News 1/29/25
Top News
AI-powered cancer drug discovery startup Manas AI launches with a $25 million seed funding round.
The co-founders are LinkedIn co-founder and venture capitalist Reid Hoffman and oncologist-author Siddhartha Mukherjee, DPhil, MD, who wrote Pulitzer non-fiction winner “The Emperor of All Maladies: A Biography of Cancer.”
Reader Comments
From Steve: “Re: impact of DC happenings on healthcare, Are you planning to cover it, or would you rather dodge the politics of it? I think your readers would be interested.” I will cover any significant health tech-related change in law, regulation, or standard that affects the industry once it has happened. Coverage of legislative sausage-making isn’t my long suit and is amply covered elsewhere.
Sponsored Events and Resources
Instant Access Webinar: “Healthcare Data Security: Aligning Processes with Evolving Threats & Regulations.” Sponsor: Inovalon. Presenters: Anthony Houston, MBA, senior director of security, risk, and compliance, Inovalon; Paul Wilder, MBA, executive director, CommonWell Health Alliance; Luke McNamara, MPA, deputy chief analyst, Google Cloud; Michael Quinn, VP of strategic partner development, Inovalon. Hear leaders in healthcare data security discuss some of the top recent threat evolutions and how organizations can proactively respond by making ongoing improvements to security protocols.
Instant Access Webinar: “Successfully Navigating Post-Acute Rev Cycle Challenges.” Sponsors: Inovalon and KanTime. Presenters: David Swenson, senior manager of sales engineering, Inovalon; Lucy Lopez, VP of product management, KanTime. Learn how to speed up your revenue cycle processes and avoid the common RCM and eligibility errors that cause delays and denials. Discover strategies to boost your bottom line: streamline eligibility verification, simplify complex processes, and optimize denial management for improved cash flow.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
Therapy-focused health IT vendor Raintree Systems acquires Yoomi Health, which specializes in digital tools and practice management software for physical therapy.

The Wall Street Journal reports that a potential take-private deal between Walgreens and private equity firm Sycamore Partners, which was first reported in early December, is no longer on the table. Shares of the retail pharmacy dropped on the news, further escalating the stock’s see-sawing as Walgreens investors react to a DoJ lawsuit and better-than-expected quarterly earnings. WBA shares have lost 52% in the past 12 months.
Delfina, which offers an AI-driven pregnancy care platform, raises $17 million in a Series A funding round. Founder and CEO Senan Ebrahim, MD, PhD previously founded and ran Hikma Health, which offers free and open source software for caring for refugee patients.

Equality AI CEO Maia Hightower, MD, MPH, MBA announces that the company, which focused on trustworthy AI in healthcare, has closed after four years. She says that AI standards adoption will be delayed now that the White House has cancelled a 2023 executive order that addressed trustworthy development. She previously held IT leadership roles at University of Iowa Health Care and University of Utah Health and was EVP/chief digital and transformation officer at UChicago Medicine through July 2023.
Sales
- Hartford HealthCare (CT) selects WellStack’s analytics and data integration capabilities.
People


Adam Kansler, JD (S&P Global) will become CEO of Inovalon upon the March 1 retirement of company founder and CEO Keith Dunleavy, MD.

HealtheConnections promotes Elizabeth Amato, MHA to president and CEO.

Linda Janiszewski (UCSF Medical Center) joins CTG as IT strategy and value solutions leader, healthcare.
Announcements and Implementations
The development team that is behind the Opal patient portal for Canada’s McGill University Health Centre shuts down the app due to funding shortfalls, leaving 7,000 patients without access. Opal was developed as a non-commercial alternative to MyChart, part of Quebec’s $2 billion Epic implementation. The seven-year-old app, which was built with a $7 million innovation grant, required $350,000 annually to operate. The hospital stated that Opal failed to meet its expectations as a stable clinical solution and declined to provide further funding.
Duke Health and UNC Health will build North Carolina Children’s, the state’s first standalone children’s hospital. The 500-bed facility, which is expected to cost $2 billion, will receive $320 million in state funding. Groundbreaking is scheduled for 2027, with the hospital opening in the early 2030s and full campus completion by 2033.

Tampa General Hospital (FL) funds the rollout of OnMed’s “clinic in a box” – which offers real-time virtual visits – at a homeless shelter. The station includes diagnostic tools and thermal imaging cameras. I wrote this in October 2019 when TGH installed one of the units in its employee cafeteria:
Even odder: Tampa General Hospital opens an OnMed telemedicine consult and drug dispensing booth in its food court so that its employees — who are inside its walls — can seek medical care from clinicians who aren’t. Maybe this is a Halloween-appropriate “the call is coming from inside the house” type situation. It’s not really an admission that employees don’t have time to deal with their own hospital employer’s bureaucracy as patients – the hospital is in business with the vendor and this first booth is a pilot for a broader rollout. The hospital CEO says millennials won’t wait to see a doctor in person, which if you’re a doctor who actually wants to care for patients, is depressingly accurate. The oldest millennials are now in their late 30s, so it would be interesting to see how those who are doctors run their practices and patient encounters.
Other
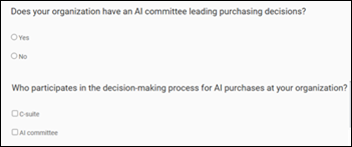
The CEO of non-profit Peterson Health Technology Institute, which evaluates digital health technologies using evidence-based assessments, tells Politico why the organization is launching yet another AI task force that involves big health systems. CEO Carolyn Pearson says:
We are not working with the AI evangelists or the AI researchers. It’s a CFO saying: “When I spend X, Y, Z, how is productivity changing in my environment? Or if I’m not pushing productivity changes and I’m doing it for the provider’s well-being and to prevent turnover — how am I measuring that?” A lot of them want to roll out AI medical scribes because it’s good for providers and helps with the long-term sustainability of that job. But as the solutions are coming into their systems, they are very quickly spreading out into cycle management, staffing, prior authorization and a million other service lines these companies offer. If you’re a health system leader and not being very careful and thoughtful about what you are and are not adopting, you can find yourself with big solution costs very quickly.

UMass Memorial Health creates a Digital Hub to unify its patient flow, remote patient monitoring, and in-home care management services. The e-ICU, part of the health system’s RPM division, monitors 150 ICU beds across facilities, with staff members responsible for up to six patients each.
Children’s Hospital of Philadelphia develops the Clinical Outcomes Data Archive, incorporating EHR data and manually collected and clinically reviewed data, to improve early interventions, care plans, and pregnancy-related outcomes research within its fetal medicine department.
Sponsor Updates
- Black Book Research publishes a new report, “Innovation for Equity: The Transformative Role of DEI in Healthcare IT Success.”
- AdvancedMD releases “CPT/HCPCS Codes Guide 2025,” a comprehensive resource for ambulatory care providers listing the latest medical billing code updates.
- AGS Health will exhibit at the HFMA Lone Star Winter Conference January 30-31 in Irving, TX.
- Ascom Americas welcomes new project manager Casandra Siefkes.
- Capital Rx releases a new episode of The Astonishing Healthcare Podcast, “Why Drug Prices & Modern Tech Matter in Hospice Care, Too, with Nick Opalich.”
- Clinical Architecture invites healthcare professionals to participate in its 2025 Healthcare Data Quality Survey.
Blog Posts
- Meaningful AI in Post-Acute: Elevating Care and Efficiency with Integrated AI (Netsmart)
- Proposed Changes to the HIPAA Security Rule (AdvancedMD)
- AGFA HealthCare at HIMSS 2025: Revolutionizing Enterprise Imaging with Innovation and Work-Life Balance (Agfa HealthCare)
- Six realities facing CIOs—and a complimentary report on navigating them (Altera Digital Health)
- A CIO’s Advice for Moving All-Digital Hospital to Epic EHR (CereCore)
- Ensuring successful EHR implementations: A holistic approach to people, data, and technology (Cardamom Health)
- OCR’s Proposed HIPAA Security Rule Notice of Proposed Rulemaking Part 1: Overview, Key Takeaways and New Terms Defined (Clearwater)
- EHRs as Engines of Insight (CliniComp)
- CloudWave’s Predictions for Healthcare IT in 2025 Part 4: Broader Adoption of Targeted Use Cases for Healthcare AI (CloudWave)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Contact us.



































"The US Immigration and Customs Enforcement (ICE) posts an anticipated future contracting opportunity for a correctional EHR for ICE detainees,…