Top News
The UK government enlists the help of healthcare and consumer technology companies to address the coronavirus pandemic.
Companies in attendance at a high-level meeting include Babylon (symptom checking chatbot) and Thriva (at-home blood tests).
Startups that have reported surges in demand for their products there include Nye (secure doctor-patient message via telephone and video), Patchwork (matching doctors with available hospital work shifts), and Pando (WhatsApp-like teamwork and collaboration).
Reader Comments
From Mark: “Re: University of Arkansas Medical Sciences. Has a web page set up specifically for their employees on quarantine. Their concern was that their staff who test positive (and they test everyone daily!) and are quarantined, will need food, meds, and goods delivered to their houses while in quarantine. Any employee can use this. So if you are working long hours and don’t have time to shop for groceries, for example, you can visit the site and make a request. Great way to support their staff in this time of need. Kudos!” We are hopefully coming to the realization that lockdowns aside, the only way some of us will survive is if our caregivers and their families make their own sacrifices to remain on the job. We’re woefully short on ventilators, but even those aren’t worth much if we don’t have experts to run them. We have to figure out how to keep hospital employees healthy, get them back to work after exposure, and support them in ways that go beyond paying them on time.
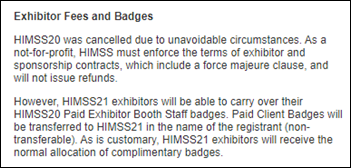
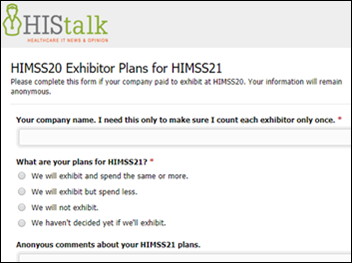
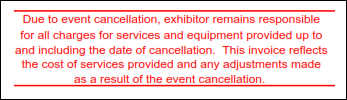
From Freeman Victim: “Re: HIMSS20 cancellation. Freeman is not refunding anything except booth disassembly. They are billing us for furniture rental through March 11 and we received an invoice today for handling the return of our booth, which was on top of the exorbitant shipping we had already paid. The original invoices didn’t spell out the policy for HIMSS cancellation, yet new ones include a policy of charging vendors full fees for services that were nod delivered. I know cancellation hurt them, but they could do a better job sharing that instead of squeezing exhibitors for every last penny in charging for services they didn’t actually deliver. I would encourage HIMSS to crack down on this, because if the event cancellation itself doesn’t cause exhibitors to question its overall value, Freeman’s handling of it will.” I assume that every cancelled conference is creating a mass of frustration and outright anger at the costs that won’t be refunded, whether simply billed anyway (Freeman) or rolled over as an unwanted credit for future services (HIMSS). It may be a tough sell for companies to sign up for HIMSS, Freeman, OnPeak, etc. all over again for next year, assuming there is a next year. The monetization of every conference moment and physical attribute has always seemed wildly excessive to me, so perhaps conferences — like other aspects of our economy and personal lives — will change positively following an unwelcome but necessary recalibration.
HIStalk Announcements and Requests
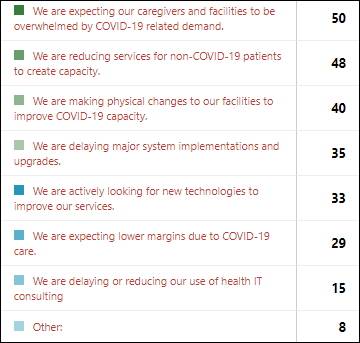
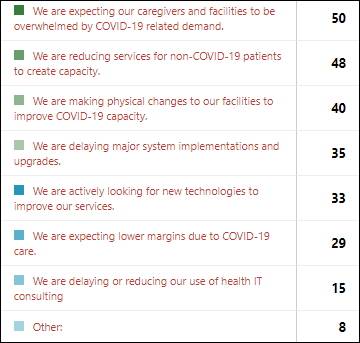
The health system employers of respondents to last week’s poll are responding to expected overwhelming demand by reducing non-COVID-19 services and making physical changes to their facilities. Those who are delaying system implementations and upgrades are matched by those who are looking for new technologies to improve their services, with use of health IT consulting not changing. Readers also say they are ramping up telehealth capabilities and searching for workforce management tools.
New poll to your right or here: Which leaders are doing a good job in responding to the COVID-19 outbreak?
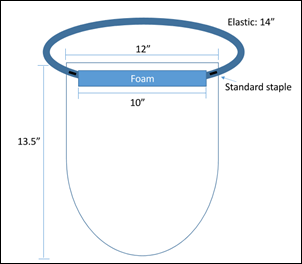
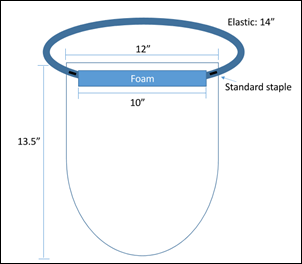
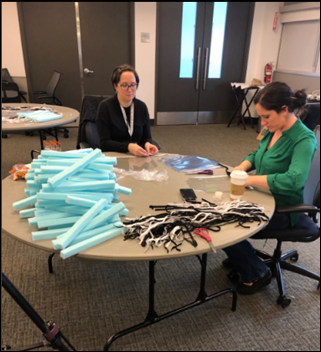
Readers asked about Providence St. Joseph Health making MacGyver-like provider face shields from components foraged from local craft and office supply stores (the need to do so, while shameful, is out of scope for this mention). Providence has published instructions for creating face shields and a video showing volunteers how to sew face masks from Providence-supplied kits.
I’m being overwhelmed with companies that want me to mention their COVID-19 related technology rollouts. I will do so if: (a) the offering is free, seems broadly useful, and has limited strings attached; and (b) it can work for everybody and not just existing users of other company products. Enhancing an existing product is of interest only to current customers, and in that case, you don’t need me to notify them on your behalf.
Listening: new from Nada Surf, one of my favorite bands of all time. They’ve been playing alternative music together as an intact unit since 1990, with an easily identifiable sound that still stays fresh with each new album. I remembered the band while creating (“curating,” as the cool kids say) a multi-hour Spotify playlist for a friend who is social distancing all alone, but is preparing for a long drive to join family. She’s younger with accordingly different musical tastes and in need of something upbeat, so I chose for her Anderson .Paak, Arlissa, Birdy, Cassie, Shakira, Hinder, Leona Lewis, Radiator Hospital, Tennis, Vargas & Lagola, Alexandra Stone, and a few of my own unrelated favorites she’s never heard such as The Hives, Juliette & The Licks, and The Tragically Hip. Her playlist sits in Spotify adjacent to my unfinished work titled “HIMSS20.”
Webinars
March 25 (Wednesday) 1 ET: “Streamlining Your Surgical Workflows for Better Financial Outcomes.” Sponsor: Intelligent Medical Objects. Presenters: David Bocanegra, RN, nurse informaticist, IMO; Alex Dawson, product manager, IMO. Health systems that struggle with coordinating operating rooms and scheduling surgeries can increase their profitability with tools that allow for optimal reimbursement. This webinar will identify practices to optimize OR workflows and provider reimbursement, discuss how changes to perioperative management of procedures can support increased profitability, and explore factors that can impede perioperative workflow practices.
March 26 (Thursday) 12:30 ET. “How to Use Automation to Reduce ‘My EHR is Slow’ Complaints.” Sponsor: Goliath Technologies. A common challenge is that a clinician is ready to work, but their technology is not. EHRs can be slow, logins not working, or printers and scanners are offline. Troubleshooting these end user tickets quickly is nearly impossible, especially in complex environments that might include Citrix or VMware Horizon. This webinar will present real-world examples of how leading health systems are using purpose-built technology with embedded automation and intelligence to proactively anticipate, troubleshoot, and prevent end user performance issue across their IT infrastructure and EHRs.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Announcements and Implementations
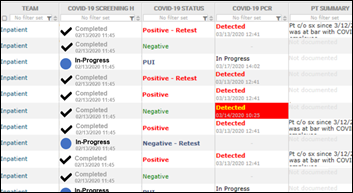
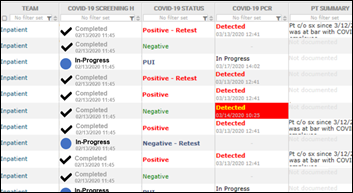
TransformativeMed offers Seattle-area hospitals free use of its COVID-19 / Core Work Manager. The product is already being used at UW Medicine, which says the application “is critical for our tracking of suspected and confirmed cases.” The Cerner-integrated app allows clinicians to track and segments lab tests and results, monitor symptom checklists, and submit information to the state health department.
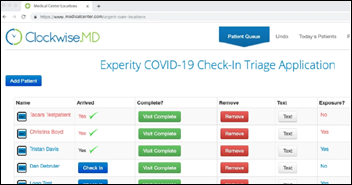
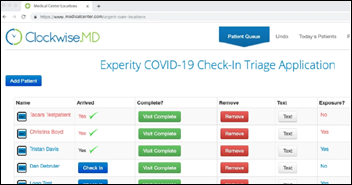
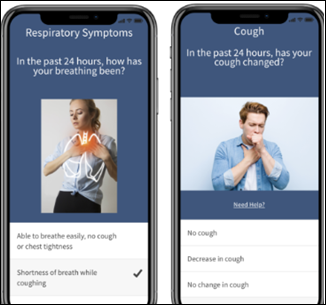
Experity offers urgent care clinics free use of its COVID-19 Check-in Triage app, which sends questions to scheduled patients via two-way messaging and then tells them how to proceed with their visit. Experity launched a year ago in merging Clockwise.MD, DocuTAP, and Practice Velocity.
Epic continues to update its “Managing Coronavirus Disease (COVID-19) with Epic” paper, which provides guidance on reporting capacity management, reporting nurse data and patient throughput, managing COVID-19 patients at an outpatient pharmacy, creating a training plan, and reporting on the outbreak for managers and leadership.
COVID-19
A reader comment spurred me to ponder whether the country’s haphazard public health reporting makes optimal use of data housed in the Epic and Cerner systems, which cover much of our bed capacity. It doesn’t matter when, where, or how COVID-19 testing was performed on individual patients – those systems track suspected and confirmed cases, they store the demographic and clinical information of patients, and they record the progression and outcome. Individual health systems are surely monitoring this information, but I don’t know if it’s being aggregated for review at the state and national level. We’re missing one significant denominator – the number of asymptomatic or previously infected people who didn’t seek medical attention from hospitals – but the trove of information otherwise is massive and complete.
Early CDC data analysis finds that COVID-19 hits younger people harder in the US than was seen in China and Italy. They also worry that a long incubation period means that seemingly healthy people are walking around spreading the virus before they know they are infected.
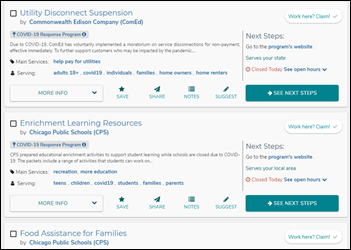
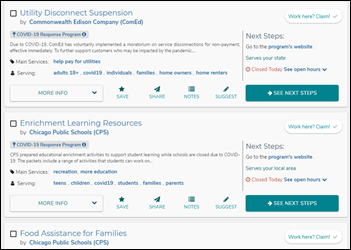
Aunt Bertha creates FindHelp.org, which allows community members to search for and connect with personally vetted social programs such as financial assistance, food, and emergency services. Hospitals can add the information to their community resource sites. The Aunt Bertha team added 700 programs in four days and is adding hundreds each day. I interviewed founder and CEO Erine Gray a few months ago and the work they do is impressive even in normal times.
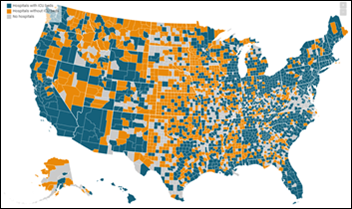
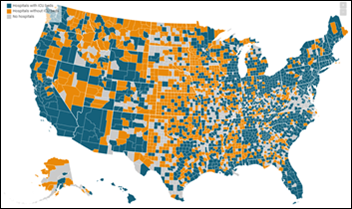
A Kaiser Health News data analysis finds that half of the counties in the US have no ICU beds, also noting that ICU beds per older resident vary widely. Experts note that hospitals with ICU beds cluster in high-income areas where patients have private health insurance. More positively, those rural counties are often located near larger cities– if you need an ICU bed, you care more about availability and distance than whether it’s in your county or someone else’s.
Cerner updates its COVID-19 response to include mandatory employee work from home through April 30 where possible, institution of an emergency pandemic time off policy, stopping all international and non-critical travel, and a 14-day quarantine at home for employees who have traveled to a high-risk location or have been in contact with someone who has.
Vice-President Pence’s statement about waiving state licensure limitations on telehealth doctors has created confusion, Politico reports, since only states can waive those restrictions, few have done so, and the federal government’s legal authority to preempt states is not clear. The Federation of State Medical Boards maintains a list of states that have waived licensure requirements in response to COVID-19, either for in-person encounters or for telemedicine. It’s still not legal for a doctor to conduct a virtual visit for a patient who is sitting in a state where the doctor isn’t licensed unless that state has waived its requirements. It would be so much easier if licensing was based on the doctor’s state rather than the patient’s.

Teledentistry provider SmileDirectClub, which sells plastic teeth aligners, will open its 3D printing facility for creating COVID-19 supplies, such as face shields and respirator valves. The company, whose 3D printing capacity is among the country’s largest in producing 20 million mouth molds per year on 49 HP Jet Fusion 3D printers, asks medical supply companies that need help and are willing to provide STL 3D printing files to get in touch.
Italy reports that nearly 800 people died and 6,500 new cases were reported Friday, with 5,000 deaths so far. Spain had 1,400 deaths and 3,800 new cases as its case growth tracks to exceed that of Italy. Doctors in hospitals in Spain are sedating patients over 65 and then removing their ventilators to free them up for younger patients. Meanwhile, CDC continues to report US cases only Monday through Friday.
New York-Presbyterian Hospital reports having 558 COVID-19 inpatients as of Sunday morning, 20% of them in ICU and many more likely bound for there.
Health departments in New York City and Lost Angeles advise doctors to skip testing people with mild respiratory infections for coronavirus unless the results would change the clinical management of those patients. The recommendation acknowledges a strategy that is shifting from containment to slowing the transmission.
In another change in how COVID-19 is viewed, scientists call for quick development of a serological test to determine whether someone has been exposed to coronavirus and has developed some level of immunity as a result. That information will help drive public health decisions since if people can develop immunity after exposure (nobody knows that yet), they could return to work, including to healthcare jobs.
Former FDA Commissioner Scott Gottlieb, MD says this about the COVID-19 current state:
- The best hope of having a therapy available by summer is antibodies. As such, bulk manufacturing should be ramped in parallel just in case something is found to work, allowing rapid rollout.
- Efforts should be focused on widespread testing (such as point-of-care testing in physician offices) and serology to help understand coronavirus epidemiology.
- We need as a nation to define the COVID-19 endpoint and develop a plan to get there rather than taking haphazard actions without federal leadership.
- The US is seeing much higher numbers of young people having confirmed cases, with 56% of New York City’s being under age 50.
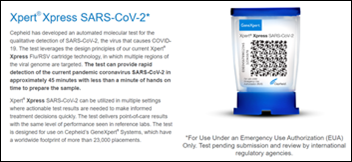
FDA gives emergency authorization for molecular diagnostics firm Cehpeid to start shipping a 45-minute coronavirus test that will run on its 23,000 GeneXpert systems, of which 5,000 are in the US and are capable of running hospital tests 24×7.
An ED doctor shares her hack for using a single ventilator to support up to four patients. She warns that such use is off-label, but also notes that anything goes in a disaster.
Just a note of who to believe on Twitter: people with expertise in data visualization, statistics, journalism, or medical practice still aren’t epidemiologists. Understanding COVID-19 from a public health perspective requires specific expertise. Choose your experts wisely and avoid the armchair kind. I also note that many non-healthcare tech folks are rushing out apps that do little to help with the coronavirus response – we have ample supplies of imitative symptom checkers and tracking maps, so please channel your talents into creating something more useful.
Privacy and Security
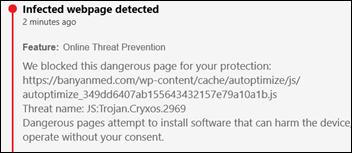
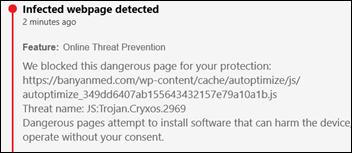
I got a press release from telemedicine technology and services vendor Banyan Medical Systems about a free hospital COVID-19 offering, but note to the company: Bitdefender says your website is ironically infected with a virus of a different kind (a cryxos trojan).
Other
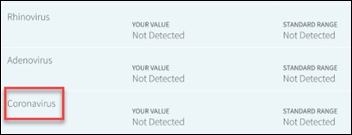
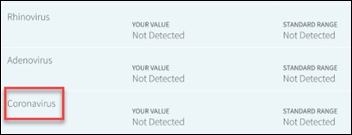
Stanford Health redesigns lab reports in its MyHealth portal after several students complained that their reports indicated a negative coronavirus test result, only to be notified soon afterward that they were positive for COVID-19. Stanford explains that the first results listed are for normal seasonal coronavirus, but the COVID-19 test takes longer and positive results then trigger a phone call from a nurse instead of immediate release of results to the portal. One of the students who was fooled is the daughter of UCLA Director of Clinical Informatics and pediatrician Paul Fu, MD, MPH, who is self-quarantining after experiencing COVID-19 symptoms. He says other health systems are reporting similar problems with patient communication, adding, “One of the things that we focus on when we put information out through patient portals is to empower our patients to become partners with us in delivering healthcare. The other thing is to help them understand what the data means, and that how we present the data is clear and unambiguous.” Paul isn’t happy that his COVID-19 exposure probably came from his daughter since Stanford didn’t cancel its Family Weekend on February 27-28 and then abruptly sent students home without self-quarantine instructions since testing wasn’t available.
Idiots with too much free time on their hands are “Zoombombing” public Zoom meeting in then blasting pornography to participants. The default Zoom setting is that any participant can share their screen. The company urges hosts of large public meetings to change the default so that only they can share their screen. It also recommends that private meetings be set to invitation-only with a password required. Users also suggest disabling “Join Before Host,” enabling “Co-Host” to allow others to moderate, disabling “File Transfer,” and disabling “Allow Removed Participants to Rejoin.”
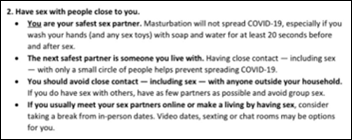
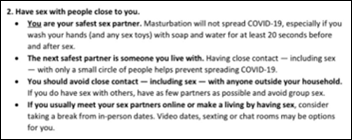
NYC Health’s guide to sex and COVID-19 suggests not having sex with anyone outside your household, noting that “you are your safest sex partner” in advocating video dating, sexting, and chat rooms. It also helpfully notes that shared keyboards and screens should be disinfected after their use for those purposes.
Sponsor Updates
- Bluefield Regional Medical Center (WV) uses Live Process software to notify managers of updated COVID-19 communication and guidance documentation.
- Meditech announces event changes for March and April.
- Spok appoints Christine Cournoyer (N-of-One) to its board.
- CompuGroup Medical sets up a dedicated website and phone line for providers to request six months of free CGM ELVI Telemedicine.
- Experity publishes “E/M Coding for the 2019 Novel Coronavirus (COVID-19).”
- Relatient names John Glaser to its board.
- Vizient awards a group purchasing contract to CI Security for managed detection and response cybersecurity services.
- ROI Healthcare Solutions creates a virtual booth after the cancellation of several conferences.
- Impact Advisors posts a white paper titled “Keeping Your EHR Implementation On Track Amid COVID-19.”
- StayWell creates a COVID-19 resource hub for patients, members, and communities.
- The Dallas Business Journal features T-System’s efforts to offer providers COVID-19 documentation resources.
- Voalte parent company Hillrom donates $5.5 million in medical devices for critical and intensive care to 25 hospitals fighting COVID-19.
- PerfectServe offers clients free COVID-19 automated patient and family outreach software and free services to implement best practices.
- Wolters Kluwer Epidemiologist Mackenzie Weise appears on a special PBS “NewsNight Conversations: Coronavirus.”
- Zynx Health publishes new COVID-19 order sets and care plans.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.
































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…