News 6/27/25
Top News
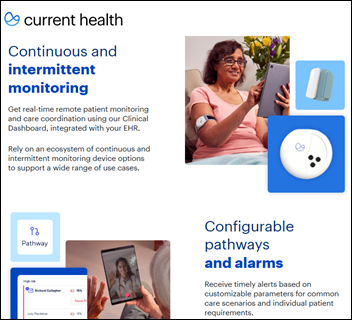
Best Buy sells remote patient monitoring technology company Current Health back to its co-founder and CEO Christopher McGhee (formerly known as Christopher McCann).
Best Buy acquired the company in October 2021 for $400 million and has struggled with its in-home healthcare business since, including taking two write-downs totaling nearly $600 million this year.
McGhee left Best Buy in March 2024. I interviewed him in April 2022. Several former Current executives will return to the company with him.
Best Buy’s CEO said in its most recent earnings call that hospital-at-home solutions business was advancing more slowly than it had expected.
Reader Comments
From Blew Button: “Re: AI strategy. Everyone is pushing for faster adoption. How are health systems balancing that with validation, integration, and project priorities? We can’t skip the hard parts just because execs and the board are believing the AI hype.”
HIStalk Announcements and Requests
Microsoft’s retirement of Skype pushed me to use Teams instead for my weekly English sessions with my Ukrainian student. Teams has been unreliable, slow, and maddening (why can’t I test my camera and microphone without connecting to a meeting?) Teams repeatedly froze the connection this week, so we tried WhatsApp, which had better quality and reliability for at least those few minutes. I will confirm next week after we try our full-hour session on WhatsApp.
Sponsored Events and Resources
None scheduled soon. Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
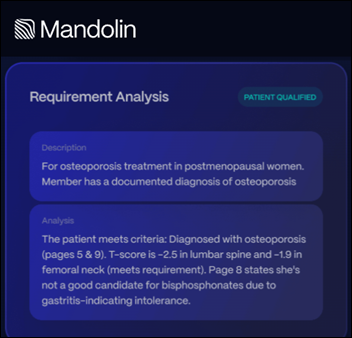
Mandolin, which uses AI agents to manage specialty drug intake, benefits, prior authorizations, and RCM, raises $40 million in seed and Series A funding.

Veradigm reaffirms its intention to have its shares relisted in 2026. The company said in its earnings call that it is gaining new provider business in specialty practices, value-based care, and especially in revenue cycle. Revenue is flat as the company expected, however, and it continues to see attrition among larger clients.
Provider data management vendor Certify raises $40 million in a Series B funding round. Founder and CEO Anshul Rathi, MS started the company in 2021 after managing network data for Oscar Health.

Arine, which offers an AI-powered medication optimization platform, raises $30 million in a Series C funding round. CEO Yoona Kim, PharmD, PhD worked in pharma and at Proteus Digital Health before she co-founded the company in 2017.
People

Evidently hires Chris Cowart (Xsolis) as head of growth.

Tony Murdoch (Bamboo Health) joins Zus Health as VP of business development and partnerships.
Announcements and Implementations
Altera Digital Health launches Sunrise CarePath, a mobile patient engagement platform that is integrated with its Sunrise EHR. It offers secure messaging, self-scheduling, patient notifications and appointment reminders, and billing integration.
Researchers describe ECGFounder, an ECG foundation model that was trained on 11 million ECGs and their cardiologist notations. They theorize that its expert-level diagnostic performance could provide useful in analyzing ECG data from wearables.

KLAS surveys C-level health system executives about their technology vendor expectations. Recommendations to companies:
- CEO: address big-picture value of the platform; back up claims with real-world metrics from other health systems; be prepared to pitch at a board level.
- CFO: provide contracting transparency; be flexible in negotiations; show line-item cost implications; partner to perform post-implementation financial impact reviews.
- CDO: provide integration playbooks; provide change management toolkits; partner in developing data governance frameworks.
- CIO: address how the solution fits into the broad IT strategy; provide proactive support from implementation through optimization; partner on rationalizing legacy technology and vendor sprawl.
- CISO: provide risk documentation and real-world threat models; provide easily deployed security tools; include advisory services in the engagement model.
- COO: provide turnkey dashboards that integrate operations, finance, and quality; provide industry benchmarks and advisory services; provide quick-win use cases and tactical automation.
- CTO: provide architecture diagrams, threat models, and deployment recipes; include stakeholders in roadmap previews, especially when dependencies or APIs will change; share reference implementations and provide a sandbox to prove extensibility claims.
- CMO/CMIO: involve them in roadmap development; showcase measured clinical outcomes and provider satisfaction benchmarks; provide tools to help build consensus with clinical leaders.
- CNO/CNIO: shadow nurses to map workflows; provide real-time, around-the-clock support; get nurses involved in roadmap designs using clinical councils or pilots.
Government and Politics
Digital health companies Whoop, CoachCare, and Epic testify before the House Ways and Means health subcommittee about the benefits of wearables and remote patient monitoring. Their timing was ideal given HHS Secretary Robert F. Kennedy, Jr.’s recent call for every American to wear a device within four years, but less so given lawmakers’ focus on a proposed reconciliation bill that would strip coverage from 16 million people through Medicaid and ACA coverage cuts.
Privacy and Security
King’s College Hospital NHS Foundation Trust tells a patient’s family that a cyberattack contributed to his death. Pathology provider Synnovis was hit by a ransomware attack on June 3, delaying the patient’s critical test result.
Other
Microsoft profiles how 365 Copilot is used by the chief digital officer of a hospital in Brazil. He says it helped him improve his no-nonsense email style to be more polite and “really cute.” He adds that it has reduced his email management time by 70% and allows quicker decision-making by summarizing long email threads.
Sponsor Updates
- An unnamed Southern health system selects Vyne Medical’s Trace Platform to process inbound orders in its patient access department.
- Black Book Research poll-takers name the leading EHR-native patient accounting systems for 2025, including HIStalk sponsors Meditech and TruBridge.
- CereCore earns a five-star rating and “Best Practice” designation as an Infrastructure as a Service provider by Securance Consulting.
- Findhelp welcomes new customers City of Kansas City, MO; DSR Public Health Foundation; and Careforth.
- Five9 releases a new customer success book titled “Aeroflow Health Improves Efficiency with Automation.”
- Healthcare IT Leaders releases a new “Leader to Leader” podcast episode titled “From Technical Debt to Transformation: The Cloud Journey Healthcare Needs.”
- Meditech releases a new customer success story titled “Sierra View Medical Center Unleashes the Power of Data with Meditech’s Analytics Solution.”
Blog Posts
- How We Did IT: Oracle Health EHR Speed & Reliability Score Increased 17% (Goliath Technologies)
- Recent Enforcement in Healthcare Price Transparency: What You Need to Know (FinThrive)
- How Managed XDR Strengthened Cyber Defense at a Vermont Hospital (Fortified Health Security)
- Simplifying chronic care: What you need to know about APCM codes and MIPS MVP reporting (Healthmonix)
- 5 Strategies to Build a Motivated Healthcare Workforce (Inovalon)
- Advancing Data Integrity: DAV Cohort 10 Reflects KONZA’s Continued Leadership (Konza)
- How Orthopedic Practices Are Streamlining Patient Disability and FMLA Form Management with MRO (MRO)
- 5 key takeaways from our VBC initiatives roundtable (Navina)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Sponsorship information.
Contact us.

























The New Yorker cartoon of Readers Write articles.