HIStalk Interviews Suresh Venkatachari, CEO, Healthcare Triangle, Inc.
Suresh Venkatachari is chairman and CEO of Healthcare Triangle, Inc. of Pleasanton, CA.

Tell me about yourself and the company.
Healthcare Triangle combines two great companies, each successful but stronger together. One is rooted in proven healthcare and business methodologies, and the other is a born-in-the-cloud early adopter turn global leader. Together, we are a 360-degree solution with the know-how and innovation capacity to meet technology, data, care delivery, and business operation needs.
We offer solutions to three core healthcare customers — hospitals and health systems, health insurers, and life sciences companies. I’m proud of our commitment to support each one’s respective effort to improve health outcomes by enabling the adoption and optimal use of new technologies, data enlightenment, business agility, and response to immediate and emerging business needs and market trends.
I have 30-plus years of experience in creating and managing businesses in cloud, ecommerce, IT solutions and consulting services in healthcare, life sciences and banking. But nothing compares to the excitement of today’s healthcare innovative landscape.
How does the combination of traditional health IT consulting, such as EHR implementation and optimization, and cloud transformation and security benefit clients?
I am incredibly excited by this combination and its advantages. Our traditional consulting background helps us understand the complex challenges that are facing healthcare CIOs in the current ecosystem. Our technology expertise in cloud transformation and security in the life sciences space means we understand the power of cloud transformation in highly regulated environments.
The combination also guides our clients on a practical and achievable roadmap of digital transformation. For one hospital, for example, our work focus might be disaster recovery and backup, while simultaneously leading higher-level discussions on end-to-end managed healthcare IT services with the C-suite executives. Simply stated, we are all about alleviating a lot of headaches for the CIO with solutions for operational efficiencies and lowered costs.
What’s really thrilling is that bigger picture, the healthcare industry is on the cutting edge of realizing a monumental pivot among healthcare providers and life sciences. Significant high-tech advancements are happening in personalized healthcare at every stage of the patient’s healthcare journey. Innovative and customized solutions are reshaping delivery of better access to smarter and more effective care to everyone.
What pandemic-driven technology challenges and opportunities will health systems see in the near future?
We’ve recently highlighted key challenges with technology extensively in our “Return to Revenue” series. But underlying that, the greatest challenge will be maintaining the business agility that is needed to react quickly and deploy those technologies that have an impact on patient safety and are demanded by the patients themselves.
Our clients succeeded in meeting the COVID-19 crisis head on by rapidly adopting and adapting telehealth technology. Next, we recommend that they go to the next level by deploying virtual waiting rooms and exam rooms, in-home monitoring, and data solutions. Traditionally, these types of projects take years to plan and implement, but we’re seeing increasing need to drive change in weeks and even months. HTI is their enabler to continue to iterate quickly and set a roadmap for continuous practical innovation.
On the life sciences side, we witnessed two immediate COVID-19 related challenges. First, the need to analyze data extremely rapidly. Second, the need for rapid deployment of digital health technologies.
We have a customer, Stay Smart Care, who is the perfect example of digital health excellence. Their business purpose is to help people safely age in place in their home. Stay Smart Care offers remote patient monitoring, with real-time sensor data, dashboards, and chat functions. We built the entire digital health platform, from the digital health management application to the secure, compliant patient communication application. This technology offers amazing potential in multiple areas of telehealth.
My team has a deep knowledge of the healthcare system, cloud technology, and digital health applications,. We are advising our clients about solutions that will help them navigate and succeed in the next normal of telehealth.
How have the data sourcing and analytics needs of life sciences companies and researchers changed as they address COVID-19?
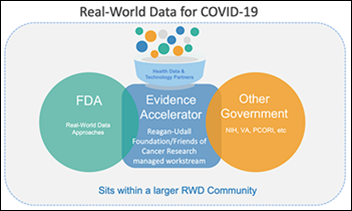
COVID-19 has dramatically fast-tracked research toward treatment and prevention. New collaborations are springing up to protect public health. Not surprisingly, researchers and life sciences companies find themselves having to obtain, analyze, and share a high volume of test results and other data rapidly and safely. The solutions we offer for cloud transformation make management and analysis of that data less challenging and allow researchers and life sciences companies to focus on what counts most, which is saving lives.
Specifically, our DataEZ solution – a data lake as a service, if you will – is used by five of the largest global pharma firms. It allows rapid analysis of clinical trial information, for example. One client went from conducting clinical trial to submitting the reports to compliance agencies in a matter of weeks. Before this, the process required several months.
Health system IT departments have quickly rolled out new technologies such as telehealth, chatbots, and remote worker support, delivering quick wins rather than the more typical implementation projects that can take years. Will this experience change how those IT departments manage projects and technology going forward?
We did see some very quick technology implementations over the last few months. I hear health system leaders talking positively about the quick consensus-building and lean approach to implementation that it took to make that happen. It is a very agile approach to deploy a solution and iterate on improving it over time based on real-life experience impacting productivity and costs. We focus on delivering business agility whether we are supporting a cloud migration, providing data insights, or optimizing an EHR workflow, and I hope that momentum is sustained going forward.
How will cloud-based services change the job of the health system CIO over the next five years?
We’ve been saying for years that the role of the CIO is changing from functional technology leader to business strategist and transformationalist. Trends in innovation driving that change are digital health, personalized healthcare, telehealth, remote monitoring, data-driven decision support systems, and blockchain innovation. Cloud is the key that unlocks the capacity in our client CIOs.
Taking advantage of cloud technology and automation means that CIOs can focus on full-scale organizational transformation and drive business agility into their technology platforms. Instead of 30-day cycle to spin up a server, we’re talking seconds on the cloud. And that’s a cascading effect, right? Every win along the journey to the cloud allows the organization to transform faster and faster in today’s changing environment and our client CIOs to drive that change rather than constantly react to it.
What are your medium-term goals for the company?
We want to drive the conversation centered around digital transformation into a new phase of bold action. The disruption to the industry and our communities demands that we use technology to strengthen our ability to deliver healthcare despite the impact of external forces. We are flexible and practical. We will meet clients wherever they are in their digital transformation and make great advancements together accelerating the value that they see from technology.
The drive to improve care delivery and business agility in healthcare is limitless. I know that we are ready as an industry to deploy new technologies, gain enlightenment through data insights, and push toward the next frontier of digital innovation. That’s what Healthcare Triangle is here to do — to reinforce healthcare progress.







































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…