News 5/26/21
Top News
AI-powered revenue cycle company Iodine Software acquires Artifact Health, which offers a physician engagement and patient documentation query technology platform.
Artifact CEO Marisa MacClary, MBA will join Iodine as EVP of the Artifact team.
HIStalk Announcements and Requests
A generous donation from reader Deborah, with matching funds applied from my Anonymous Vendor Executive, allowed me to fully fund the Donors Choose teacher grant request of Ms. H in Los Angeles, who asked for 3D geometry kits for her middle school class.
Webinars
June 3 (Thursday) 2 ET: “Diagnosing the Cures Act – Practical Prescriptions for Your Success.” Sponsor: Secure Exchange Solutions. Presenters: William E. Golden, MD, MACP, medical director, Arkansas Medicaid; Anne Santifer, executive director, Arkansas Department of Health – Office of Health Information Technology; Kyle Meadors, principal, Chart Lux Consulting. A panel of leading experts will provide practical guidance on how to prepare for the Cures Act. Will it upend your business model? What is information blocking? How can standardized technologies be applied to meet Cures Act requirements? What must I do now as well as in the next five years?
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Baptist Health South Florida severs ties with Health System Solutions, which had been handling the hospital’s revenue cycle management since 2018. BHSF created the RCM company as a joint venture with Navigant, transitioning nearly 600 hospital staff to the new business. The hospital will bring those employees back in-house.
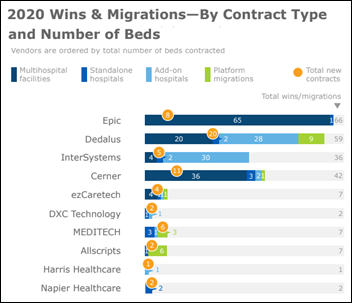
The private equity arm of Adu Dhabi Investment Authority acquires a minority stake in health IT provider Dedalus Holding.
Weight loss coaching app vendor Noom raises $540 million in new funding, valuing the company at $3.7 billion as it expands into stress management, sleep, diabetes, and hypertension. The company hopes to expand from individual subscribers, who pay $60 per month, to employers and insurers.
Sales
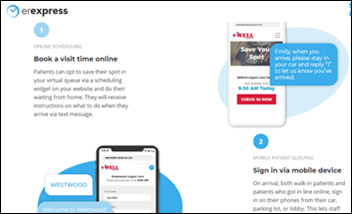
- MSU Health Care (MI) will implement Epion Health’s patient Check-In and Digital Screeners software.
- McLaren Health Care contracts with India-based HCL Technologies to deliver IT services to its 15 hospitals in Michigan and Ohio and create a global EMR Center of Excellence.
- Clinical management company SCP Health will expand its use of SOC Telemed’s Telemed IQ acute care telemedicine platform as it extends its telemedicine practice so it can offer both on-site and virtual care.
- US Orthopedic Alliance selects 2bPrecise’s precision medicine platform to identify drug-gene interactions.
- Colorado Center for Personalized Medicine will make the de-identified data of 7.3 million patients available to UK-based Sensyne Health, which will mine it and sell insights to drug companies, with revenue shared with CCPM. The company signed a similar deal with St. Luke’s University Health Network last week.
People

Tidelands Health (SC) family physician and Air Force veteran Gerald Harmon, MD will become AMA president next month.

Shelagh Fraser, MD (Priority Physicians) joins LifeOmic as its first CMO.

Jackson Hospital (AL) names Mark Lauteren (El Centro Regional Medical Center) AVP/CIO.

Tania Schade (Slalom Consulting) joins The Greeley Company, a division of The Chartis Group, as VP of business development.

Connect America hires Rosemary Kennedy (ECare Informatics) as chief health informatics officer.

Babylon names Darshak Sanghavi, MD (UnitedHealthcare) as global chief medical officer.

NextGen Healthcare hires Srinivas Velamoor, MBA (McKinsey) as EVP / chief growth officer.
Announcements and Implementations
Qardio implements Redox’s health data exchange API to enhance the interoperability of its remote patient monitoring solution.
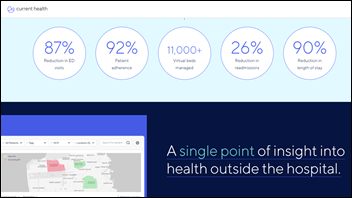
Geisinger Health System (PA) launches ConnectedCare365, a remote patient monitoring program for people with chronic conditions. The program’s technology comes from virtual care delivery startup Noteworth.

CareAlign offers free access to its task management system through the rest of 2021 for clinicians who sign up as beta testers.
Queen Anne County, MD will equip paramedics and EMTs with DrFirst’s Backline for EMS, which will allow them to scan a driver license barcode to confirm identity and retrieve a six-month medication history. It also allows them to exchange messages with local hospitals.
Other
Appointment-booking website Zocdoc fixes a software glitch that improperly allowed current and former employees of doctor and dental offices to access the patient data of 7,600 people via its provider portal. The company revealed similar programming errors in 2016.

St. Luke’s Health System in Idaho expands virtual emergency services to all nine of its EDs across the state. Patients will have access to virtual neurologists, behavioral health providers, pediatricians, social workers, critical care and nursing support specialists, plus emergency physicians and nursing teams through the system’s Virtual Care Center in Boise.
Cleveland Clinic seeks a digital health venture partner for its commercialization arm.
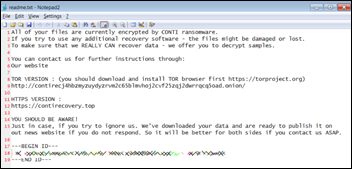
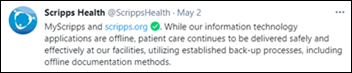
Scripps Health CEO Chris Van Gorder says the May 1 attack on the hospital’s computer systems was ransomware, and that its EHR and patient portal systems should be back up by the end of the week. He said the organization has kept quiet about the specifics of the attack to avoid copycat hackers: “Other attackers are already using what is being reported in the media to send scam communications to our organization.”
Sponsor Updates
- SCP Health expands its use of SOC Telemed’s technologies to include its Telemed IQ software for acute care.
- Ascom publishes a new whitepaper, “The high-reliability ICU.”
- Cerner’s Charitable Foundation honors 39 employees with Volunteer Impact Awards.
- The local paper profiles CoverMyMeds’ new $240 million headquarters, set to open in the coming weeks as the company begins bringing back its 1,500 workers.
- Diameter Health Software Architect Sam Schifman will present at the 2021 HL7 FHIR DevDays on June 9.
- Avtex publishes “Omnichannel Healthcare Experience Report 2021.”
- Meditech will convene its virtual “2021 Nurse Forum: Setting the Pace” June 16-18.
- KLAS recognizes Engage as a leader for its response to the COVID-19 crisis with a perfect score within the All Services Firms category.
- Ellkay recognizes Nuance EVP and GM Diana Nole as part of its Women in Health IT program.
- WHO Director-General Tedros Ghebreyesus will speak at the Everbridge COVID-19: Road to Recovery Executive Summit May 26-27.
- First Databank is included on Modern Healthcare’s “Best Places to Work in Healthcare” list.
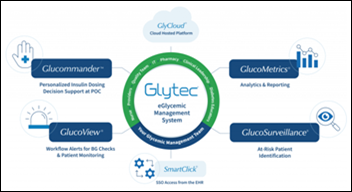
- Glytec releases a new video, “An Update in Glycemic Management in the Hospital: Impact and Lessons from COVID-19.”
- WebPT CEO Nancy Ham joins the HST Pathways Board of Directors.
- Georgia Hospital Health Services, a subsidiary of the Georgia Hospital Association, will promote Jvion’s All-Cause Readmissions product to member hospitals across Georgia.
Blog Posts
- How a SaaS-based scheduling system can help overcome the healthcare staffing crisis (Ability Network)
- “What About My Ovaries?” Part 2: The Paper Scanning Conundrum (Access)
- How to Bring Non-DICOM Imaging into Your Enterprise Imaging Strategy (Agfa HealthCare)
- Wildfire and Hurricane Preparedness: New PULSE Enterprise Features to Increase Flexibility and Scalability in Disaster Responses (Audacious Inquiry)
- OMOP Common Data Model: Build, Deployment, and Limitations (Bluetree)
- The Truth About Advanced Analytics: What Healthcare Leaders to Know (CereCore)
- Uber-izing the COVID Vaccination Experience (Change Healthcare)
- Role of the Healthcare CIO in Driving Digital Transformation (Divurgent)
- It’s Always Time to Switch for Value and Performance (EClinicalWorks)
- New Changes and Updates to Medical Decision-Making Guidelines from the AMA (Experity)
- “What About My Ovaries?”A Case Study Series Where It All Went Wrong – Part 1, Part 2 (Access)
- Back to Basics: HIPAA-Compliant Texting (Halo Health)
- Robotic Process Automation: An Essential Co-worker for the Digital Age (The HCI Group)
- Drive Better Outcomes with Four Data-Informed Patient Engagement Tactics (Health Catalyst)
- A Bite Size Update on Digestive and Metabolic Health IT (Healthcare Growth Partners)
- New Forrester study reveals COVID-driven Digital Identity issues and solutions (Imprivata)
- COVID-19 and the Biden administration jump-start policy focus on social determinants of health (Intelligent Medical Objects)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.























































































































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…