Monday Morning Update 3/24/25
Top News
Google Chief Health Officer Karen DeSalvo, MD, MPH, MSc announces six health AI updates at the company’s annual healthcare conference:
- Enhanced the AI overview capabilities of health searches, including “What People Suggest,” which can “organize different perspectives from online discussions” into themes.
- Provided API access to Health Connect, the company’s Android-based health and fitness data sharing platform.
- Rolled out loss of pulse detection, an FDA-cleared Pixel Watch 3 feature that automatically calls emergency services if the wearer’s heart stops.
- Released an AI co-scientist for Gemini 2.0 that can help design clinical studies by reviewing existing research and proposing testable hypotheses.
- Released open, Gemma-based models to enhance AI-powered drug discovery.
- Worked with a hospital in the Netherlands to support personalized pediatric cancer treatments by applying knowledge from medical publications to individual patients.
Reader Comments
From RM: “Re: NIMs. Nvidia Inference Microservices are now available on Microsoft Azure AI Foundry. These are essentially optimized containers for two dozen foundation models, allowing developers to deploy generative AI applications and agents quickly. Epic is planning to be an early adopter.” The Microsoft blog post quotes Epic VP Drew McCombs as saying that it will use Azure AI Foundry and is working with UW Health and UCSD Health to evaluate clinical summaries using advanced models. Epic gains several advantages from using a direct infrastructure pipeline for AI model deployment:
- Standard APIs make it easier to integrate models into workflows with contextual awareness.
- Customer deployment of models is easier.
- Health systems can fine-tune models locally.
- Epic gains competitive advantage in using advanced technology and applying it to key integration points such as Best Practice Advisories.
From Piazza: “Re: VA. How will they hire contractors to support ramped-up go lives when the federal government is cutting contracts? Who would take those jobs, especially if start and end dates are soft?” That will be one of the VA’s many challenges. It might have been easier had the VA followed the DoD’s lead in choosing a government-entrenched company like Leidos as the prime contractor with Cerner as the subcontractor rather than allowing Cerner to be its own prime.
HIStalk Announcements and Requests
Last call for provider-side IT leaders to join my Executive Watercooler panel, whose participants will get a monthly “what do you think about this” email and send me their brief thoughts.
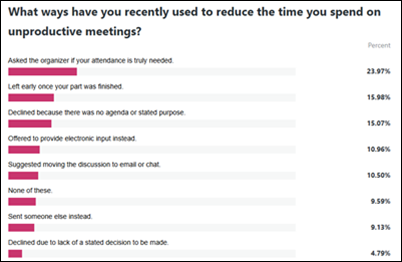
Poll respondents list several ways they reduce their time spent in unproductive meetings.
New poll to your right or here: How has your employer’s support for work-life balance changed in the past two years?
Sponsored Events and Resources
Live Webinar: March 27 (Thursday) noon ET. “How to Improve Clinical Workflows with AI Chart Summaries and Risk Predictions.” Sponsor: Health Data Analytics Institute. Presenters: Scott Cullen, MD, senior advisor, Health Data Analytics Institute; David Clain, chief product officer, Health Data Analytics Institute. Learn how the EHR-embedded HDAIAssist tool is transforming the ability of clinicians to pull insights out the mountains of data that have accumulated in the EHR, quickly, accurately, and cost-effectively. HDAlAssist, which is part of HealthVision, the intelligent health management system, combines AI chart summaries and granular risk predictions to quickly inform care planning decisions, especially for the most complex, high-risk patients.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
Canada-based virtual healthcare kiosk manufacturer UniDoc Health acquires most of the assets of telemedicine hardware and software vendor AMD Telemedicine for $175,000. The Massachusetts-based AMD’s Agnes Connect software platform captures and shares real-time medical device data its live videoconferencing module.
People

Jett Reidy, MBA (EnableComp) joins Collabrios Health as CTO.
Sponsor Updates
- Findhelp powers seamless closed-loop referrals and data exchange under CalAIM’s CLR and HRSN requirements.
- Nordic releases a new episode of its “Designing for Health” podcast titled “Interview with Spencer Dorn, MD.”
- Surescripts releases a new episode of “The Dish on Health IT” podcast titled “What Challenges, Opportunities and Urgency Face Pharmacy Interoperability Today?”
- TeamBuilder will exhibit at the AMGA conference March 26-29 in Grapevine, TX.
- Tegria will present the The Beryl Institute’s Elevate PX conference April 1 in Las Vegas.
- WellSky will exhibit at the NHIA conference March 29-April 2 in National Harbor, MD.
Blog Posts
- The HIM Director’s Guide to Autonomous Medical Coding (Nym)
- Better Outcomes, Lower Costs and Reduced Downtime Through AWS’ Independent Recovery Environment for Epic (Prominence Advisors)
- Connected Healthcare Summit Day One: A Vision for the Future (RLDatix)
- HIMSS25 & ViVE 2025 Highlights: Key Innovations Transforming Healthcare (TrustCommerce, a Sphere Company)
- Reflecting on ViVE 2025: Healthcare’s Next Big Leap (Symplr)
- Medical librarians can help evaluate AI-enhanced decision support (Wolters Kluwer Health)
- Where to Begin: Unlocking the Value of Automation in IT Service Desk Management (CereCore)
- Powerful AI: Examining results of Waystar AltitudeCreate in RCM (Waystar)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Contact us.























The New Yorker cartoon of Readers Write articles.