Monday Morning Update 1/4/10
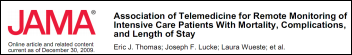
From Ned Flanders: “Re: remote ICU monitoring. Publication bias apparently runs both ways. JAMA rejected a study evaluating the clinical and financial impact of remote ICU monitoring last year because although the results were extremely impressive, they claimed the study had a weak design (before and after) and did not shed light on the actual reasons why remote ICU monitoring helped (since it had already been shown to help). Curious considering the recently published study had the same design and flaws, with the only difference being outcome.” This highlights a little-appreciated reason for not believing everything you read: the most powerful influence wielded by publishers isn’t how they spin a particular story, it’s their choice of which stories to include in the first place. That process has zero transparency to readers, so it’s the most dangerous. The second most powerful is where the piece appears if it is published. The third is how the headline (or abstract) is worded since many people will base their conclusion, consciously or subconsciously, on that alone.
From FinSoft: “Re: QuadraMed. Jim Klein is out – read the 8K from December 30.” This was actually reported by Misys_ex to me in early December, but I always hesitate to run rumors about named individuals unless it’s public knowledge since I’d hate to see my own name in “he’s been fired” speculation (no need to give the boss ideas). Jim was SVP of product management and CTO until his “involuntary termination”. Some degree of executive change is all but mandatory when a company is acquired. Companies don’t generally buy other companies because they don’t want to change a thing.
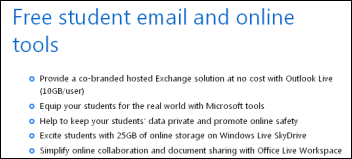
From Anne Onymous: “Re: HHS rules. For years, vendors charged a fortune for simple interfaces to the systems of other systems. Now, in order to get certified, they have to offer this interoperability. In addition, they may not be able to charge for it! There are no provisions for them to charge for receiving patient data, although there is no mention about sending patient data (I could have overlooked it). I predict that in the final rules, certified vendors will have to receive select patient data and respond to inquiries for it from other certified systems at little or no cost. This is reasonable and necessary for patient care. The impact of these rules will be very positive for vendors that provide niche applications.”
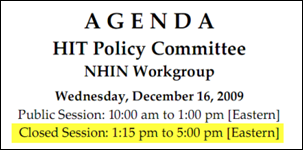
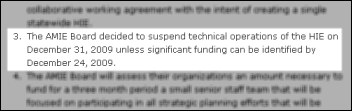
From Downtown: “Re: meaningful use. Awesome summary. Will anyone other than attorneys read the whole thing? With an unusual lack of fanfare, ONCHIT seems to have published a new Web site, StateHIEResources.org. It was registered on the 13th by some Canadians. Now I’m really confused!” I signed up for the listserv and it’s apparently a follow-up to (and the same domain registrant as) the State Health Information Exchange Leadership Forum, run by AHIMA “through a cooperative agreement with the Office of the National Coordinator for Health IT.” The new site has no AHIMA reference. ONCHIT apparently offshored its Web development to Canada.
From ChiSalesChick: “Re: a big EMR vendor I won’t name. They are ‘restructuring’ a lot of their sales people right out of a job.”
From Cleveland Brown: “Re: HIStalk. I was scrolling down the sponsor list yesterday and thinking about how far your little blog site has come in the years that I have been reading. All of your hard work and your integrity surely has brought you well-deserved respect and fame (if not fortune). Thank you so much for producing the one blog that I turn to daily! I do admit, however, that I do not share your site with many of my peers. It is important for my ego to always know more than anyone else and reading HIStalk makes it so.” Lots of readers have confidentially told me they keep their HIStalk reading habits secret for the same reason, which is flattering and amusing. I guess that does slow the word-of-mouth effect, although I note that December’s HIStalk visits were up nearly 40% year-over-year, which is closer to shocking than merely surprising since I keep figuring that anyone who cares has already found it.
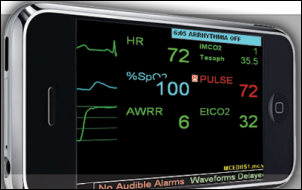
Speaking of the remote ICU article, thanks to the reader who sent over the JAMA full text article. The article by a University of Texas Medical School associate professor looked at mortality, complications, and length of stay before and after implementation of Philips VISICU in six ICUs in five hospitals (in a single health system) from 2003 to 2006, using around 2,000 randomly selected patients (about half the total). Hospital mortality dropped a little, but that was not statistically significant after adjusting for severity. There was minimal effect on complications and length of stay. The big gotcha: two-thirds of the patients studied had doctors who allowed the intensivists to intervene only in life-threatening situations, i.e. they were not really letting the remote intensivists manage those patients. Also: the hospitals did not integrate their CPOE and progress notes into VISICU, so all the intensivists had to work from was a daily fax (note the irony that, among all that expensive technology, the only “interface” was a daily fax from one user to another). My conclusions (crediting Smalltown CIO for some thoughtful comments left on my original post about this article): (a) as is often the case, implementation decisions had more impact on outcomes than did the technology itself; (b) you could flip the conclusion around and say that, since tele-ICU had no negative impact, it provides opportunities to maximize use of scarce resources; (c) rural sites could use tele-ICU and keep the patient closer to family members without negatively impacting outcomes (and helping support those rural facilities instead of big academic medical centers); and (d) hospitals buying remote ICU monitoring technology should first see if local docs will support it by letting those remote intensivists do something more than just provide off-hours fire watch coverage.
Speaking of tele-ICUs, Advanced ICU Care, a St. Louis ICU monitoring service whose 60 intensivists and ICU nurses use VISICU, raises another $2 million of investor money, bringing its total to $12 million.
It’s a new year – time for parades, bowl games, and HISsies nominations. Tell me your thoughts about 2009’s best and worst vendors, the smartest and stupidest vendor moves, and of course the granddaddy of all HIT industry awards: your choice for “HIT industry figure in whose face you’d most like to throw a pie.”
Another New Year’s tradition: newspaper profiles of the local hospital’s first baby of the year, which as I annually note, seldom involves married parents.
Listening: Boston-based Lyres, which sounds like the Animals or Seeds time warped from a 1960s garage into the 1990s with their Farfisa organ in tow.
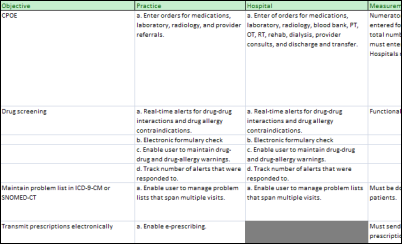
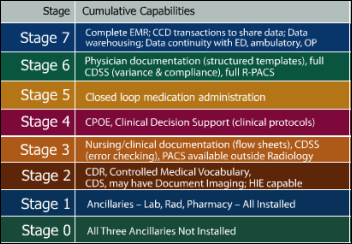
HHS didn’t make its proposed Meaningful Use standards easy to work with, scattering them over two verbose PDF files (they didn’t exactly lead by example when it comes to discrete data and interoperability). I pored over the documents again in my usual nerdy New Year’s Eve (while watching some guy doing an Evel Knievel-style car jump on TV and all three hours of Rush in Rio) and put the actual criteria and thresholds into a handy-dandy Excel worksheet (note: it looks crappy in the preview, but perfect once you download). It spells out the provider parts of the MU requirements in concise detail. Certification and payment specifics means nothing if you can’t look down this list and nod your head that, hey, we can do all this stuff on the computer. Let me know of any additions or changes. I numbered the criteria just for reference, but it’s a made-up number.
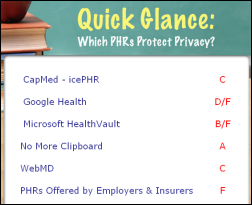
Some thoughts on the proposed Meaningful Use criteria:
- I’m trying to figure out who the big winners will be if these criteria are approved. Consultants for sure. Companies like RelayHealth that provide eligibility, claims, and information exchange services. Companies that can perform a security analysis. Vendors that offer a usable medication reconciliation function. Vendors with patient portals. Companies that can help put vital signs information directly into the EMR.
- Losers: EMR vendors already strapped to pay for CCHIT certification who now have to cough up another million or two to meet the additional requirements. That’s another blow to small and innovative vendors who aren’t raking in the cash, meaning the market tilts even more in favor of the older, bigger ones whose sales were so limited that the government decided to intervene in the free market in the first place. Market consolidation is probably good, but I expect the development agenda will now be even more driven by Uncle Sam, not users (especially since the HITECH sales window is small, so even sales-driven innovation may dry up once everybody has chosen their dance partner).
- Lots of folks, me included, expected the criteria to be a slam dunk for moderately tech-savvy hospitals and practices. Not so: considering the small percentages of them using CPOE and e-prescribing, the minority that can provide electronic copies of information to patients, and the small number of practices that can provide patients with fast access their online health information, the these are stretch goals. I bet those requirements will be dialed back in the final version for that reason.
- Good luck with providing the denominator number for the reimbursement measures. You will need to know the total number of prescriptions generated, the number of orders issued, and the number of episodes in which medication reconciliation should have been performed. The document indicates an estimated time to generate the denominator at one hour using the EMR’s capabilities, which is surely a mistake since the EMR doesn’t help you count paper orders.
- The CPOE requirement is generous to hospitals, which have been screwing around since the 1980s trying to get doctors to use CPOE with dismal results. They are required to hit only 10% CPOE usage since “CPOE is traditionally one of the last capabilities implemented at hospitals.” (like, decades after buying it?) Practices, most of them considering their first EMR in a quick ramp-up to earn HITECH money, need 80% usage right out of the gate. I expect changes here, too, with the hospital target raised and the practice one lowered.
- With the minimal CPOE usage required for hospitals, the five required (and undefined) clinical decision support rules won’t have much impact on patient outcomes.
- The report cites a pseudo-fact that, “Some vendors have estimated that EHRs could result in cost savings of between $100 and $200 per patient per year.” Vendors say a lot of things, but I believe only those that are enumerated in a contract, preferably with rewards or penalties to encourage backing up self-serving statements with risk. I’m not sure I would have included that stat.
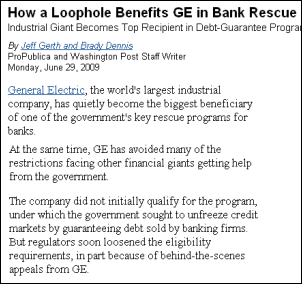
- The report used the high estimate of EHR cost from a range of $25,000 to $54,000 per provider, stating that “we believe the cost of such technology will be increasing.” Why should software costs increase when user bases are increasing, which should allow vendors to spread their fixed software development costs over more users? The only one factor that would raise the price is the vendor cost of complying with certification requirements (government meddling in free markets never comes free).
- That higher upfront EMR cost makes the elusive $44K jackpot even less enticing. Doctors were already avoiding EMRs because of cost and negative workflow impact. Providers are questioning whether they can qualify for the incentives and whether they trust the government to pay them.
- Conclusion: if you like the idea of having the government use taxpayer money to encourage the use of specific products in the pursuit of lofty and possibly unrelated goals, this at least pushes some theoretical behavior change in the users who choose to participate. If you’re a provider trying to decide whether the government money has too many strings attached, this might convince you that it does. And if you asked me how the odds of high EMR utilization changed with the release of these proposed requirements, I’d say they got worse.
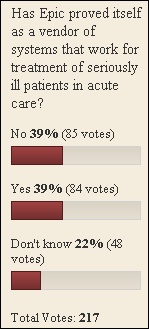
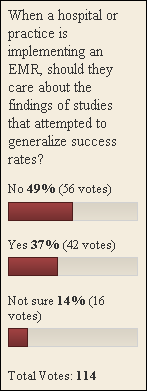
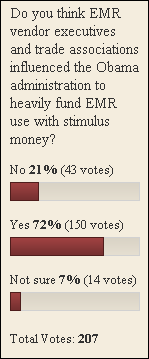
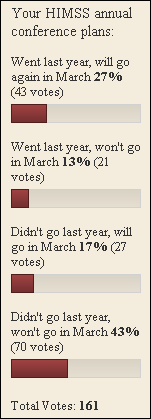
Apparently we are not collectively certain that Epic is a proven solution for acute treatment of seriously ill patients, at least based on the results of my last poll. A new one to your right (or lower left if your screen resolution is set low): are the initial Meaningful Use criteria too easy for providers to meet, too hard, or about right?
I love this newspaper article because it reminds me how shocked I was the first time I saw what it describes first hand: the person in scrubs assisting a surgeon performing an OR procedure is sometimes an unlicensed salesperson of the medical device being used. In addition to the skilled medical personnel in the OR, “at the foot of the operating table, there’s Chuck Bates, a guy who studied biology in college and always wanted to go to medical school but never did. Instead, he began his career selling hot dogs to grocery stores. As the surgeon prepares to make an incision, Bates stares at the X-ray monitor. Come up one centimeter and make your incision there, Bates tells the surgeon.”
This is what the lure of taxpayer-funded EMR Welfare has done. An Indiana group holds its first planning meeting about applying for $15 million in federal HIT money (the Beacon Community Program) even though the representative of the only hospital involved (and the main beneficiary of the grant) skips the meeting because he’s on vacation. Their application is due January 8, so they met without him. The county health department director figured the financial windfall would be nice, but low EMR provider usage makes the group a pretty poor EMR beacon for the country to follow: “It’s been a real struggle. The hospital’s computer system has been crap. I’m not sure it is even 15 percent, let alone 25 percent.”






































































There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…