News 9/24/25
Top News


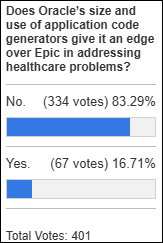
Oracle promotes Clay Magouyrk and Mike Sicilia to co-CEOS, replacing Safra Catz.
Magouyrk was president of Oracle Cloud Infrastructure and has been with the company 11 years. Sicilia joined the company in 2008 and most recently was president of Oracle Industries. Both were heavily involved with Oracle’s AI work.
Sicilia, a former lobbyist, was an early post-acquisition spokesperson for Oracle in several federal hearings about the VA’s stalled Oracle Health project. He is a regular critic of Epic and CEO Judy Faulkner. CTO Larry Ellison said, “Mike has spent the last several years modernizing Oracle’s Industry applications businesses, including Oracle Health, by completely rebuilding those applications using the latest AI technologies.”
The promotions were first disclosed in a June SEC filing.
Sponsored Events and Resources
None scheduled soon. Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock

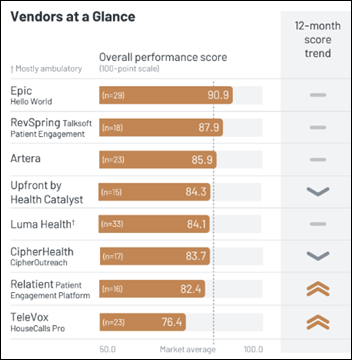
Patient communications and payment solutions RevSpring will acquire Kyruus Health, which offers provider search and scheduling.
Pharmacy benefit manager and administrator Capital Rx rebrands to Judi Health, the name of its AI-powered health benefit management platform, and announces $400 million in new funding. The company has raised $732 million since its 2017 launch. I interviewed CEO AJ Loiacono last October.

Patient Square Capital will acquire tech-enabled group purchasing and supply chain company Premier Inc. in a $2.6 billion take-private deal. Premier, which went public in 2013, has been evaluating strategic alternatives for two years.

Prosper AI raises $5 million in seed funding. The company develops AI voice agents for patient access and administrative workflows.
Enterprise telehealth vendor Caregility announces $25.1 million in new funding, bringing its total raised to $92 million.
Diabetes software vendor Glooko acquires Monarch Medical Technologies, which offers a glucose management system. Glooko’s CEO says the acquisition will support its efforts to deliver a full hospital-to-home service.
Sales
- The New York Office of Mental Health will implement Oracle Health’s EHR across 24 inpatient psychiatric facilities and 300 outpatient programs.
- Yale New Haven Health (CT) will roll out Artisight’s Smart Hospital Platform, initially focusing on virtual nursing.
People

ReferWell names Loren Koerber (Medecision) VP of strategic account management.

Jason Bond, MBA (CareAbout Health) joins Sevaro Health as CFO and SVP of strategy.

Matt Rockhold (GE HealthCare) joins Thynk Health as chief commercial officer.

Joe Moscola, PA, MBA (Northwell Health) leaves the organization and will offer advisory consulting services.

Allymar Health Solutions hires Cecil Lynch, MD, MSc (Accenture) as CMIO.

Scottsdale Institute appoints John Glaser, PhD (Harvard Medical School) as board chair, replacing co-founder Don Wegmiller.
Announcements and Implementations

Sutter Health (CA) will use Epic-connected medical devices in its Sutter Sync digital care program for patients with chronic conditions and pregnancy.
Quest Diagnostics announces a collaboration with Epic to integrate its lab operations nationally, streamlining ordering, results, billing, and patient engagement through technologies like MyChart as part of its Project Nova initiative
Micromedex adds AI-powered drug information search for clinical decision support.
Government and Politics
VA Electronic Health Record Modernization Integration Office CNIO Toni Phillips, RN touts the new Oracle Health-based federal EHR’s streamlined medication administration capabilities, noting that the clicks to scan patient IDs have been reduced from 15 to two.
Sponsor Updates
- Worcestershire Acute Hospitals NHS Trust’s review of Altera Digital Health’s Sunrise EPR finds that the system has delivered significant advancements in care quality, patient safety, and clinical efficiency.
- Black Book Research publishes a new report titled “The Middleware Mandate.”
- Linus Health, Navina, and Wolters Kluwer Health will exhibit at AAFP FMX October 5-9 in Anaheim, CA.
- Clinical Architecture sponsors CHIME Innovation Summit Southwest through September 25 in Irving, TX.
- Consensus Cloud Solutions will exhibit at the HIMSS Gulf Coast Conference September 24-26 in New Orleans.
- Divurgent releases a new episode of “The Vurge” podcast celebrating the company’s 18th anniversary.
- Canopii Collaborative names Brady Thomas account executive.
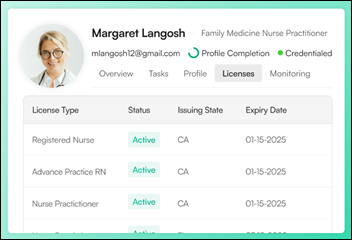
- Symplr adds capabilities to its Operations Platform that unify provider data.
- Surescripts announces the 11 winners of its 2025 Surescripts White Coat Award.
Blog Posts
- Emerging Trends and Challenges in Healthcare Revenue Cycle Management (AGS Health)
- How clinical decision tools improve healthcare and potentially reduce malpractice risk (Wolters Kluwer Health)
- Arcadia Customers Outperform National Average in 2024 MSSP (Arcadia)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Sponsorship information.
Contact us.






























Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…