Monday Morning Update 6/14/21
Top News
A federal court indicts the COO of Atlanta-area Internet of Things security vendor Securolytics, claiming that he launched a 2018 cyberattack against Gwinnett Medical Center (now Northside Hospital Gwinnett) for personal financial gain.
Vikas Singla allegedly disrupted the hospital’s phone service, obtained information from a digitizing device, and disrupted network printing for unspecified purposes.
Singla pleaded not guilty to 18 charges, was released on $20,000 bond, and will return to court June 23.
HIStalk Announcements and Requests
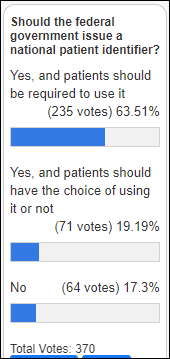
Poll respondents are nearly universally in favor of implementing a national patient identifier, with the majority of those believing that its use should be mandatory.
New poll to your right or here, as suggested by a reader: Looking back five years, which aspects of healthcare have been significantly improved by technology?
Reminder: I’ll include HIStalk sponsors who are exhibiting at and/or attending HIMSS21 in my HIMSS guide if you submit your details. Meanwhile, It’s not even summer yet and Las Vegas will have daily highs in the 117-degree range for most of this week, to the point that motivational speakers could convene one of their BS firewalking rituals by just having participants take their shoes off and walk 20 feet on a Strip sidewalk.
It feels as though the industry is taking an actual summer break, as opposed to the never-ending virtual connections of 2020, given the absence of significant news over the weekend. Shockingly, I saw no new announcements of money-losing companies that I’ve never heard of being valued at billions of dollars, no eye-rollingly fawning articles describing how AI will disrupt healthcare, or non-experts seeking attention by claiming that Cerner or Meditech or some other company might be acquired by someone someday. It may be that everybody is saving their energy for HIMSS21, but I suspect that isn’t the case and instead we’re just enjoying a return to pre-pandemic summer life. At any rate, enjoy today’s minimal reading time since I have no incentive to dishonestly pad things out just to hold your attention.
Webinars
June 24 (Thursday) 2 ET: “Peer-to-Peer Panel: Creating a Better Healthcare Experience in the Post-Pandemic Era.” Sponsor: Avtex. Presenters: Mike Pietig, VP of healthcare, Avtex; Matt Durski, director of healthcare patient and member experience, Avtex; Patrick Tuttle, COO, Delta Dental of Kansas; Chad Thorpe, care ambassador, DispatchHealth. The live panel will review the findings of a May 2021 survey about which factors are most important to patients and members who are interacting with healthcare organizations. The panel will provide actionable strategies to improve patient and member engagement and retention, recover revenue, and implement solutions that reduce friction across multiple channels to prioritize care and outreach.
June 30 (Wednesday) 1 ET. “From quantity to quality: The new frontier for clinical data.” Sponsor: Intelligent Medical Objects. Presenters: Dale Sanders, chief strategy officer, IMO; John Lee, MD, CMIO, Allegheny Health Network. EHRs generate more healthcare data than ever, but that data is of low quality for secondary uses such as population health, precision medicine, and pandemic management, and its collection burdens clinicians as data entry clerks. The presenters will review ways to reduce clinician EHR burden; describe the importance of standardized, harmonious data; suggest why quality measures strategy needs to be changed; and make the case that clinical data collection as a whole should be re-evaluated.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Sales
- SouthEast Alaska Regional Health Consortium goes live on Nuance Dragon Ambient Experience.
Announcements and Implementations
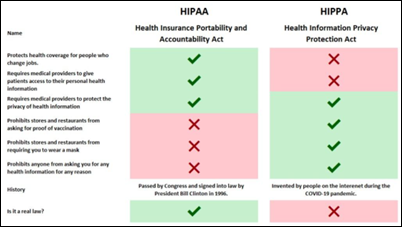
California will implement an electronic vaccination verification system “very shortly.” The state emphasizes that the unspecified system is not a vaccine passport because it will be offered only to private businesses who can decide for themselves how to use it, if at all.
Government and Politics
Captain James A. Lovell Federal Health Care Center (IL), a joint facility used by both the VA and DoD, will be the first test of interoperability between their respective Cerner implementations.
Sponsor Updates
- Waystar partners with career development nonprofit Inroads to launch a health IT internship program for local students.
- Healthwise has received seven Digital Health Awards for its patient education videos and content in the Health Information Resource Center’s 2021 spring competition.
- Netsmart VP & GM of CareGuidance AJ Peterson is included in the Kansas City Business Journal’s list of 2021 NextGen Leaders.
- Protenus publishes a new report, “2021 Diversion Digest: COVID-19 Conceals True Scope of Clinical Drug Diversion in 2020 as Incidents Left Undiscovered.”
- Talkdesk names Laura Butler (Workfront) chief human resources officer.
- Tegria publishes a new white paper, “Cloud-Based Managed Services Allow Healthcare Organizations to Do What They Do Best: Focus on Patient Care.”
Blog Posts
- Worrying About Being Sued – A Call to Action (Nuance)
- Polishing your portal to empower patients (Nordic)
- How Wearable Technologies are Creating New Clinical Trial Endpoints (PatientBond)
- Billions of $ in Funding for Public Health: 3 Strategies to Make the Most of It (Pivot Point Consulting)
- How Cyber Insurance Fits Into Your Cyber Security Posture (Fortified Health Security)
- How Can We Make Healthcare Billing Easier for Nephrologists? (PMD)
- How Updated Star Ratings Impact Your Hospital (Premier)
- 4 Ways to Improve Your Patient Communication Outreach (Twistle)
- Stretched to Their Limit, Doctors and Nurses Account for 67% of Drug Diversion in 2020 (Protenus)
- A Tale of Two Ransomware Attacks: Which Company Are You? (Pure Storage)
- How to Use HCC Analytics to Improve Provider Education and Point-of-Care HCC Capture (RCxRules)
- 6 Ways to Influence HCAHPS with Interactive Technology (Sonifi Health)
- PCI Data Discovery Tools: Is Your Organization Protecting Its Data? (Spirion)
- 6 things to know when purchasing on-call scheduling software (Spok)
- Enhancing the member experience with help plan fulfillment services (Krames)
- What is customer experience and why it matters in your contact center (Talkdesk)
- How Video Conferencing is Improving Patient and Family Communication (Vocera)
- 4 steps to getting the most out of your analytics (Waystar)
- 3 Reasons to Adopt a Team Treatment Systems in Your PT Clinic (WebPT)
- Are Self-Signed Certificates Hiding in Your Interface Engine? (Zen Healthcare IT)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



















































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…