Bob Katter, MBA is president of First Databank.

Tell me about yourself and the company.
I’ve spent my entire career in healthcare, primarily health IT and a little bit of health services. Before joining First Databank about 15 years ago, I was with RelayHealth and then McKesson for several years. At First Databank, I’ve previously headed up the commercial and consumer-facing functions, and then at the start of 2020, right in time for the pandemic, I took on the role of president.
First Databank, which I think is referred to by most in the industry as FDB, is one of those companies that few people outside of the industry or even inside it have heard of. We play an important role. Many healthcare delivery organizations, probably a majority, count on us to provide timely and accurate medication information. We support a whole range of clinical, administrative, and financial workflows. We aren’t an application, per se. We’re the content that supports it. That can be an EHR system, a pharmacy management system, a claims processing system, and other types of systems.
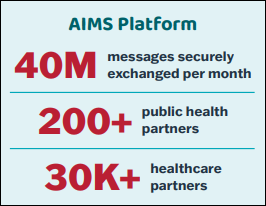
We recently expanded beyond that core business to get into the e-prescribing network business with FDB Vela. It’s different than our core content business, but also related, in the sense that a lot of the customers, the people who use the network, are the same people who use our medication content. We think that our expertise with the content gives us a unique and special way to do that e-prescribing network.
How has medication decision support changed in terms of personalization and making the information actionable to the correct person?
You’re absolutely correct. That is our core business, and in many ways, is the most important thing that we do. It is changing a lot, and I think it’s about to change a lot more because of the advances in technology and generative AI.
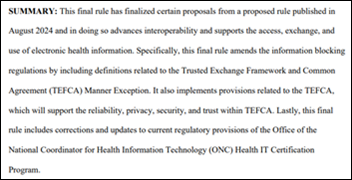
Everyone is probably saying something similar, but even prior to these recent advances in AI, just through FHIR and those types of things, we’re seeing a much greater ability to pull information from whatever clinical system in which our content is being used to make the content or the decision support that we provide more patient specific and more actionable. The clinician not only gets the patient-specific information, but is in a good position to act on it right then. A clinician should consider a number of patient-specific factors when ordering a med, for instance. Those include demographic factors, which we’ve also always had, but also clinical factors such as diagnoses, allergies, other meds the patient is on, lab values, risk scores, and increasingly, a patient’s genetic profile.
The technology is evolving to the point where we can access this information in real time and provide that succinct kind of impact statement. “Here’s what that means for this patient in this order,” and even give some sense to the clinician not just as a safety check, but potentially a more actionable, “Here’s what you ought to do.” We are doing that in the hospital setting. We are also doing that in the pharmacy setting. We’ve rolled out a program with CVS that we’re excited about. They don’t call that decision support, they call it DUR, drug utilization review, but it’s a pretty similar process. It is focused on very patient-specific information and focuses on the actions the clinician should take as a result of this information.
How might that process be changed with generative AI, which could help make sense of the information in context or tie into external references?
As you can imagine, that is question that my senior team and I are spending a lot of time on. In terms of building on what I was talking about a minute ago about patient-specific decision support, one thing that these large language models can do better than any other technology that we have worked so far is to take unstructured data and do a reasonable job of structuring it. Through standards, there are ways to pull structured data out of an EHR and put structured data back into an EHR. We are doing that with several EHR partners. But a lot of the data inside a chart, including meaningful and useful data, is in text form, in an unstructured form. The LLMs provide a lot of promise in terms of being able to pull data out. We are working on that right now to support several clinical and administrative workflows.
Something else that this type of technology can do is in the area of so called real-world evidence that people have been talking about. You can essentially ask the technology, what have clinicians done for thousands of other patients that look very similar in terms of clinical context to this patient? I don’t think that necessarily provides a definitive answer, but it’s another perspective that you can surface in front of the clinician that would be useful advice when combined with the so-called traditional evidence that FDB and companies like us have based our content on to this point.
In our AI testing, it’s very good, but it’s not at the near-perfect or perfect standard that I think our industry will require for clinical decision support. There remains a role for experts to guide and manage the technology. In our business, 99% is not nearly good enough. We’re talking about a 99.9999% standard. Based on what we’ve seen, to get to that level of accuracy and consistency will require expert humans along with it. That said, there’s no doubt the technology is very powerful and is continuing to advance. For pulling things that are unstructured and structuring them, as well as offering that real-world evidence component, we think the technology is going to become very useful.
What opportunities does a prescribing network such as Vela provide in connecting not just providers, but other types of participants, such payers?
In terms of other types of participants, the current network and Vela support all of the NCPDP standards. The currently available networks already support connectivity between the prescribers who use an EHR system; the payers, if you consider the payers to be PBMs in this case; as well as the pharmacies. But one constituent that is left out of that equation is the patient themselves. We think that is important.
Vela supports a workflow where the patient doesn’t receive an actual prescription that they can do anything with other than forward it. Patient choice becomes an important component, and the networks should support that. That has been done in the past by having a patient-facing app mimic a pharmacy, but we don’t think that’s the right workflow because it removes subsequent pharmacy-to-physician communication that the standards support. You need to have a different role. Thankfully, NCPDP has worked with us and there is a standard that supports that. You need to have a different role for the patient, and that’s an important constituency.
When you get into specialty drugs, you can use the prescribing network for all the standard things. But when you get to prior authorization, specialty enrollment, and patient financial responsibility, those are all separate transactions that the provider’s office has to manage separately. We think there’s a real opportunity to pull all of that into one unified system. The provider would write the prescription in the EHR system. Then, all of the information that you need to support those subsequent workflows — whether that’s a real-time patient benefit request, a prior authorization request, or specialty enrollment request – can be done with data or content from the EHR. That’s where you get back into pulling things out of the EHR that are unstructured and the promise that AI has for that as opposed to just structured information. There’s a lot of opportunity to innovate in that area.
We’re up to somewhere around 10 or so partners that have consumer-facing applications. Something that the patient can use, typically on their phone, to manage their prescriptions. Our network supports the standard by which that application can essentially receive a copy of that prescription, and then the patient has the ability — depending on which application it is — to do all sorts of things that include choosing a pharmacy from the pharmacy network and decide where they want that prescription sent.
It’s also an excellent opportunity to surface other things. You mentioned real-time pharmacy benefit. That, along with a coupon from a company like GoodRx, allows the patient to make intelligent decisions based on their financial responsibility. They can seek to fill the prescription at a pharmacy where they can afford their co-pay or co-insurance, for instance. We also think that here’s an ability, once the patient is in that workflow, to provide information around adherence and things that are going to help that patient fill that drug initially and stay on that drug subsequently. We’re not an application company per se, but we will support any kind of NCPDP-compliant application that can manage and forward prescriptions.
How extensive is the use of precision medicine and genomics in in ordering drug therapy?
There are several hundred drugs that have good, published clinical evidence to support it. A lot of those are in the central nervous system area, mental health drugs, pain drugs. There are certain therapeutic categories where there tends to be more evidence. It’s very specific, such as if you have this particular genetic variant, you’re going to metabolize this particular drug differently, so you need to change the dosing. Sometimes it’s an absolute contraindication given a genetic variant, where we would advise the clinician to prescribe a different drug.
A couple of years ago, I would have said that this is something that we love talking about, but we’re a little out in front. It’s very much going mainstream now. We’re getting both public and private hospitals adopting it, particularly those that use Epic and Meditech EHRs. We are finally starting to see this come into clinical practice in a major way.
What is the status of recording and using medical device information?
For several years, we have published a database called Prizm. It’s a comprehensive database of Class I, Class II, and Class II medical devices. It’s fairly different than medications, and maybe even we didn’t understand how different it was initially. Medical devices are not managed in the same way as drugs. There isn’t that definitive set of content or set of therapeutic categories anywhere near to the same extent as drugs. We are continuing to work with health systems and starting to see traction.
In terms of the use cases, there are almost too many to list, but I guess I could just throw out a couple of pretty obvious ones. One is inventory management. If you truly understand which devices are in which categories, even to the point where you could substitute this particular device for this other device if supply is short or the price goes way up, then hospital systems should be able to manage their inventories much better and probably save a lot of money in the meantime.
There’s also a patient safety aspect to this. Somebody in a hospital told me a couple of years ago, and I hope it’s not completely true, that, “We probably have a better idea of what cans of food are on our grocery store shelves nationwide right now than we do of which devices we’ve implanted in which people.” This idea that we’re putting implantable devices in people and we’re not able to completely keep track of which patient has which device or which generation device it is, affects decision support as well as recalls. I may be being a little too critical of how that’s managed, but I think that with a more standardized content source, the industry can do a much better job.
What consumer-facing use cases do you see for your products?
There’s a big gap in what patients are prescribed. Maybe a Medicare patient has a number of meds and doesn’t understand why they’re taking them, how to take them in cases where it’s more complex than just swallowing a pill, or which meds they should take at different times. We provide specific information beyond the long, industry-approved monograph that covers everything. What are the most salient points that the patient needs to know?
There’s also a need to provide patient information at an appropriate reading grade level, which might involve using pictures or so-called pictograms that are more universal and easier for people to understand. Also making the information available in multiple languages. We have an incredible number of people living in the United States for whom English is not their first language. They might not understand something as complicated as medications in English. This is obviously another area where AI will provide tremendous assistance.
What are the company’s priorities over the next few years?
I’ve been spending a lot of time in the past year or 18 months thinking about that, given how fast things are changing. With the ongoing advancement and adoption of AI technology, clinical practice is going to change pretty dramatically. The amount of information that can be made available to clinicians to aid in their decision-making process will be immense, even relative to what it is today.
The priority for our company is to say, how do we play? If more hospitals are using ambient AI technology in patient encounters for charting, that might kick off a different workflow for how decision support works. We’re going to want to make sure that our information is made available in that setting. Maybe the clinician won’t be typing in the order and managing it the way they traditionally have. Maybe it will be more of a verbal process. A huge priority for us is to understand how those clinician workflows will change and how we can participate and remain valuable to the clinician in that process.
We will determine how we can leverage AI and real-world evidence in new ways. Not to stop doing what we do now in terms of the traditional evidence, but combine it with the larger amount of content and data that we can get using real-world evidence and how that combination of things can be more powerful.




































Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…