Theresa Meadows, RN, MS is CIO in residence at Symplr.

Tell me about yourself and the company.
I have been in healthcare my entire career. I started as a nurse in cardiac transplant and interventional cardiology and ended up in IT by accident. Over the years, I’ve done various roles in consulting companies and software companies. Before Symplr, I was the chief information and digital officer at pediatric institution for 15 years, and with Ascension Health prior to that.
At Symplr, I’m excited because I get to do a unique new role as the CIO in residence. That means that I get to bring insider baseball to Symplr, meaning how healthcare CIOs think and the needs that healthcare institutions have. I get to help them with customers, building relationships, and doing the fun part of the CIO job, which is collaboration, building relationships and trust, and forming strategic directions. I’m excited about being here.
How do you define success in your job?
For me, it’s of course always having happy customers, meaning customers who are satisfied with the services and the software that we provide. That is how I would measure success. Hopefully being seen as a leader in the industry. Looking at our NPS scores and other ways to understand customer satisfaction, getting feedback, and making sure that we are listening. These are all ways that I evaluate how I’m helping the organization as the CIO.
How have you seen the CIO job change in the past few years, including the creation of new C-level roles that have a technology focus such as chief digital or chief transformation officer?
There has been tons of evolution. I can remember early on that the role was technology focused. We would spend a lot of time talking about product, functionality, uptime and downtime, and those types of things.
With the transformation of going to the electronic health record and COVID even, we moved into more of an operational role. I saw my role become more about operations, understanding how hospital systems work, and providing solutions to challenging problems, versus being the technical leader. It has evolved over time to be a strategic position.
All those new C-level roles are important. How we partner with those roles is important. I don’t want to minimize the fact that a CIO can also be transformative. But having additional people who support a technology vision that can drive strategy and the technology that supports that strategy, the more people you have on board with that, the easier the CIO job becomes. We can have partners who are helping transform the organization.
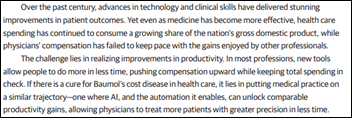
Some clinicians in big health systems would argue that their level of burnout increased with EHR adoption because it was used as a corporate control mechanism rather than to improve their capabilities or patient outcomes. Will the rollout of AI empower clinicians or just be another way to enforce administrative rules and boost margins?
We have learned from our mistakes or sins of the past, if you might say, of how we collaborate with clinicians. With artificial intelligence, that collaboration is going to be critical. Only clinicians know if the AI is doing the right thing clinically. As we get into more and more clinical use cases, having those partners of nurses, physicians, and the whole clinical team to weigh in on how we know that the AI that we are using is safe, effective, and creating the outcomes that we need.
We learned a lot during COVID about burnout and how to start addressing it. Adding more to-do’s to clinicians’ plates is not going to be how we get there. We have to find ways to remove things from their plates and get them back to doing the things that they love, which is patient care, interacting with people, and creating good outcomes. I hope that AI will allow us to do that.
How will the tension be addressed between using these new tools to make the physician’s day better versus increasing patient loads, which would increase margin while shortening appointment lead times?
Ultimately, if we do the right things, productivity, revenue, and those types of things follow. If we can find ways to make our clinicians happier in what they’re doing and revamp the tasks that they are doing, I think we will see revenue improvements. We will see patient experience improvements, because people are happier in the roles that they’re doing versus thinking about it the other way, which is that we have to see more people.
Most clinicians appreciate that the ability to get into health systems is difficult today. The average wait time is long. How can we see more patients and make our patients happier? If technology can support that, that would be ideal, but I don’t think that we can go into the conversation with the goal of seeing more patients. Our goal should be how to make the process more efficient, better for our patients, and better for the clinicians. The revenue returns will follow.
A recent KLAS report found that EHR issues, particularly duplicate and unnecessary documentation, influence nurse burnout. Could the flow sheet process be improved?
I agree with that. At my previous organization, we did the nursing collaborative through KLAS, and we saw exactly that. We have created the note bloat scenario in nursing. If we need to capture data for a quality project, we add more documentation. But we never take documentation away.
As we start adding things to the EHR, we need to be thoughtful about the purpose of that documentation and how will it be used. We spent a lot of time in my previous organization looking at and optimizing nursing documentation. A lot of duplicate documentation exists in flow sheets, and we overuse flow sheets to capture data that could be captured in other ways.
Health systems are rolling out AI without a strategy, governance, or regulatory guidance. Will they get burned or is this just the natural cycle of a new technology?
I think it’s probably the natural cycle of a new technology. We get excited about things that we hope will improve outcomes for our patients and our caregivers. We go at it hard initially because we think it’s going to change something. Then we realize that with every good technology, you have to consider the people in the process. AI is no different.
The challenging thing with artificial intelligence is that we haven’t spent a lot of time looking at our data, our data structures, and what data will be used to generate those AI models. Healthcare has been notorious for collecting lots of data, but that doesn’t mean that it’s quality or good data.
The challenge that we as a healthcare industry have to figure out is how to get the right data into these tools so that we can see the appropriate outcomes. That’s where people start getting nervous about diving too deep into AI, because they know that the data that they are using may or may not be the most structured or clean data that they could be using to make decisions. You see most organizations focusing on that. How am I going to get the right data so that the model works the way it’s intended to work?
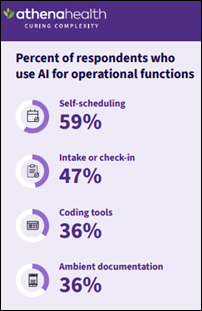
How are health systems evaluating the use of AI? Are they emphasizing output rather than outcomes by focusing on revenue cycle and productivity that generates ROI?
I would love to say that the answer to that question is yes. We would love to see productivity benefits and ROI. But right now, we are still in that learning phase of what we are trying to improve.
A lot of process improvement goes hand in hand with deploying AI, so a lot of learning is happening. Sometimes when we think we’ll see ROI, what we really learn is that the process that is driving the data is broken. To get a good outcome, save money, or do whatever we think the right thing is, we have to go back and reevaluate that workflow that we were doing as part of the process.
AI helps us get us to that solution faster than in previous worlds, where we weren’t sure if it was workflow, the data, or the tool itself. AI helps us get to that decision-making process a lot faster, and then we can address those issues quicker.
Early technology such as EHR focused on technology that supported doctors since they are making the decisions that impact the bottom line. Will we see the emphasize refocus on the less-penetrated area of technology that supports nurses?
It is super exciting that we are now talking about the nursing profession and how to help nurses be more efficient and effective. The nurse is the center of all things when it comes to the patient interactions. Anything that can help automate nursing tasks through AI and assist with prioritization will be a win for nursing.
Ambient listening for nursing will eventually be a huge win. The challenge with nurses is that we don’t typically talk about our assessments out loud with a patient, and we don’t talk about them in a way that would generate documentation. A lot of change management has to occur when we go to ambient listening for nursing. But once we figure some of those key words and phrases, nurses will adopt that quickly.
Nurses are resilient. If it’s a good process or a good product, they will adopt it. They adopt really crappy products sometimes and make them work. They are very resilient in that way.
We have an opportunity to look at nursing tasks, how we automate them, and how to give the tasks to the right person on the clinical team. Sometimes we give tasks to nurses that could be done by a nursing assistant, an MA, a unit secretary, or a unit clerk. There are ways to do that. AI can help with some of those workflow processes and getting the right task to the right mailbox.
A lot of opportunity still exists in the space between the EHR and the ERP. Hundreds of applications haven’t been optimized or looked at, and those are all falling in the operations space. There is also an opportunity to improve those processes where we haven’t spent a lot of time yet. There’s a whole vast array of applications, workflows, and processes that the EHR or the ERP doesn’t touch. There’s plenty of opportunity in those areas for the future as well.
Will nurses need to vocalize or dictate what they’re doing to support ambient listening, unlike physicians who can mostly carry on normal patient conversations and let AI do the work?
For physicians, it’s natural. They dictate it all the time through their whole career. That’s been their process.
For nurses, when we talk to patients, we are trying to do the education piece and less the documentation piece. It’s going to be training a nurse on how to say some of the key findings that they ordinarily would just document or check a box and then educate a patient, building that into the education. Talking to the nurses and figuring out that style.
The change management pieces are going to be something different for nursing because we focus a lot on education and making sure the family or the patient knows what the next right step is, versus talking about the assessment out loud.
How will virtual nursing programs affect nurse shortages?
Virtual nursing is a huge win. I am a huge proponent for virtual nursing for a number of reasons. The first is that we can capitalize on nurses who may be ready to retire later in their career, where the physical part of nursing is hard, but the intellectual process is still intact for them. Virtual nursing allows us to have some of our more seasoned nurses be able to help some of the newer nurses by being there virtually for them as a resource, to watch things on the unit, and to see how things are going and give input.
It is also a good tool for addressing burnout, because you can create schedules to have people rotate through virtual nursing so that they aren’t at the bedside every day. They can rotate through those different scenarios and learn a different skill set.
It’s better overall for patient care, because you have people who are observing what’s going on in each patient room, and you don’t have that today. Some of the safety events that have occurred can be mitigated through a virtual nursing process. There’s lots of opportunity to reduce handoffs and reduce the need to have two nurses in a room for certain processes.
There’s a lot we can still learn from that process since people are pretty early on in their deployments of virtual nursing. We probably haven’t seen all the benefits that can be accomplished through those programs just yet, but we will.
Medicaid cutbacks, the elimination of subsidies for exchange-sold health insurance, and the possibility of having more unemployed people who lose access to employer-provided insurance will likely raise the number of uninsured people. Are health systems planning for that, and do technology implications exist?
Health systems are absolutely planning for that. By nature, we are conservative beasts. If we start to see where there will be a challenge around funding, insurance, or people’s capacity to pay for medical care, we get more conservative.
Our choices around technology will be to look for items that will improve revenue capture, make our length of stay shorter so the cost is cheaper, and look at ways to be more cost effective and see more patients. We are going to be looking for those types of things, but we’re also going to be looking for ways that we might lessen the burden with more virtual care, remote care, where you’re not spending the large dollars on an inpatient stay. If we can take care of people remotely or hospital at home, organizations will look at those avenues, because the cost inevitably is cheaper in those scenarios.
How we maximize the resources that we have to deliver to the care at the lowest cost point is going to continue to be a focus for all organizations going forward, especially if we have a lot of cutbacks in insurance capabilities.
How do you expect healthcare and health technology to change over the next few years?
We will see people focus on ways to automate the workforce and automate having the right people on shift at the right time for the lowest cost. You will continue to see a lot of focus there.
We will also start to look at ways to augment our workforce. We will always need nurses, doctors, clinicians, and people, but how do we make them more efficient so we can do more with less? Automation should help us in those areas.
We will continue to see how we can educate the next set of providers, nurses, and other clinicians so they come out of school much more efficient using tools better.
There’s just a lot that we can do, and we will see this evolve. I get excited, because having done this for the last 25 years, the technology has finally caught up with the workflow things that we need. We will start to see advances more rapidly than we’ve ever seen. I’m excited about the things that we will be able to do in the future with where technology is today.
Comments Off on HIStalk Interviews Theresa Meadows, RN, CIO in Residence, Symplr


























Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…