Jason Rose is CEO of Clearsense.

Tell me about yourself and the company.
I’m Jason Rose, the CEO of Clearsense. I’ve been here about a year. I’ve got 30 years in healthcare technology. The first half of that was on the healthcare technology side of provider, working at companies like Cerner, Ernst & Young, and Ardent Health Services. In the last 15 years or so, I’ve been mainly on the payer side, focusing on value-based care and providing tools to clinicians to advance outcomes. Inovalon and Adhere Health are a couple of those companies.
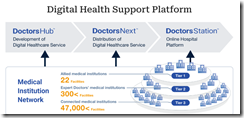
I’m excited to be with Clearsense. We are a data-enabling platform company that focuses on supporting health systems to revitalize their data for other use cases, such as reducing costs in areas such as application decommissioning, or advancing other areas of innovation, such as healthcare data lakes, clinical trials, research, and AI validation.
Who do you see as your competitors and how are you different?
Because we’re a broad data-enabled platform company, our modules have different areas of competition.
When we’re talking about application decommissioning — we’re more commonly using the term active archiving — we are competing with companies that operate in that space as a SaaS organization. We don’t compete with companies that do, let’s say, application rationalization. In fact, we partner with companies, consulting groups, that do application rationalization or that put in governance programs so that we can exploit the value proposition to scale the decommissioning of applications that are mired in most health systems of today due to all the mergers, acquisitions, and enterprise rollouts of EHRs and ERP systems.
We’re on KLAS. We have fantastic ratings. We are on record as the largest decommissioning project ever, per KLAS. You’ll hopefully be seeing some news on that in the coming days with respect to this massive installation of literally hundreds and hundreds of different applications and several tens of millions of dollars in cost takeout.
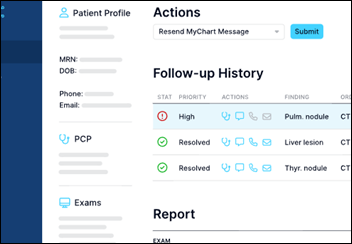
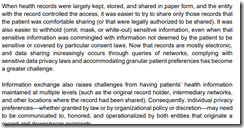
On the data lakehouse side, we will compete with middleware companies that are taking data in from primary sources, EHR companies such Epic, Cerner, and Allscripts. Think about archiving, systems that are shut down or systems that have been around for 20 years or longer. We’re pulling in longitudinal data and as near real-time data as the client wants. We’re certifying that the data is exactly accurate to the data source. We certify it with DAV, Data Aggregator Validation, which is an NCQA certification program that matches the data we got from the primary source, whatever EHR system, with our new data lakehouse to make sure it is identical and complete.
We are taking in multiple EHR instances across the entire health system. In some cases, it could be dozen or dozens of instances that we are patient matching across the entire enterprise. When the client wants to bring their own technology, such as their own AI methodology, proprietary tools, data visualizations, or different types of areas of LLM, they can do that on top of our data enablement platform. We are enabling them to do all those things in rapid fashion.
Some people might see decommissioning as just converting whatever data you can to the new system and then leaving the old system running somewhere just in case. What expertise is needed to do it right?
We are, I would say, the expert’s expert in doing this at massive scale. Health systems are commonly doing mergers, acquisitions, rolling out EHRs and ERP, or trying to improve their cybersecurity posture. All of those are critically important today.
The reality is that in the application portfolios of these systems, they have done the app wrap programs with lots of consulting firms over time. What they haven’t done is look at how to do this at massive scale across all the different areas. Having the SaaS program that we deploy, the consulting, and the expertise, we put together governance programs that are partnered with the executive leadership of the health systems.
These are not IT projects, these are business projects. This is going to include not just technology, but also clinical, HIM, finance, procurement, the legal team, and the operational areas of the health system to take the applications from the app wrap program and prioritize — with everyone putting their hand on the stone, so to speak – to say, we’re going to decommission these dozens, hundreds, or in some cases, thousands of applications.
Most of these health systems have 20 to 30% bloatedness, that’s the term, in their portfolio. The massive amount of cost takeout and cyber improvement is huge if you are deploying it in the right way. Cross-departmental as a business problem, as a cost takeout, and cyber improvement, but it needs to be multi-departmental. It’s not something to take lightly.
It really is a company mission, and our best examples where we have done this really well was where it was a mandate from the top down that said, “We’re going to do this as a health system and make it a priority so that we can reduce our operating costs. These are hard numbers. We can improve our cyber posture.To realize the benefits that the EHR system represents, to represent the ERP system enterprise value, or the M&A transaction.”
This is all about acceleration to value. We see ourselves as the pioneer in this advancement.
Do increased cybersecurity concerns bring in clients who need help, but who also want to know more about how you will protect their data?
A lot of these systems that need to be decommissioned may not even be supported by the vendor at this point. Or they could be homegrown, which is even worse. Issues such as cyber threats are at the top of the list. Some people call them zombie apps. These are the easier ones, you know, but they are still there.
Once decommissioned, the data is processed and stored securely in our HITRUST- and SOC 2-certified cloud environment. The data is immediately placed in a safe and secure environment because of the nature of where it came from and where it’s going.
Does AI create new business opportunity?
I’ve historically been skeptical of any new acronyms that have come out in our healthcare industry. There has been so much hype around the next big thing, and then it fizzles out. Healthcare is just different from other industries. We’re much, much slower to adopt, for lots of good reasons and lots of bad reasons, too.
But I will say, and this is literally the only time my career that I have said this, that I think AI is legit. I did not say that about blockchain, big data processing, or all these other things that have happened over the last 20 or 30 years. I’ll even go Y2K. But I think AI is legit.
As a company, we are looking at how to apply AI to writing code more efficiently, processing data faster, and ingesting data differently. We are exploring different areas of how AI can help make us more internally efficient so that we can drive value acceleration, which is what our brand is all about.
But on the flip side, we’re a data enablement platform company, so we look at AI as an opportunity to add a value proposition in things such as enabling our clients to incorporate their AI onto our data platform. For example, we have a significantly large health system that we’re in the midst of bringing live. We have millions and millions of members that are across a dozen or so EHR instances. It’s longitudinal back to 20 years and up to three days ago. It has completeness, timeliness, and the data is certified.
The client is putting their own AI tools and their own proprietary tools on top of our data platform so that they can run their own algorithms and test other technologies and initiatives that they want to do, both within their health systems and also across their their other ventures. It is helping them advance in a rapid, scalable way to be free to explore and create their own mission. We are the enablement aspect of that.
As someone who has been in health tech for a long time, how do you see today’s environment and how it might change in the short term?
I’m going to quote Stephanie Davis, who is a Barclays analyst, from something she said last year. We have the ViVE conference coming up here in Nashville, which is our new corporate headquarters for Clearsense, but at last year’s LA ViVE conference, a question from the audience asked Stephanie, “What are your thoughts on AI, and how many of the companies on the floor of ViVE you think will exist in two or three years?” Her response was astounding, interesting, and I agree with it. I think that it will be a single percentage left in years to come.
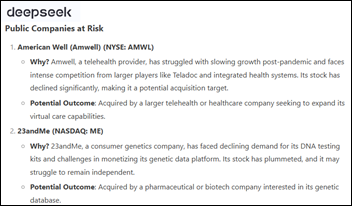
You will have all these different AI companies that are hyper competitive with each other, and only a very few of them will actually exist in years to come. There’s a lot of hype around companies that claim to be the next big thing on AI versus the commodity of AI, AI itself. There will be a lot of churn in areas. We are not trying to be the AI company. We’re trying to be the enablement of AI. I predict that we’re going to see a downfall of a lot of hype and investment in these AI companies, because they’re going to eat each other.
The other prediction, and this is sort of Captain Obvious, is that if you’re not focusing on your clients’ value proposition as your core mission, you will have a hard time succeeding in today’s environment. It’s no longer where private equity and venture capital will support hype. They need growth, profitability, and sustainability. These companies that are just built on hype won’t exist. You have to have real tangible value that you can point to. Not actuarial madness, but actual hard dollars that your clients will tout, including the CFO of those companies, to say that this is actually a tangible ROI that I received out of this company. Without that, a company is in trouble in this hectic time.
How has the health tech business climate changed in Nashville?
This is the second time that I have moved to Nashville. The first time was back in 2002, when it was the country’s best-kept secret. Now the secret is out and is no longer a secret.
A lot of people consider Nashville to be the healthcare tech capital of the country. A lot of people consider that the Silicon Valley of healthcare technology is in Nashville. If you look at the core of this environment, almost all, if not all, of the large for-profit health systems are headquartered here in Nashville. The most dominant industry in Nashville and greater Nashville is healthcare. Because of that, there are dozens if not hundreds of companies that are focusing on innovation in healthcare and driving healthcare technology strategies. Companies like HCA, which is the largest health system in the United States, Ardent, Lifepoint, Community Health Systems, and all those large companies.
Because of that massive amount of economy here – I think it’s around $100 billion coming out of Nashville alone, which is just a fraction of the valuation of those companies — this is the nucleus of the country. That’s why ViVE is coming here every other year, and that’s why it’s gotten so much accolades. Oracle about a year ago announced that they are relocating their entire corporate headquarters to Nashville and they are in the midst of doing that right now, downtown next to the new multi-billion dollar Titans stadium. Amazon announced years ago that their eastern service excellence headquarters moved here as well.
This is a big tech hotspot now, and also healthcare is dominant. We’re happy to come back here and I wasn’t moving, so it was easy for me to make that choice. It was from a company standpoint and the fact that I love this town and the culture. If you’ve never been to Nashville, it’s an awesome town. They call it Nash Vegas for a reason. It’s one of the best places to go in the country, with food and entertainment, and is very rich in healthcare as well.
What excites you most about the next five to 10 years in healthcare?
I go really way back. I got a graduate degree from the George Washington University School of Business. When I went there in the mid 1990s, there was no healthcare tech program. That didn’t exist. I was asked to choose a discipline of focus in my Master’s of Health Services Administration degree. I said, I want to do technology. They said, that doesn’t exist. No one’s doing that. It’s either acute care or regulatory compliance. I said, no, I want to do healthcare tech, so they allowed me to create my own custom degree. I’m actually the first graduate intern at Cerner Corporation. I may be the only graduate intern, but I was the first graduate intern for sure [laughs]. That set forth the last 30 years of where I am today.
What I am most excited about goes back to where I was in the 1990s, where I saw the promise of technology, data, and analytics advancing healthcare in helping drive us to better healthcare outcomes, higher quality and healthier lives, and increased efficiency and reduced cost in healthcare delivery. I have about equal parts of a provider and payer experience with a dabbling of life sciences, so I’ve got a pretty broad spectrum of my foundation of experience. I have never been more excited than right now about where we’re headed over the next five or 10 years.
AI is definitely a big part of it, but not the only part of it. I could not be more excited about where we’re headed because of the massive adoption we’re finally doing in health care tech. I think it’s real this time.
Comments Off on HIStalk Interviews Jason Rose, CEO, Clearsense








































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…