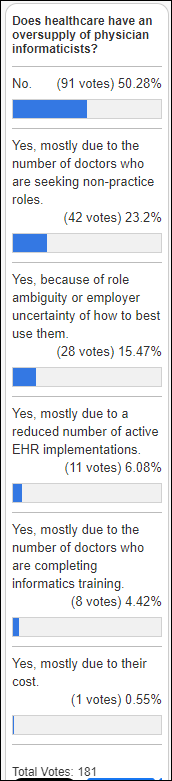
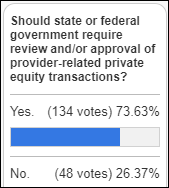
Poll respondents are evenly divided on whether an oversupply of physician informaticists exists, with those who say yes pointing to the number of doctors who are seeking non-practice roles.
New poll to your right or here: Who is most responsible for physician dissatisfaction?
Webinars
July 18 (Thursday) noon ET. “New CMS Final Rule: Strategies to Get EHR and IT Vendors Up to Speed.” Sponsor: DrFirst. Presenters: Nick Barger, PharmD, VP of product, DrFirst; Tyler Higgins, senior director of product management, DrFirst. The new final rule that was issued by CMS on June 13, 2024, goes beyond a basic upgrade of SCRIPT standards and improves care connections among doctors, pharmacies, and patients. The presenters will lead EHR and IT vendors through the final rule, provide details on key provisions and compliance deadlines, offer tactics to tackle roadmap development, and provide direction on where and how partners can best leverage the requirements for the benefit of their customers.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock

Private equity firm New Mountain Capital proposes to buy R1 RCM and take the company private at a valuation of around $5.6 billion. RCM shares are down 38% over the past 12 months, valuing the company at $4.6 billion.

California’s attorney general approves UCSF Health’s acquisition of Dignity Health’s Saint Francis Memorial Hospital and St. Mary’s Medical Center, with terms that include UCSF Health spending at least $80 million on their EHR.
India-based hospital operator Narayana Health launches a Kaiser Permanente-type health plan that covers a family of four starting at $10 per month, which is about 20% of what private insurers charge. Founder, chairman, and cardiac surgeon Devi Shetty, MBBS says that Indian citizens need 70 million surgeries per year but only 20 million are performed due to lack of affordability, which he says causes many times the deaths of malaria, TB, and HIV that are covered by government programs. The policy’s benefits include treatment coverage of $6,000 and surgical expenses of $120,000. The company promises easy claims settlement, coverage of preventive checkups, and discounts on tests that are performed at Narayana’s hospitals. Thanks to the reader who sent this item my way.
Sales
- Shepherd Center will implement Kemtai’s computer vision AI assessments for people with brain injuries.
People

Primary care network Main Line HealthCare (PA) names SVP/CMIO Donald Klingen, MD as interim president.
Announcements and Implementations

Bath Community Hospital (VA) goes live on Meditech Expanse.
Australia-based telemedicine service My Emergency Doctor implements InterSystems HealthShare Health Connect Cloud for interoperability with a major suburban hospital to perform virtual overnight supervision.
Government and Politics
National Coordinator Micky Tripathi, PhD, MPP and FDA Director of Digital Health Center for Excellence Troy Tazbaz resign as non-voting members of the board of Coalition for Health AI to avoid potential conflicts of interest. Republican lawmakers criticized FDA’s involvement with the group last month, citing concerns about potential conflicts given CHAI’s membership that includes major technology companies and health systems that develop AI businesses.
Privacy and Security

Palomar Health Medical Group (CA) notifies patients that their information may have been compromised in a May 5 cyberattack, but says it doesn’t yet know which patients and which information was involved. PHMG originally hoped to restore most of its systems by July 1, but now is targeting mid-July.
The RansomHub ransomware group claims to have publicly posted 100 GB of information that it stole from the systems of the Florida Department of Health, which declined to pay the ransom that it demanded in accordance with state policy.

An Ascension Saint Agnes Hospital NICU nurse is forced to use a fax machine for the first time when clinicians lost access to the EHR during Ascension’s cyberattack. She says that staff weren’t prepared for a four-week systems outage, when patient medications were tracked on a shared spreadsheet that was faxed to the pharmacy.
Other
The FDA orders North Shore Medical Center (FL) to stop performing mammograms, determining that the facility’s tests failed to meet American College of Radiology image quality standards. The hospital has contacted all patients who had the tests over a two-year period to advise them to have their results re-evaluated and possibly to have the test repeated. The hospital, which is owned by the bankrupt Steward Health Care, will cover the cost if the patient has the rework performed at another Steward facility.

“Jeopardy!” fans debate the decision by host Ken Jennings to accept the answer of contestant and Mary Washington Healthcare IT application coordinator Matt Brooks, who mispronounced “larynx” as “larnyx.” He eventually won the game. Some fans were appalled that Jennings accepted his answer given that it is equivalent to misspelling the word, while others said that the mispronunciation is common in the South and Midwest and noted that former host Alex Trebek had accepted the same mistake in 1997 and 2006 in explaining that a lot of people say it wrong.
Sponsor Updates
- Black Book Research’s latest survey of health plans ranks Surescripts as the top technology solutions provider for payer member safety, PBM, and pharmacy solutions.
- In Belgium, AZ Sint Lucas and AZ Sint Jan hospitals implement Sectra’s One Cloud public cloud service.
- Over 400 Konza-powered sites achieve and/or maintain Validated Data Stream Designations in NCQA’s Data Aggregator Validation Program.
- Meditech customer Humboldt Park Health becomes the first Midwestern hospital to achieve Healthcare Equity Certification from the Joint Commission.
- Nordic releases a new “Designing for Health” podcast, “Interview with Jeff Mounzer, PhD, and Peter Kriss, PhD.”
- Optimum Healthcare IT names Brad Sourwine (Pivot Point Consulting) director of recruiting.
- Sana Kliniken in Germany implements RLDatix’s cloud-based workforce management solutions across the enterprise.
- Waystar will exhibit at the EClinicalWorks Denver Day Show July 10.
Blog Posts
- Inovalon Backs Safer Care: Answering the PCAST Call (Inovalon)
- Maximizing the Value of Your Time: Billing for Linus Health Digital Cognitive Assessments (Linus Health)
- Healthcare CFOs Highlight the Need for End-to-End Digital Solutions (Medhost)
- Unraveling the Financial Ramifications of MSSP ACO Reporting (MRO)
- Physical Therapy Billing Units: A Comprehensive Guide (Net Health)
- The Future of Physical Therapy Documentation Software (Netsmart)
- Nurses of Note 2024: The Clinical Nurse Educator (PerfectServe)
- Optimizing Physician On-Call Schedule Management (QGenda)
- Data intelligence for all: a recap of new solutions and key takeaways from Databricks’ 2024 Data + AI Summit (Redox)
- Attracting Top Tech Talent to Healthcare: Strategies for Success (Revuud)
- Opening the Door to the Patient Cost Conversation – and to Affordable Medications (Surescripts)
- From Vision to Reality: Healthcare Leaders Share Their Vendor Compliance Journeys (Symplr)
- Moving to Meditech Expanse? Five Key Support Considerations for Post-Implementation (Tegria)
- Navigating the Complexities of Outpatient vs. Inpatient Billing (TruBridge)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




































I believe it is this: https://www.investopedia.com/terms/w/warrant.asp So an option, but one provided by the original company.