Mr. H posed a question last week about how to streamline training for PCPs and asked me to weigh in as well.
To really answer the question, we have to ask ourselves what we as a society actually expect primary care providers to do and what kinds of experience we expect them to have. The answers to those questions directly impact how we could best train people to share the primary care load.
To help mitigate my own bias as a board-certified family medicine physician with 20 years of experience, I looked to MedlinePlus (which is an official website of the US government) to define “primary care provider.” According to the site, “A primary care provider (PCP) is a healthcare practitioner who sees people that have common medical problems. This person is most often a doctor. However, a PCP may be a physician assistant or nurse practitioner. Your PCP is often involved in your care for a long time. Therefore, it is important to choose someone with whom you will work well.”
Some lay people might read that and think “common medical problems” are things like cough and cold, urinary tract infections, rashes, sprains and strains, and the like. Although those are common, those kinds of acute problems are only a small part of what primary care providers actually see. In a traditional primary care practice, we’re also caring for lifelong medical problems like asthma, diabetes, high blood pressure, heart failure, stroke, chronic obstructive pulmonary disease / emphysema, kidney failure, vascular disease, connective tissue disorders, cancer, neurological diseases, and more. Additionally, we care for more complicated acute problems like pneumonia, bronchitis, kidney infections, unusual rashes and suspicious lesions, and clusters of symptoms that don’t have a clear cause.
The latter is where primary care physicians really shine, being able to look at a set of related or seemingly-unrelated symptoms and pulling it all together to create a plan to diagnose the patient. That kind of clinical skill is far beyond evaluating cold symptoms and running a COVID or flu test.
The other thing that happens in primary care, but was not mentioned in the MedlinePlus definition, is the delivery of preventive health services. This is the part where we talk to patients about recommendations, present the options, discuss the risks and benefits and which options might be best depending on the patients’ other medical factors, and ultimately order the services. For a patient who is reluctant to undergo a screening test, this might involve ongoing conversations over a period of months to arrive at the point where a patient accepts a test.
Other preventive services include counseling on smoking, drugs, safe sex, diet, exercise, nutrition, mental health, family dynamics, and what to expect as you age. Speaking of the aged, we also have conversations about advance care planning. On the other end of the spectrum, those of us who see pediatric patients do a lot o bnf counseling and anticipatory guidance, making sure parents know what to expect as their children grow and what might be normal or not normal. Some days, we give a lot of reassurance.
In family medicine, we’re also trained to perform office-based procedures ranging from skin biopsies and toenail removal to joint injections to flexible sigmoidoscopy to colposcopy and cervical / endometrial biopsies. In some areas of the country, we provide full-spectrum maternity care, including c-sections. Some of us are trained to perform colonoscopy, and a small subset of us who have done extra training can even perform appendectomies and other urgently-needed surgical procedures. Most of the family physicians working at that level are either part of a residency / fellowship training program or are practicing in a more rural area, but it’s something that the majority of readers are likely not aware of.
Internal medicine training is similar, but with less of a focus on procedures and no care for infants, children, or pregnancy. Pediatrics generally covers people under the age of 18, but includes a full spectrum of conditions and procedures. Geriatrics is often left out of the primary care list, but as our population ages, it is becoming increasingly important.
That broad definition of primary care falls to the wayside if you listen to many of the talking heads in the healthcare industry today. They feel that primary care can be delivered in a transactional fashion without continuity, and don’t fully understand that when a patient has a lot of different seemingly-minor problems, they can actually add up to something much more significant. These organizations are happy to hire people who aren’t even trained in primary care to deliver primary care services, as long as they’re willing to work for cheap. You don’t have to be board certified when patients are paying cash. (Generally, you do have to be board certified or at least board eligible if you’re being added to insurance panels.)
The definition also morphs a bit when primary care providers become employed by organizations that see them as little more than referral mills, sending patients to subspecialists who perform high-dollar procedures. One of my primary care colleagues who works for a hospital-affiliated group was recently scolded for not sending her diabetic patients to an endocrinologist. Guess what? Her patients have excellent glucose control, are on evidence-based regimens, and aren’t having side effects. That combination of factors means that referrals weren’t warranted. The organization tends to make more money on patients when they are referred to endocrinology, though, so they weren’t happy.
Another role of primary care providers, according to MedlinePlus, is to “assess the urgency of your medical problems and direct you to the best place for that care.” When we actually know you (which means you’re probably not getting your care from a transactional non-continuity entity) we can better assess your symptoms and determine if you can see us in the office on Monday, whether you can go to an urgent care tomorrow morning, or whether you need to go to the emergency department immediately. That’s not to say that a primary care provider who doesn’t know you can’t do that assessment, but from experience, that’s when I see the most patients sent to a higher level of care than they need, usually at a higher cost.
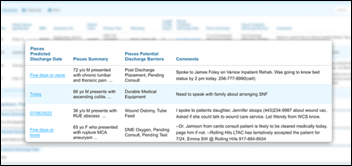
Many primary care providers also see patients in the hospital, although that’s becoming less common every day. Being able to manage hospitalized patients in an environment where the goal is to get the patient out of the hospital as quickly as possible becomes difficult when you’re also seeing patients in the office. That has led a large number of primary care providers to turn over the care of their hospitalized patients to “hospitalists” for inpatient management. Sometimes this results in better coordinated care, sometimes it results in more disjointed care, and I’ve seen the whole spectrum. In an ideal situation, the hospitalists have close relationships with the primary care providers and coordinate discharge and follow up, but there can be misses when the focus is on patient throughput.
Primary care physicians have a bachelor’s degree, four years of medical school for a MD or DO degree, and a minimum of three years of residency. They graduate training with around 20,000 clinical contact hours, which makes it much more likely that they will have seen rare diseases or unusual presentations of common diseases. Physician assistants have bachelor’s and master’s degrees and typically graduate their training with around 2,000 clinical contact hours. Nurse practitioners have a bachelor of nursing degree and typically graduate their training with around 500 clinical contact hours. Although in the past many nurse practitioners had extensive experience as a registered nurse prior to going to NP school, most of my colleagues who have recently entered the field have two or fewer years in practice before starting their NP program. Boiling those hours into years of post-bachelor’s training using data on the quickest paths around — physician=7, PA=2, NP=2.
Keeping that all in mind, we can turn back to the question. What is the shortest time we could train someone to work as a primary care provider? It all depends on what we want them to do. If we want them to be able to find the zebras hiding among the horses (which is how medical school professors like to describe rare diseases) we probably need people with more education. If we want people to follow algorithms and guidelines and crank out referrals and orders, we can use resources with less education.
I think there is room to streamline the path for physician trainees, or at least to allow them to focus on the areas where they might want to dig deeper. For example, I knew early on in my training that I would not be practicing in a rural area and would not be delivering maternity care. Still, I had to complete multiple months of required labor and delivery rotations that could have been better spent learning geriatrics or weight management. I also spent several months staffing the intensive care unit even though I knew that I would be moving to an area that doesn’t allow family physicians to have ICU privileges.
Mr. H asked whether med school should be more training than education given the endless access to literature and resources. I think med schools have evolved over the last decade. I have watched my alma mater make significant changes to its curriculum. For example, they’ve shifted clinical education so that it starts almost on Day One.
For people who are committed to a career path, it could be streamlined a bit, but sometimes physicians don’t find their calling until their third or fourth year of medical school. My own school penalized me for wanting me to do family medicine from the get-go, but that’s another story. As someone who chose a path to deliver comprehensive care, though, I can only think of one clinical rotation in medical school that didn’t contribute to my future specialty-specific knowledge, although it taught me an unquantifiable amount in the realm of delivering compassionate care.
Mr. H also asked how much of a mid-career PCP’s practice uses their training from decades before. I’d say that 20 years out, my family physician colleagues in traditional practice are using a fair amount of their original training, minus the obstetrics, general surgery, ICU, and some of the emergency medicine procedural skills. They’ve also learned a considerable amount as medicine has changed. For example, many of the drugs used to treat diabetes today didn’t exist when I was in medical school. For me in the emergency and urgent care space, on a routine basis, I use about 70% of my training, but when something comes in that falls into the other 30%, I’m glad I have it deep in the recesses of my brain.
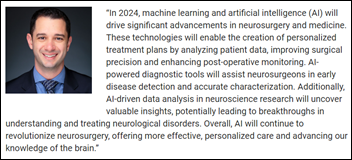
Mr. H asked whether some things can be eliminated because they’ll become obsolete, and I think that’s tricky because it’s hard to predict what exactly will be obsolete. For example, we’re still treating strep throat the same way we did 20 years ago, but not diabetes.
As a seasoned attending physician who formerly precepted students and residents, I’ve seen what can happen when less-trained individuals see patients. During the training period, however, there’s the opportunity for supervisors to educate and correct these situations. When less-trained individuals are out in practice unsupervised, regardless of their degree, there’s no process for correction until the patient sees another provider or something bad happens. There is a growing body of literature that demonstrates that less-trained individuals order more referrals, which leads to more expensive care, not to mention delays in patient care and poor patient experience.
Because of that, and what I’ve seen in practice, I personally don’t believe that less training or less education is what we need. Instead, I think we need to be using the resources we have more effectively. How do we do that, you may ask?
First and foremost, unshackle the highest-trained providers (the physicians) from the work that others with less training can do. Free them from their inboxes and hire adequate staff to support them. Use highly trained support staff to manage messages and triage patients using protocols and standing orders. Put registered nurses back on the team, not just medical assistants or patient care technicians.
Second, embrace team-based care. Bring nurse practitioners and physician assistants into specific roles. For example, seeing complex diabetic patients monthly for ongoing education and fine-tuning of treatments while the physician sees them quarterly. That way, the patient can benefit from both levels of education. Encourage patients to build relationships with the team so that there’s a larger pool of people that know them and can watch for changes in their status.
Third, bring in ancillary disciplines for support – registered dieticians, clinical pharmacists, certified diabetic educators, psychologists, social workers, care coordinators, health coaches, patient navigators, and more. Those disciplines have different education than primary care providers and can help deliver more focused interventions so that others can work at an appropriate level commensurate with their training and education.
Finally, I’m going to go out on a limb and mention the rise in the number of for-profit schools as contributing to the problem. For some of them, the focus seems to be on cranking out graduates rather than producing well-educated, well-qualified graduates. As an example, the local medical schools and PA programs (which are affiliated with comprehensive universities) all provide students with lists of “approved” preceptors for rotations. They are vetted and provide documentation about their teaching style and what they’ll allow students to do. The for-profit NP program in the area (which is not affiliated with a comprehensive university) allows students to select their own preceptors, and the students have to call around and beg people to allow them to rotate. I get two or three calls a month. I can’t imagine there’s much quality control over what some of those preceptors may or may not be teaching and the process seems predatory given how much tuition the students are paying.
To make a long blog short, I think there are some ways we can streamline training programs in the US, but we still need some primary care providers to have longer, more comprehensive educational experiences. By using those with shorter training programs or those that have a narrower focus alongside those with broader training, along with other ancillary professionals, we can provide not only the best care for patients, but also the most cost-efficient care with the best outcomes. I would be remiss if I didn’t mention the biggest barrier to people becoming primary care physicians, which is that they are among the lowest-paid specialties.
What do you want in a primary care provider? Or do you just want to get your care from Amazon? Leave a comment or email me.

Email Dr. Jayne.































I've figured it out. At first I was confused but now all is clear. You see, we ARE running the…