Karly Rowe, MBA is VP of new product development, care and identity products, at Experian Health of Franklin, TN.

Tell me about yourself and the company.
I’ve been with Experian for eight years. I oversee all of our new product development, the processes, the teams, as well as our identity and care management portfolio. Our Experian Health business is represented by the areas of revenue cycle management, identity management, care management, and analytics. We started in the market serving a group of providers.
What are the chances of the US implementing a unique patient identifier?
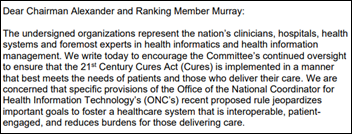
Now more than ever, there’s an openness to consider a national patient identifier, especially as topics of interoperability are getting more and more advanced through things like TEFCA. There’s a new acknowledgement within the public sector, the private sector, and the healthcare industry as a whole that a lot of the things that we want to achieve — in terms of true interoperability and improvement of care for patients and care coordination – all foundationally stem from having a national patient identifier in place.
I don’t have a crystal ball to predict whether that time will be tomorrow, next week, or a year or two years from now. But I do think that there’s been a significant shift and an openness, to where we are closer now than we ever have been to getting to a point to embrace the national patient identifier.
How would that change the company’s business?
I don’t see a large pivot. Our position is that there isn’t one key-holder to this identifier. It’s more likely and more beneficial that it’s a handful of vendors, of organizations, working together to provide it.
We collaborate with vendors across many other lines of business. Our core business is as a credit bureau. If you look at that model, Equifax, TransUnion, and Experian work together, collaborate, and share information as it pertains to individual’s credit to ensure that the information is the most accurate when going out to consumers.
For us in a healthcare setting, do we provide identity services? For sure. Would we be open and accepting to collaborate with other key leaders within the industry to make this something that could truly help transform the healthcare industry? 100%. There’s precedent that has been set across multiple aspects of our business. That credit example is just one of many.
Online services often ask people to verify their identity by choosing their previous address or a car they used to drive from a list of choices, something that they know that others would not. How is that being used in healthcare versus just taking a patient’s driver license or insurance card?
That’s a service that Experian Health has been providing to the healthcare industry for several years. We work with a lot of the patient portal systems and are integrated directly with them. We can help provide the confidence to our healthcare clients that the patient is who they say they are, before you then open up access to all of their personal health information that’s highly sensitive.
That’s something that we have carried over. Banks and financial institutions probably paved the way and were pioneers of setting that precedent. Healthcare is adopting that, as patient information is no longer on paper and it’s all electronic records. Access to that information needs to be protected and treated with the highest degree of security and sensitivity.
Surveys have shown that consumers, wisely or not, are willing to share their private information with companies that give them something in return. How will that play out in healthcare?
Even speaking for myself as a consumer, there’s a general frustration that we all feel when we say, “I can’t access all of my health information, my historical information, anywhere.” Unlike when I go online to look at my credit card statement and I can see all the transactions and I can look across multiple credit cards. The history, credits, and debits are all there.
It is absurd in healthcare that from a consumer perspective, if I wanted to do that today, I would have to individually reach out to find every doctor, every pharmacy, every lab test that I ever got, and manually go ask for that information. There’s a convenience where I would love to know that the care that I’m getting, the decisions that the doctor who’s standing in front of me is about to make on my health, are the best decisions.
The way for that doctor to make the best decisions is for me to provide the consent to say, you have access to that information, and there’s a way to pull that all together. The only way that that really happens is if you have an understanding of who I am as a patient across all of the different encounters that I’ve had. That stems by speaking the same common language, and the problem that we have today in healthcare is that we’re all speaking different languages. Everybody’s got a different way of identifying a patient and none of them interact. It’s like one health system speaking French, one speaking German, and another speaking Italian, all trying to talk to each other about a patient. It’s impossible.
Are health systems interested in using outside consumer information for patient engagement, marketing, or other communication that doesn’t involve only what the EHR contains?
Some are, but there are clear lines of distinction. This is where the patient plays a role in what information is being shared and for what purposes. There’s that clinical aspect of saying, I just want to be able to provide the history of my health so that that doctor has seen every lab result, every test, every procedure in their hands.
There is another element where, like in many other facets of our lives, we like the customization of the ads that are being sent to us, the coupons that are targeted to services that we enjoy, or the commercials. That transcends every other part of our life. In healthcare, there is an interest in saying, “Maybe there are pieces of who I am as an individual and the likes that I have. I’m OK with you having so that you can tailor my experience when I’m a patient visiting your portal or when I’m interacting with you as a healthcare system.”
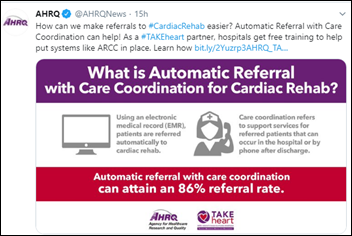
That starts to get into things that could improve the patient experience and their overall engagement. A lot of topics stem around overall care management, care coordination, and how that patient is being treated and receiving care. There are broader socioeconomic data factors that can assist in that. But I draw a line of distinction between those. For a lot of consumers and patients, clinical information is different and feels different than your lifestyle, behavioral, and socioeconomic type information. Patients may want to choose to share those things differently for different purposes.
Some of the first uses of commercial consumer information I saw in health systems were as simple as verifying a patient’s identity via the address they provided or to determine their propensity to pay. Is it a big leap from there to using social determinants of health?
We talked about having a patient identifier. Studies done by ONC on patient matching show that having reference data, knowing more about a patient than what’s present within a healthcare system, can help you get a better match. It’s the same in social determinants of health. They say 80% of health outcomes are attributed to non-clinical factors. That means the socioeconomic factors that surround someone.
If you take a step back and say, what am I willing to give to get, it is like what you said about consumers. If a consumer knows that they could receive better care or have better care decisions made for them if they allow the caregivers or the healthcare organization to have a more complete picture of who they are as an individual, I don’t know who wouldn’t sign up for that.
Protections need to be in place to make sure that there isn’t abuse. Organizations like ours take it very seriously — the types of data, how that data is being used, and adhering to all of the regulations that are set forth. One of the things that we stand by very strongly is that we’re an original source compiler, which means all the data that comes into us, we have direct relationships with all those data furnishers. That allows us to ensure the integrity of that data, how it is intended to be used, and the regulations that are involved.
Others are buying data from somebody who buys data from somebody who buys data. The further downstream you get and all those different extensions, the higher the risk goes in terms of that data being used for the wrong purposes and for purposes that wouldn’t make a patient feel good.
What trends are you seeing in the increasing number of uninsured patients and high-deductible health plans that leave them paying more?
Patients have two pain issues – paying a larger percentage of the total and wanting visibility earlier. Sometimes it’s not the total of my bill that bothers me, but rather that I don’t have visibility before I get that bill in the mail. We do a lot of work with many of our clients to put patient estimates in the hands of consumers so that they are not surprised by what a particular procedure will cost or what their bill will look like. That goes a long way in helping them have a dialogue and a conversation with their healthcare provider to understand whether they have options or flexibility.
That becomes critical, because it ties directly to the overall amount that the patient will ultimately be burdened with. There may be things that are optional within a patient’s care plan, there may be things that aren’t, or maybe there’s a drug that’s getting prescribed where there’s the option for a generic. Having that patient visibility into the cost up front allows that dialogue to happen, and maybe downstream to reduce that total burden and allow the patient to play an active role.
What is the expected outcome of Experian Health acquiring patient scheduling vendor MyHealthDirect?
What MyHealthDirect does is synergistic with what we do. We provide a lot of services that fall into the patient access realm. Bringing in the scheduling component to our suite of solutions, providing that ability to schedule a service, combining that with our matching and the correct identification of that patient, and then being able to facilitate the registration process, which starts to include running eligibility, looking at coverage, and providing those estimates. It’s really just continuing our breadth and advancing the more holistic solution of the patient access services that we can provide to our client base.
All of this ties around our broader vision of of helping improve the care coordination for patients on behalf of our clients. It’s a natural fit and tie-in with many of the services that we provide today, but it also allows us go back to our clients with a solution that helps them manage that upfront interaction with a patient from the point of scheduling an appointment.
Do you have any final thoughts?
We at Experian Health are excited about how we can help transform the healthcare industry, providing services and offerings to the market that are unique to our business. How we combine those, how we help solve challenging problems. One of the reasons I got into our healthcare space is that we have unique data and unique capabilities that, when hearing the challenges that our clients are facing, allow us to provide a differentiated solution. We’re excited about where we can help take the industry as we go forward.


















































1) RE: EMR down & good staff collaboration. I believe it. Having worked at a now defunct EMR for 15+…