Download the printable PDF version of this guide to bring along to the conference here.
Access

Booth 2256
Contact: Lindsey Keith, sales and marketing operations manager
lindsey.keith@accesseforms.com
913.752.9938
One place. One view. ALL of your forms. Access develops electronic forms management solutions that eliminate the expense, risk, and inefficiency of paper forms. Our software, including Web-based Access Passport, enables organizations to capture, manage, sign and share e-forms data with other systems without paper, printers or scanners. Staff can interact with paperless e-forms anywhere, anytime using any device. Stamp your passport to paperless at HIMSS booth 2256 and learn more at www.accessefm.com.
AirStrip

Booth 4421
Contact: Jeaniene Outley, executive assistant
jeanieneoutley@airstrip.com
678.432.7813
AirStrip enables health systems to achieve interoperability with vendor- and data-agnostic mobile technology solutions for doctors, nurses, and other caregivers that seamlessly provide the engagement, collaboration, and insight required to care for others anytime, anywhere. AirStrip is the trusted champion for complete interoperability across all sources of health information throughout the continuum of care. HIMSS15 is the perfect opportunity to see how the AirStrip ONE mobile interoperability platform and solutions integrate disparate systems, data and devices, and eliminate barriers between technologies, people, and processes. Visit the AirStrip booth to discuss the technology you are using today. We’ll focus on your immediate needs as well as your plans for future innovation.
AirStrip will donate $1 for every badge scanned at the AirStrip HIMSS booth to a local Chicago charity. AirStrip is also running a #HIMSS15 giveaway on Twitter. Follow @AirStripmHealth to learn more.
AirWatch by VMware

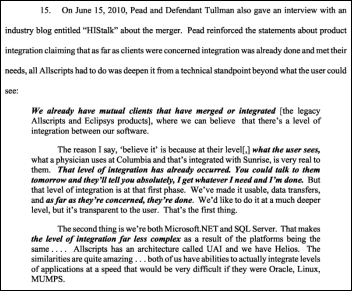
Booth 8164
Contact: Jeff Pool, director of healthcare solutions
jeffpool@air-watch.com
470.247.4041
AirWatch by VMware is the leader in healthcare mobility management, with more than 14,000 global customers. The AirWatch platform includes industry-leading mobile device, email, application, content, and browser management solutions. This year at HIMSS15 we have a demo station in our booth where you can meet with sales executives to get an overview of our solution. We also have a presence in the VMware booth (2268), featuring theater-style presentations and a separate demo area. Acquired by VMware in February 2014, AirWatch is based in Atlanta and can be found online at www.air-watch.com.
Anthelio Healthcare Solutions

Booth 7132
Contact: Andrea Watson, executive sales assistant/conference coordinator
andrea.watson@antheliohealth.com
214.257.7167
Anthelio is the largest independent provider of healthcare technology solutions. The company impacts quality care for over 6 million patients through its innovative solutions in the areas of IT, interoperability, EHR, HIM, patient engagement, and analytics. Stop by booth 7132 during HIMSS15 to learn about our cutting-edge solutions and shoot hoops with us!
We invite you to join Anthelio’s Casino Night for the ultimate HIMSS15 experience atop Willis Tower, the second-tallest building in the country. The breathtaking views, free drinks, cocktails, heavy hors d’oeuvres, appetizers, DJ, casino games, prizes, gift certificates, and much, much more await you … reserve your space early since capacity is limited. To RSVP, contact Andrea at andrea.watson@antheliohealth.com.
Aprima Medical Software

Booth 3020
Contact: Judy Friedman, marketing and events
jfriedman@aprima.com
847.800.2214
Aprima is unveiling its new Aprima NOW technology at HIMSS. This important new technology gives users greater functionality than ever before when viewing and managing patient data from their mobile and tablet devices. Thousands of providers have left their old EHR and made the move to Aprima. Aprima ranks among the top five vendors that physicians choose to replace their previous EHR. Here’s just a few reasons why:
- You’ll document patient visits with lightning speed.
- Aprima helps you navigate MU, ICD-10, PQRS, CQMs and more.
- More than 50,000 people already use Aprima.
- All customer support is US-based.
- Our customers tell us they can see more patients, enjoy improved financial performance and are able to spend more time with their families.
Aprima is one of the few companies with a 17-year track record of success. To learn more about Aprima, or for a demo of the Aprima NOW app, visit us at HIMSS in booth 3020 or visit www.aprima.com.
Arcadia Healthcare Solutions

Booth 7834
Contact: Greg Chittim, vice president, strategic marketing and business development
Greg.chittim@arcadiasolutions.com
781-202-3653
Arcadia Healthcare Solutions is an EHR Data Aggregation and Analytics technology company trusted by provider groups, health plans, and integrated delivery networks nationwide. Key events at HIMSS15 include:
- Monday, 4:30pm @ Booth 7834 – “Have a Sam Adams with Sam Adams” – join our SVP Sam Adams for an open bar, appetizers, and informative demos. Prizes to anyone who has a name joke that Sam hasn’t heard before.
- Monday, 6:30pm @ Palmer House Hotel – Healthcare Informatics Innovator Awards – Join longtime Arcadia client Carlos Olivares, CEO of the Yakima Valley Farm Workers Clinic, as he is honored as “Innovator of the Year.”
- Tuesday, 12:00pm @ Room S501-BC – “6 Things You Don’t Know About Your Patient … Because You’re Underutilizing EHR Data” – a Lunch and Learn sharing key insights and “a ha!” visualizations of populations and practices.
- Wednesday, 1:00pm @ Room S404 – “Bad Data’s Effect on Pop Health” – Join Bill Gillis, CIO at Beth Israel Deaconess Care Organization, as he presents the implementation and outcomes of an EHR Data Quality program.
Giveaway: Stop by our booth, 7834, for the chance to win an Apple Watch, Moto 360, or Fitbit Surge smartwatch.
Aspen Advisors, part of The Chartis Group

To schedule a meeting:
Contact: Dan Herman, information and technology practice leader
dherman@aspenadvisors.net
412.370.4900
Aspen Advisors is a top-ranked IT advisory services firm that works with leading healthcare organizations across the country to enhance care delivery, improve community health status, and achieve market distinction through the strategic and effective use of technology. In November 2014, Aspen joined The Chartis Group, a leading healthcare strategy consultancy, to deliver leading-edge capabilities in information technology in a way that is powerfully integrated with client strategy, clinical delivery, and evolving business models. Together, we provide healthcare providers with uniquely experienced senior healthcare professionals and consultants who apply a distinctive knowledge of healthcare economics, markets, clinical models, and technology to help clients achieve unequaled results.
Ultimately, our goal is to help you realize the value of your IT investments and continue to improve the effectiveness of your organization in improving the patient experience of care and the health of populations, while reducing the per capita cost of healthcare. Learn more at AspenAdvisors.net.
Billian’s HealthDATA

Booth 2045
Contact: Jessica Clifton
jlclifton@billian.com
678.360.9043
Billian’s HealthDATA and Porter Research offer unparalleled healthcare business insight and go-to-market research programs that help HIT firms and healthcare suppliers identify the best avenues to sell and market their products and services. Schedule your healthcare sales intelligence database demo by contacting jlclifton@billian.com or learn more at www.billianshealthdata.com.
Stop by booth 2045 on Tuesday, April 14, between 4:00 and 6:00 p.m. to learn more over complimentary cocktails and appetizers.
Capsule Tech

Booth 455
Contact: Brianna Roy, marketing and even specialist
briannar@capsuletech.com
978.482.2339
Capsule unlocks the power of medical device data to provide healthcare organizations with the critical patient and device information they need to provide safer, more efficient patient care. Its SmartLinx Medical Device Information System delivers connectivity, advanced integration, and analytics that turn volumes of patient data into relevant information.
Giveaway: Raffling off a Samsung Galaxy 4 Tablet
CareTech Solutions

Booth 7819
Contact: Lisa Kennedy, director of marketing and communications
lisa.kennedy@caretech.com
248.251.4539
CareTech Solutions is an information technology and Web products and services provider for U.S. hospitals and health systems, creating value for clients through customized IT solutions that contribute to improving the patient experience while lowering healthcare costs. From implementing emerging technologies to supporting day-to-day IT operations, CareTech offers clients expert health information technology services earning it the 2008, 2009, 2010, 2011, 2013 and 2014 Best in KLAS award for IT Outsourcing (Extensive), and the 2012 and 2013 IT Partial Outsourcing Award as ranked by healthcare executives and professionals in the respective annual “Best in KLAS Awards: Software & Services” report.
Come visit us at HIMSS15, booth 7819! We have your passport to healthcare innovation – everything you need to know to be successful in navigating the changes in the healthcare industry! For more information, please visit www.caretech.com/HIMSS15.
CenterX

Booth 4094
Contact: Christopher Marshall, COO
christopher@centerx.com
855.236.8379
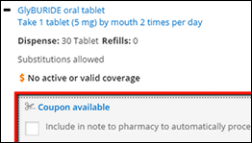
CenterX is a comprehensive e-prescribing network focused on improving patients medication adherence. CenterX offers advanced e-prescribing services, electronic prior authorization, clinically relevant prescription history, full clinical fax service, and clinical messaging and HISP services/CCD exchanges. CenterX works with prescribers, pharmacies, payers, and software vendors to create an open, efficient network that reduces cost and improves patient care.
Giveaway: Stop by booth 4094 to learn about CenterX, view a demo, and to pick up a swag bag, water bottle, pens and notepads.
ChartMaxx by Quest Diagnostics

Booth 1280
Contact: Vicki Joyce, ChartMaxx Marketing Specialist
Vicki.M.Joyce@QuestDiagnostics.com
513.204.2621
Coffee, Lattes and Actionable Insights. Visit ChartMaxx at Quest Diagnostics booth 1280 for your favorite barista java and learn more about how to transform your data into actionable insights with our ECM and BPM solutions.
Giveaway: Fill out a "Slice of the Windy City" game card and enter for a chance to win one of four Chicago prizes.
Clinical Architecture

Booth 2074
Contact: John Wilkinson, Vice President, Business Development
john_wilkinson@clinicalarchitecture.com
317.313.0013
Clinical Architecture is the leading provider of innovative healthcare terminology solutions. We develop software that evolves the way the healthcare industry overcomes challenges related to information; with a focus on improving quality, usability and reducing the burden on resources. We developed Symedical®, our comprehensive software suite, as a fully customizable platform for the acquisition, maintenance, and distribution of the terminologies you need. Let us show you how Symedical can provide the foundation for establishing and maintaining semantic interoperability.
Stop by booth 2074 to talk with one of our team members, enter to win our raffle, and check out our giveaways. For more information, and to schedule a time in advance to meet at HIMSS, visit: www.clinicalarchitecture.com.
Clockwise.MD

Booth 8191 Kiosk M-28 in the HX360 Innovation Pavilion
Contact: Michael Burke, CEO
mike@clockwisemd.com
404.271.8652
Clockwise.MD – a finalist in this year’s HX360 Innovation Challenge – improves the experience of waiting for care. Patients can make online reservations or appointments, and are kept informed of wait status via text message and a dashboard in the waiting area. During delays, patients can leave the waiting area and receive a message when it’s time to return. On discharge, patients review the facility via a text survey and are invited to share their experience on review sites. Come see us in the Innovation Pavilion, booth 8191, kiosk M-28.
CommVault

Booth 4873
Contact: Jay Savaiano, director, worldwide healthcare business development
jsavaiano@commvault.com
816.520.7367
Come learn how CommVault can turn your data into a valuable strategic asset. Our data storage and backup solutions can help you unlock data silos and put your data to work for you.
Giveaway: Enter to win an Xbox One with Kinect and a one-year Xbox Gold Live membership. Daily drawings, must be present to win.
CoverMyMeds

Booth 6027
Contact: Alison Bechtel, marketing manager
abechtel@covermymeds.com
614.300.1595
At HIMSS15 you will have the opportunity to speak with our experts on how CoverMyMeds automates the electronic prior authorization process for EHRs, PBMs and health plans, prescribers, and pharmacists. We are the only ePA vendor with all payer, all medication ePA functionality and we’d love to show you how it works. ePA National Adoption Scorecard talks will be held at booth 6027 Monday at 11:30 a.m. and 3:30 p.m. for EHR/Health Systems track and Tuesday at 11 a.m. and 2 p.m. for PBM/Plans track.
CTG Health Solutions

Booth 1580
Contact: Amanda LeBlanc, managing director, marketing and communications
Amanda.LeBlanc@ctghs.com
225.772.8865
Established in 1987, CTG Health Solutions, the healthcare business unit of CTG, is one of the largest providers of IT consulting services in the U.S. today with 600+ clients, and is dedicated to helping provider/payer organizations achieve their strategic, clinical, financial, and operational objectives by providing the highest quality clinical, business, and IT solutions. CTG (NASDAQ: CTG) is a publicly owned IT services and solutions company that generated revenue of $393 million in 2014. CTG Health Solutions will partner with IntrepidHealthcare to broadcast interviews—in a program called “#TalkHITwithCTG” – with many of today’s leading authorities on #HealthIT during #HIMSS15 (in our booth 1580, April 13 & 14) and then sharing the recorded version of these interviews after HIMSS.
Cumberland Consulting Group

To schedule a meeting:
Contact: Dave Vreeland, partner
david.vreeland@cumberlandcg.com
615.335.5272
Cumberland Consulting Group is a national information technology advisory, implementation, and support services firm serving the payer, provider, accountable care, and life sciences healthcare verticals. We specialize in providing technology implementation and project management support to help our clients advance the quality of services they deliver and improve their overall business performance. There will be several Cumberland representatives at HIMSS and we’d love to chat with you about your IT project needs. For more information on Cumberland, please visit www.cumberlandcg.com.
Direct Consulting Associates

To schedule a meeting:
Contact: Anthony Caponi, vice president of healthcare IT
acaponi@dc-associates.com
440.996.0863
Direct Consulting Associates (DCA) provides a broad range of IT consulting and staffing solutions including staff augmentation, temp-to-perm, and direct hire for enterprise and healthcare IT initiatives. Whether you’re an IT professional searching for that perfect opportunity or a client company looking for the very best IT talent you can trust, rely on DCA to help meet your goals.
Divurgent

Booth 1891
Contact: Keri DeSalvo, marketing manager
keri.desalvo@divurgent.com
757.213.6875
Divurgent will feature a fast-paced, interactive Trivia Charity Drive inspired by the explosively popular mobile app game, Trivia Crack. It will be hard to miss the vibrantly-colored Trivia Charity Wheel as HIMSS attendees spin to see what trivia category they will land on, along with what donation value Divurgent will contribute on the attendee’s behalf. Everyone is welcome to participate to help Divurgent meet its goal of raising $5,000 for Lurie Children’s.
Divurgent is a nationally recognized healthcare IT consulting firm, specializing in cyber-security and privacy solutions, population health management, clinical documentation improvement, and activation management and training. Visit booth 1891 to learn how Divurgent can help improve your operational effectiveness, financial performance, and quality of patient care. To view all of Divurgent’s exciting events and happenings during HIMSS, click here.
e-MDs

Booth 7832
Contact: Patrick Hall, executive vice president, business development
phall@e-mds.com
512.638.6966
E-MDs is a leading developer of integrated EHRs and practice management software for physician practices and enterprises. Founded and actively managed by physicians, the company is an industry leader for usable, connected software that enables physician productivity and a superior clinical experience. E-MDs software has received continual top rankings in physician and industry surveys including those conducted by the American Academy of Family Physicians’ Family Practice Management, AmericanEHR Partners, MedScape, and Black Book. E-MDs has a proven track record of positioning clients for success as demonstrated by Meaningful Use attainment in 2011, 2013, and 2014, and is currently rolling out Meaningful Use Stage 2-compliant solutions to clients. According to data provided by CMS, E-MDs clients are attesting in the top proportion of all major vendors. For more information, please visit www.e-mds.com, facebook.e-mds.com, and Twitter.com/emds.
ESD

Booth 2749
Contact: David Tucker, vice president of national sales
dtucker@contactesd.com
512.350.1735
Celebrating our 25th year in business, we pride ourselves on assisting healthcare organizations make the most out of their healthcare IT investments. Our team of clinical support professionals increases adoption and usability among clinical and physician teams by helping prepare, implement, and optimize your EHR systems. Stop by booth 2749 to discuss your goals and challenges. We would be happy to help!
Experian Health/Passport

Booth 2677
Contact: Cindy Dullea, chief marketing officer
cindy.dullea@passporthealth.com
703.802.1376
Experian Health and Passport provide the healthcare industry with a single platform that orchestrates every facet of the revenue cycle. Our integrated offering redefines efficiency with an exception-based workflow, Touchless Processing, and data and analytics to ensure unmatched payment certainty from patients and payers.
Giveaway: Visit booth 2677 and receive a Starbucks gift card—all while learning more about our Best in KLAS solutions to automate up to 80 percent of manual processes with intelligent automation.
Extension Healthcare

Booth 4408 / Intelligent Hospital Pavilion Booth 6656-23
Contact: Jenny Kakasuleff, PR manager
jkakasuleff@extensionhealthcare.com
317.345.4176
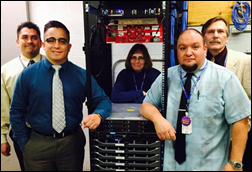
Extension Healthcare will exhibit in booth 4408, as well as part of the Intelligent Hospital Pavilion in booth 6656-23. Our main booth will feature:
Demonstrations of the new release of Extension Engage (v5). Recharging lounge with seating, multiple charging stations, and individual tablet demos. The first 250 visitors who "listen and learn" will receive their own ear buds and case. Grand prize drawing for visitors who fill out a short survey worth $500. Private room available to meet with an Extension Healthcare representative.
Our solutions will also be featured in Cisco Systems booth 2002.
Falcon Consulting Group

To schedule a meeting:
Contact: Brendan Downing, partner
brendan@falconconsulting.com
312.751.8900
Falcon Consulting is a comprehensive Chicago-based healthcare consultancy founded in 2010 that boasts a primary capability as a provider of Epic Systems implementation and support services. Falcon has experienced tremendous growth over the last three years and now deploys more than 130 consultants at 35 clients across the nation, serving in myriad capacities supporting a wide range of Epic applications and functions. Falcon recently pivoted its operating model by focusing on the acquisition of several operational experts from a market-leading Big 4 management consulting firm in an effort to continue driving value across all aspects of our provider organizations.
Falcon Consulting partitions its services into three main categories: Technology Services/Staff Augmentation, Professional Services, and Tools/Analytics. Our Technology Services team consists mainly of former Epic employees with market leading expertise, which is continually underscored by our outstanding client references. The Professional Services vertical focuses on strategy and operations across all areas of the provider organization- from Planning and Strategy to Performance Improvement. Lastly, our tools are developed internally to tackle the most complex issues that our clients have faced during our time on the ground. They are built to focus specifically on real issues with value driven results. It is Falcon Consulting’s mission to provide the highest quality consulting services that deliver industry leading value. We firmly believe in creating a partnership with our clients and generating a mutually beneficial relationship which, in the end, drives the best possible patient quality outcomes and financial sustainability.
Falcon has reserved a dedicated meeting room (MP7) to hold meetings with current and prospective clients. Please reach out to Brendan Downing (brendan@falconconsulting or 312-751-8900) if you would like to schedule time to hear about one of Falcon’s service offerings.
FDB (First DataBank)

Booth 2260
Contact: David Manin, director of marketing
dmanin@fdbhealth.com
650.872.4588
For HIMSS15, FDB (First Databank) has more than doubled its booth size (booth 2260) to share space with our sister companies – Zynx Health, MCG, and Homecare Homebase – under the Hearst Health network. FDB will highlight the following solutions: FDB Cloud Connector (FDB drug knowledge delivered though Web services); AlertSpace (for medication alert customization); MedsTracker (for medication reconciliation); Meducation by Polyglot (for patient medication adherence); Interoperability Module (for medication-related interoperability support); and OrderKnowledge (for medication ordering).
Giveaway: Stop by for a free cup of gourmet coffee!
FormFast

Booth 1538
Contact: Philip Blanks, marketing manager
pblanks@formfast.com
800.218.3512
Experience Higher Performance at FormFast Booth 1538! FormFast empowers hospitals by automating documents and workflow, capturing data and streamlining operations. FormFast’s productivity platform fills the gaps between different clinical and non-clinical hospital technologies. FormFast’s healthcare business solutions empower hospitals with actionable information and streamlined processes. By automating data capture and document workflow, we help hospitals achieve new levels of operational efficiency. This allows them to concentrate on their core mission – delivering quality care.
Giveaway: Come to booth 1538 and see FormFast’s productivity solutions; explore the innovative, evolutionary BMW i8; and win an all-expense paid trip for two to Las Vegas for a test drive.
Forward Health Group

Booth 5052
Contact: Barry Wightman, manager, media and communications
bmw@forwardhealthgroup.com
414.418.5654
Co-boothed with the American Heart Association and The Guideline Advantage, Forward Health Group will show off its powerful population health management toolset – PopulationManager. Highly ranked by KLAS, PopulationManager transforms chaotic data from disparate sources into valuable fuel, ready to identify and manage high-risk and/or high-cost patient populations, driving clinical outcomes improvement and financial success.
Giveaway: Stop by the booth and, if you’re really good, you’ll get a very cool LED flash light – shine a light on your data!
GE Healthcare

Booth 939
Contact: Chris Bowler, general manager, Americas region marketing
christopher.bowler@ge.com
860.620.3487
Visit GE Healthcare IT at booth 939 to learn how actionable insights can help you improve clinical, financial, and operational outcomes. Our 17 demo stations include solutions for financial management, population health, enterprise imaging, and care delivery management. And don’t miss our Augmented Reality Theater, where you can see firsthand how our software, services, and ecosystem help you spark success.
Giveaway: Enjoy fresh popcorn and a 35-foot-wide cinema experience.
GetWellNetwork

Booth 6627
Contact: Tony Cook, vice president, marketing
tcook@getwellnetwork.com
204.482.4212
Why come to our booth? Learn how our patient engagement solutions help healthcare providers engage, educate, and empower patients along the care continuum. Our patient-centered platform, delivered across mobile devices, computers, and televisions, enables providers to implement a care delivery model called Interactive Patient Care to improve performance and patient outcomes. The company extends the value of existing IT investments by integrating with EHR and patient portals. GetWellNetwork was named the category leader for Interactive Patient Systems for the fifth consecutive year by KLAS.
Giveaway: Visit our booth to learn more about GetWellNetwork and enter a drawing to win a FitBit Charge.
Greencastle Associates Consulting

To schedule a meeting:
Contact: Joe Crandall, director
crandallj@greencastleconsulting.com
856.685.0737
Greenway Health

Booth 1806
Contact: Ryan Grable, Director, Demand Generation
ryan.grable@greenwayhealth.com
813.202.5055
Get connected to Greenway Health at booth 1806 and discover innovation that helps you practice medicine your way. With 10 percent of ambulatory providers in the U.S. using our solutions today, we offer intuitive EHRs and other tools; clinical templates that rank as the best in the business; and robust population health, patient engagement, and revenue cycle solutions. We’re also leading the industry in exchanging clinical data. Ask how we can help you! Visit Greenway Health at booth 1806!
Hayes Management Consulting

To schedule a meeting:
Contact: Patty Kellicker, Vice President, Marketing
pkellicker@hayesmanagement.com
617-559-0404, Ext 249
Hayes Management Consulting partners with healthcare organizations to streamline operations, improve revenue, and enhance technology to drive success in an evolving healthcare landscape. We are different than other consulting firms – our consultants come from the frontlines of healthcare and not only understand the day-to-day challenges you face, but weave those realities into everything we do, which is why 75 percent of our clients come back for another project. Learn more at www.hayesmanagement.com.
The HCi Group

Booth 5155
Contact: Mitch Paine, executive vice president of business development
mitch.paine@thehcigroup.com
904.337.6320
At the HCi Group, we take pride in being a high-quality, value-driven provider for our clients. The HCi Group was founded on the principle that hospitals can have superior talent at reduced cost. We take a holistic approach to provide creative solutions and bring exceptional staff to our clients, ensuring the success of their initiatives. Many clients recommend the HCI Group as a result of our personal, prompt attention from leaders. The HCI Group forms working partnerships based on flexibility, responsiveness, and an entrepreneurial spirit. From the top down, our people will take on your project as our own.
Flexibility. The HCI Group produces highly creative and flexible solutions that will reduce risk and enhance outcomes. Quality. The HCi Group’s team of experienced professionals will consider every detail and go above and beyond to ensure success. Cost-effective solutions. Through collaborative planning and a lean business model, the HCi Group is able to target your pain points and offer comprehensive solutions at competitive rates, ensuring positive outcomes. We believe that selecting the HCi Group as your agile vendor partner will help to reduce the cost of implementing healthcare by delivering nimble, innovative solutions. And we prove it every day we go to work.
Health Care Software (HCS)

Booth 1709
Contact: Tom Visotsky, executive vice president, sales and marketing
tvisotsky@hcssupport.com
732.938.5600, Ext 325
The HCS Interactant platform is an enterprise solution that includes integrated clinical and financial modules that address regulatory and functional requirements for acute care, post-acute care, and behavioral health. Please visit HCS at booth 1709 to experience Interactant, our single platform solution that offers revenue cycle, financial management, EHR, and reporting and analytics capabilities.
Giveaways: Visit us for a demo and enter our drawing for a $250 American Express gift card. HCS is participating in the HIMSS LTC and Behavioral Health Task Force and will be giving away special gifts to LTPAC and behavioral health providers that visit our booth. We will also be hosting a night of baseball, beer, and burgers at the Brixen Ivy Rooftop overlooking Wrigley Field on Tuesday, April 14. In addition to fun, food, and HIT friends, we’ll be sending one lucky attendee home with a baseball autographed by Cubs Hall of Famer Ernie Banks. We invite LTPAC and behavioral health providers to contact us at tvisotsky@hcssupport.com or visit booth 1709 for details.
Health Catalyst

Booth 7545
Contact: Patty Burke, program manager
patricia.burke@healthcatalyst.com
208.861.5406
Click here to set up a meeting or a time to view a short demo and be entered for a chance to win a $100 Amazon Gift card. Or, simply swing by booth 7545 to say hello and meet our team.
Healthfinch

Booth 5273
Contact: Karen Hitchcock, director of marketing
karen@healthfinch.com
608.513.6566
Healthfinch makes Care Redesign applications that seamlessly integrate with the EHR to automate, delegate, and simplify the clinical tasks that are overwhelming physician inboxes. Our flagship product, Swoop (formerly RefillWizard), is used by major health systems to automate the prescription renewal request workflow. Using Swoop, organizations have dramatically decreased physician inbox tasks, saving over 1.5 million minutes of physician time. In addition to the time and efficiency savings, Swoop’s “care gap batching” feature identifies when patients are due for an office visit or diagnostic test. This proactive approach to patient care can be a critical component to quality improvement programs.
We invite HISTalk supporters to stop by the Healthfinch booth, 5273, at HIMSS. Meet our leadership team, including Lyle Berkowitz, MD a thought leader in #doctorhappiness, care redesign, and medical informatics. For those who schedule meeting times with us before April 11, we’re setting aside our limited edition Evolution of Care T-shirts, featuring Charlie, the happiest, hardest working healthfinch in the industry! See you there! (To book a specific meeting time and to reserve your T-shirt, please contact karen@healthfinch.com.)
Huron Healthcare

Contact: Casey Liakos
cliakos@huronconsultinggroup.com
608.234.9537
Huron Healthcare is the premier provider of performance improvement and clinical transformation solutions for hospitals and health systems. By partnering with clients, Huron delivers strategy and solutions that improve quality; increase revenue; reduce expenses; and enhance physician, patient, and employee satisfaction across the healthcare enterprise. Clients include leading national and regional integrated healthcare systems, academic medical centers, community hospitals, and physician practices.
Iatric Systems

Booth 7815
Contact: Judy Volker, marketing director
Judy.volker@iatric.com
978.805.3191
We hope you’ll stop by the Iatric Systems booth, #7815, at the HIMSS conference from April 12-16, 2015, in Chicago, and learn how we can help you get the right data to the right people at the right time. We also would love to discuss your upcoming needs regarding integration, patient privacy, medical device connectivity, the patient experience, Meaningful Use, HIE implementation, and any other healthcare IT requirements you may have.
Also, be sure to attend the educational session, "Stop Insider Snooping and Protect Your Patient Trust," April 14, 4:00 – 5:00 p.m. CT, room S406, presented by Marc Combs, AVP and assistant chief information officer, West Virginia United Health System; and Rob Rhodes, director of patient privacy, Iatric Systems.
Giveaway: Have some fun while you’re with us – we’ll show some thrilling GoPro videos, and you can register to win a GoPro Hero3+ Silver.
Imprivata

Booth 3848
Contact: Mark Erwich, vice president, marketing
merwich@imprivata.com
978.394.5595
Imprivata, the healthcare IT security company, is a leading provider of authentication, access management, and secure communications solutions. More than 1,200 healthcare organizations and 3 million end users globally rely on Imprivata’s solutions to improve provider productivity for better focus on the patient experience. At HIMSS15, Imprivata will showcase its portfolio of solutions, including:
- Imprivata OneSign, which delivers fast, secure No Click Access to EMRs, clinical applications, virtual desktops, and patient information.
- Imprivata Cortext, which enables secure, efficient communication and care coordination between providers across multiple healthcare organizations.
- Imprivata Confirm ID, which is the fast, secure signing solution for electronic prescribing of controlled substances.
In addition, Imprivata will feature a theater at its booth where customers will share their experiences and success stories using Imprivata solutions. Imprivata will have more than 35 presentations delivered by IT executives from hospitals and health systems providing details about their technology infrastructure, some of the challenges they faced, and how they are leveraging Imprivata’s solutions to address them. To pre-book a meeting with Imprivata, please visit http://www.imprivata.com/himss15.
Influence Health

Booth 3148
Contact: Anna Powell, vice president, marketing
anna.powell@influencehealth.com
205.982.5805
HIMSS15 is all about TRANSFORMATION at the Influence Health booth 3148 – from a platform that is transforming healthcare to a transformed name and booth. The Influence Health platform is the industry’s only integrated digital consumer engagement and activation platform. It is helping organizations transform healthcare by enabling providers, employers, and payers to positively influence consumer decision making and health behaviors well beyond the physical care setting through personalized and interactive multi-channel engagement. Since 1996, the Birmingham, AL-based company has helped more than 1,100 provider organizations influence consumers in a way that is transformative to financial and quality outcomes. For more information, please visit influencehealth.com.
InterSystems

Booth 961
Contact: Jerry Hinch, director of North American marketing
info@intersystems.com
800.753.2571
Be the first to know. Attend our new product announcement, Monday, April 13, 1:30 PM, for a revolution in patient engagement. InterSystems develops advanced software technologies that enable breakthroughs. With a passion for excellence and a focus on client success, InterSystems provides data management, strategic interoperability, and analytics platforms used in healthcare, financial services, government, and dozens of other industries. In selected countries, InterSystems also offers unified healthcare applications, based on these platforms, that deliver on the promise of connected healthcare. Founded in 1978, InterSystems is a privately held company headquartered in Cambridge, MA, with offices worldwide, and its products are used daily by millions of people in more than 100 countries. For more information, visit InterSystems.com/himss15.
Legacy Data Access

Booth 3455
Contact: John Hanggi, director
jhanggi@legacydataaccess.com
678-232-7922
Legacy Data Access has retired 163 different healthcare applications – a total of 362 healthcare applications! As a vendor-neutral archive provider, LDA has extensive experience in retiring numerous clinical applications including orders/results, nursing documentation, ancillary applications, and in many cases provides a Legal Medical Record for the stored data. Revenue cycle solutions include receivables functionality for earlier retirement of those applications. With a singular focus on the healthcare industry, Legacy Data Access stores data from applications – clinical, revenue cycle, ERP, ancillary, practice management and EHR – that are being retired and provides secure, Web-based access to the information. LDA’s solutions support financial and clinical processes and strategies by maintaining all detail, providing functionality based on your user requirements, improving productivity, and providing significant cost savings. If you are still running old applications just to get to the old data – we need to talk! We look forward to seeing you at our booth, 3455!
LifeImage

Booth 4674
Contact: Jackie Leckas, vice president, marketing
jackie@lifeimage.com
617.990.2262
Medical image exchange is gaining momentum as a must-have clinical capability. When physicians can easily access their patients’ external imaging histories, they can make faster, more informed decisions, and they also order fewer repeat imaging procedures. LifeImage provides a platform for medical image sharing that all of the ‘ologies in the healthcare enterprise can leverage to send and receive imaging, and import it to local systems. We also integrate with Epic and Cerner to make outside exams easily available to care providers who are already working in the EHR. Visit our booth at HIMSS to learn about adopting image exchange at your organization.
Giveaway: All booth visitors will take home a mobile phone power bank to ensure their devices stay powered up during their Chicago travels.
MEA I NEA

To schedule a meeting:
Contact: Christine Alfano, senior director of corporate and product marketing
christine.alfano@nea-fast.com
813.532.0059
MEA|NEA will conduct meetings at HIMSS with healthcare clients and partners interested in streamlining their revenue cycle via electronic claim attachment processes. CEO Lindy Benton will be on-hand, as well as Chief Development Officer Kent McAllister, VP of Sales Scott Hefner and Senior Director or Corporate and Product Marketing Christine Alfano. Our team would love to meet with you. To schedule an appointment, please contact christine.alfano@nea-fast.com and let us know your area of interest.
medCPU

Booth 108
Contact: Yoni Ben-Yehuda
ybenyehuda@medcpu.com
MedCPU delivers accurate, real-time, enterprise decision-support software and services through its proprietary Advisor technology. MedCPU captures the complete clinical picture from clinicians’ free-text notes, dictations, discharge summaries, and structured documentation entered into any EHR, and analyzes it against a growing library of best-practice content, generating real-time precise prompts for best care consideration. MedCPU’s founding multi-disciplinary team has been pioneering new clinical decision support for nearly 20 years, delivering intelligent error-reduction software systems to hospitals across the United States. MedCPU’s applications include clinical and compliance support solutions. Visit booth #108 to see the future of decision support today!
MedData

Booth 4851
Contact: Chris Farrell, vice president of marketing
chris.farrell@meddata.com
440.627.2642
MedData is a leading national provider of revenue cycle management and patient financial lifecycle solutions, including billing, coding, collections, and patient satisfaction. We’ve provided innovative billing solutions to the medical community across a variety of specialties since 1980.
Giveaways: Stop by our booth for freshly baked scones, Operation challenge, and daily drawings for an Amazon gift card.
Medhost

Booth 1817
Contact: Tom Mitchell, vice president of marketing
tom.mitchell@medhost.com
615.761.2011
Medhost is a provider of market-leading enterprise, departmental and healthcare engagement solutions to approximately 1,000 healthcare facilities. Our healthcare management system includes intuitive, easy-to-use and SaaS-enabled solutions, including YourCareUniverse, a comprehensive suite of cloud-based patient and provider engagement applications. Our robust offering of managed hosting, outsourcing and consulting services that are changing how clinicians and hospital leaders work and communicate, while generating notable operational, patient flow, care and revenue improvements. MEDHOST delivers value by enabling hospitals of all types and all sizes to better manage care and the business of healthcare while meeting evolving regulatory requirements.
Medhost will promote release of YourCareUniverse in our booth. YourCareUniverse, Inc. provides a comprehensive, integrated, cloud-based solution for managing the digital patient and supporting the consumer in a way that enables a healthcare organization to be the trusted source of health information and services within their community. Part of YourCareUniverse, we will also be highlighting YourCareEverywhere, a health and wellness site that provides medical information and localized branding for hospitals. We encourage all providers to come take a test drive of YourCareEverywhere. YourCareUniverse will also be highlighted in the Interoperability Showcase as part of a connected demonstration use case featuring the YourCareHealth portal.
Additionally, MEDHOST will be providing demos on our Physician Experience solution which provides charting, noting and the important orders management in a workflow that is natural to physicians. Other demos include our Emergency Department Information System, our Perioperative solution and AHA-endorsed Patient Flow application.
Medicity

Booth 3431
Contact: Lauren Tilelli, director of marketing
ltilelli@medicity.com
770.633.9013
Medicity, a Healthagen business, powers clinically integrated networks for over 100 organizations, which together have more than 1,000 hospitals and 250,000 end users. Its core solutions for real-time care coordination, population health analytics, and leakage and steerage empower clients to achieve accountable care goals while advancing population health today and tomorrow. As the healthcare industry transitions to value-based care, large organizations and independent practices alike are challenged to implement solutions that provide the data and integrated workflow tools needed to meet their population health goals. This will be Medicity’s focus at HIMSS2015, as it shares its latest developments to help organizations identify high-risk populations, meet Meaningful Use objectives, improve patient outcomes, and reduce cost of care.
We can help you: identify and reduce leakage while growing market share; gain a full historic view of each patient in your population in seconds instead of days; alert providers and care managers when patients are admitted to, or discharged from, a health care facility; and quickly and securely engage providers and communicate across care settings.
Medicomp Systems

Booth 2318
Contact: David Lareau, CEO
info@medicomp.com
703.803.8080
Lights, camera, action! Let’s play Quipstar! Back by popular demand, Medicomp Systems invites you to play Quipstar, the World’s Favorite HIT Quiz Show. Medicomp will show the live studio audience why doctors love Quippe, an easy-to-use documentation tool that works with your existing EHR, and that saves doctors time so they can see more patients. Contestants selected from the studio audience (this could be YOU!) will compete against popular HIT stars like Jacob Reider, MD Ross Martin, MD and Lyle Berkowitz, MD for cash and prizes.
Giveaways: At each show we’ll give away 10 (yes, 10!) iPad Air 2s, cash, and prizes. Only two shows daily so register now at www.medicomp.com/histalk.
Nordic

Booth 1699
Contact: John Pollard, senior director of marketing
john.pollard@nordicwi.com
608.358.6600
Nordic is the world’s largest Epic consulting practice. Since 2012, Nordic has been ranked #1 by KLAS for providing Epic EHR consulting services to healthcare organizations. You can find Nordic at booth 1699. Look for the green Nordic banner just down the aisle from Epic. To make sure the right experts are available when you stop by our booth, we’ve set up “office hours.” We’ll discuss population health, a variety of ROI-based approaches to Epic optimization, dealing with mergers and acquisitions, guiding you through health IT complexity, and saving money on maintenance and support daily. View the hours at Nordicwi.com While we’ll be sure to have specialists available during these times, we welcome you to arrange a time to discuss any of your Epic-related projects or challenges. Simply contact your Nordic representative or write events@nordicwi.com. We’ll be sure to make time for you!
NTT Data

Booth 3943
Contact: Larry Kaiser, senior marketing manager
lawrence.kaiser@nttdata.com
310.301.1284
NTT DATA offers healthcare organizations a complete IT solution with applications that increase efficiency, reduce medical errors, and enhance the revenue cycle. Led by our flagship solution, Optimum, NTT DATA helps bring together healthcare consumers and providers to share data and manage care effectively. We back that engagement process with a full range of clinical, RCM, accounting, and mobile solutions. NTT DATA will be promoting our complete hospital HIS at HIMSS.
NVoq

Contact nVoq (sales@nvoq.com) at HIMSS to learn more about SayIt, a true cloud-based speech recognition solution that converts speech to text within seconds. It also supports command and control through voice, or through voiceless “pop-up” shortcuts. NVoq will sponsor a Snack Hour in the HIStalk booth, 5371, on Tuesday, April 14 from 2-3pm CT. Stop by for Garrett’s popcorn and collectible lapel pins!
Oneview Healthcare

Booth 7330
Contact: Jeff Fallon, president, North America
jfallon@oneviewhealthcare.com
724.720.9389
The Oneview Healthcare patient engagement and clinical workflow solution is the most innovative interactive patient care system on the planet. Visit out booth to see why hospitals on four continents choose our platform to improve patient satisfaction, enhance outcomes and increase efficiencies.
Orion Health

Booth 4435
Contact: Sam Rosenbaum, senior marketing manager
sam.rosenbaum@orionhealth.com
857.301.2898
All attendees who schedule a meeting prior to HIMSS with Orion Health will have a donation made on their behalf to Alex’s Lemonade Stand Foundation For Childhood Cancer and be entered to win one of five Apple Watches. (Note: they will be shipped post-HIMSS as the release date is April 25.) Attendees can request a meeting by visiting www.orionhealth.com/himss/.
Park Place International

Booth 6015
Contact: Christine Mellyn, Director of Marketing
781.636.8169
Patientco

Booth 3639 in the Georgia Pavilion
Contact Josh Byrd, director of marketing
josh.byrd@patientco.com
404.444.2929
Patientco is the leading provider of cloud-based patient revenue cycle technology that empowers providers to optimize payments and increase business office efficiency through consumer-centric technology. Patientco goes beyond basic payment capture to connect every patient payment event throughout a healthcare system — delivering unrivaled visibility into and control over the patient revenue cycle. The result is improved cash flow, reduced A/R days, cost-saving efficiencies, and increased patient and provider satisfaction. For more information, visit www.patientco.com.
This year, we are a sponsor of the Revenue Cycle Innovation Task Force (RCITF) Event at HIMSS. The task force findings will be presented in a brochure that can be picked up at the Patientco booth, 3639. We are located in the Georgia Pavilion.
PatientKeeper

Booth 3212
Contact: Kathy Ruggiero, senior director of corporate marketing
kruggiero@patientkeeper.com
617.899.6521
PatientKeeper provides more than 60,000 physician users at hospitals and practice groups an intuitive way to view and act on patient information. PatientKeeper applications for order entry, med rec, documentation, charge capture, and other physician workflows run on desktop and laptop computers, smartphones and tablets, and integrate with existing IT infrastructure. Using PatientKeeper helps providers improve patient care, migrate smoothly to ICD-10, and achieve sustained Meaningful Use.
Giveaways: Visit the "PK Cafe" at PatientKeeper’s booth (3212) for a refreshing coffee or smoothie drink.
PDR

Booth 5225
Contact: Kimberly Koss, senior operations manager
kimberly.koss@pdr.net
314.567.0551
PDR is a trusted healthcare communications company providing targeted, clinically relevant information to Prescribers, Pharmacists, Payers, and Patients to improve health outcomes. PDR products and services integrate seamlessly within workflow in an effort to educate healthcare providers and impact prescribing behavior through access to information for better health. Reach over 300,000 contracted prescribers and 250,000 deployed prescribers within workflow by leveraging PDR’s proprietary business rules engine, a system that processes nearly 1 billion healthcare transactions annually.
PDR’s behavior-based messaging system is customized based on the specific actions providers take within their e-prescribing tool during patient encounters. The flow of information does not stop when the exam room door closes. PDR’s suite of professional educational tools now ranges beyond the education of healthcare providers to the education of their patients, providing resources that are certified to support Meaningful Use requirements and motivate patients to achieve medication adherence.
PerfectServe

Booth 7439
Contact: Tom Hills, executive vice president, sales
thills@perfectserve.net
877.844.2777
PerfectServe is a comprehensive communications and collaboration platform that provides a secure infrastructure uniting physicians, nurses and other care team members across the continuum. PerfectServe goes beyond secure text messaging to offer multimodal access and interoperability, minimizing your HIPAA-compliance risk and enhancing your EMR investment. Visit us in booth 7439 to learn how healthcare organizations can address the widest variety of communication workflows across all stakeholders, which drives maximum clinician adoption and results in meaningful quality and operational improvement. Plus, we have candy! To learn more about PerfectServe, visit perfectserve.com.
Phynd Technologies

Booth 2084
Contact: Thomas White, CEO
twhite@phynd.com
855.749.6363, Ext 710
The Phynd Provider Information Platform is a solution for poor provider data in the EHR and other systems. Phynd enables health systems to quickly and seamlessly integrate, manage, enroll "new" provider and analyze change data. With Phynd, hospitals improve revenue cycles, clinical communication, and productivity associated with managing provider data within multiple departments. At HIMSS, Phynd is part of the Interoperability Showcase with the leading EHR vendors and other related systems.
Porter Research, a Billian Company

Booth 2045
Contact: Cynthia Porter, president
cynthia@porterresearch.com
678.427.6241
Porter Research and Billian’s HealthDATA offer unparalleled healthcare business insight and go-to-market research programs that help HIT firms and healthcare suppliers identify the best avenues to sell and market their products and services. Learn more by contacting cynthia@porterresearch.com or visit www.porterresearch.com.
Stop by booth 2045 on Tuesday, April 14, between 4:00 and 6:00 p.m. to learn more over complimentary cocktails and appetizers.
Sagacious Consultants

Booth 1690
Contact: Jesse Adams, executive vice president
jesseadams@sagaciousconsultants.com
210-882-9658
Sagacious Consultants is your full-service business partner, leveraging technology to drive financial performance and improve patient care. Our strategic services help healthcare organizations increase revenue, decrease denials, and reduce AR days. Visit Sagacious Consultants at HIMSS booth 1690 for a chat with some of the EHR industry’s smartest leaders, including Founder and CEO Shane Adams and Principal Consultants Gordon Lashmett, George Evans, and Dr. Ron Jimenez. With experience as Epic CIOs and directors of clinical informatics, they will be available to offer advice about your most pressing technical and operational challenges.
Giveaway: Pick up some Sagacious swag while you’re visiting.
Sagacious Consultants will be rocking HIStalkapalooza as a Gold Sponsor. Invited guests can strut like rock stars on a red carpet at the House of Blues, grab a guitar or banjo prop, and strike a pose. Don’t leave without taking home a Sagacious rock poster commemorating this star-studded night for HIT.
Sandlot Solutions

Booth 2641 & 2939
Contact: Lisa Verrecchia, marketing director
lverrecchia@sandlotsolutions.com
800.370.1393
Sandlot Solutions is a leading provider of clinical interoperability and community health management solutions focused on the exchange of clinical and claims data across the care community, population data analytics, and enhanced care coordination. Sandlot provides the tools and technology that enable healthcare organizations to improve the quality of care, understand and manage risk, reduce costs, and transition to new business models.
Giveaways: Sandlot Solutions is offering a tiered giveaway at HIMSS15. More interactions equals eligibility for higher-value prizes.
1st Tier Prize: Enter for a chance to win your choice of $100 Amazon Gift Card or iTunes Gift Card
2nd Tier Prize: Enter for a chance to win an iPad mini
3rd Tier Prize: Enter for a chance to win a Surface Pro 3
Interactions include a badge swipe at either of the Sandlot booths, a product demo at the main Sandlot booth (2641), and market research at the Sandlot attractor booth (2939).
Santa Rosa Consulting

Booth 2641 & 2939
Contact: Ashley Burkhead, sales operations and marketing manager
ashleyburkhead@santarosaconsulting.com
972.804.4216
Santa Rosa Consulting is offering a tiered give-away at HIMSS15. More visits equals eligibility for higher-value prizes.
Tier 1: Visit booth 2641 or Fortified Health Solution’s kiosk in the Cyber Security Command Center and be entered for a chance to win a $100 Amazon Gift Card.
Tier 2: Visit both booth 2641 AND our Fortified Health Solution’s kiosk in the Cyber Security Command Center and be entered for a chance to win your choice of an iOS or Android tablet valued at $500.
Tier 3: Visit both booth 2641, Fortified Health Solution’s kiosk at the Cyber Security Command Center AND participate in a Fortified Health Solution demo and be entered for a chance to win a LED TV of your choice valued at $700.
Sunquest Information Systems

Booth 923
Contact: Ajay Kapare, director, marketing
Ajay.kapare@sunquestinfo.com
520.570.2868
Talksoft

Booth 4390
Contact: Eric Pearlman, director of business development
epearlman@talksoftonline.com
866-966-4700
Founded in 1997, Talksoft is an applications service provider (ASP) of reminder and notification services using phone, text, email, and mobile app. Talksoft’s service-based approach provides affordable solutions for businesses of any size. Subscribers pay only a usage-based fee – there are no long-term contract commitments, and no computer hardware purchases. For more information, call (866) 966-4700 or visit talksoftonline.com.
TeraMedica

Booth 3239
Contact: Robin Schroeder-Janonis, vice president of sales
sales@teramedica.com
414.908.7719
TeraMedica is proud to be named the 2014 KLAS Category Leader for VNA/Image Archive. At HIMSS15, we are pleased to introduce our powerful analytics platform and dashboards. The new analytics platform takes advantage of existing customized, role-based dashboards. These dashboards support interactive reporting with dynamic data filtering and trending analysis across categories. Featuring one-click statistical data summaries and forecasts, the enhancements increase user productivity and insight. Complementing our VNA’s new user interface, the solution simplifies data management, access, and quality assurance.
Valence Health

Booth 5073
Contact: Kevin Weinstein, chief growth officer
kweinstein@valencehealth.com
312.273.6623
Valence Health provides value-based care solutions for hospitals, health systems, and physicians to help them achieve clinical and financial rewards for more effectively managing patient populations. Leveraging 20 years of experience, Valence Health works with clients to design, build, and manage value-based care models customized for each client including clinically integrated networks, bundled payments, risk-based contracts, ACOs, and provider-sponsored health plans. Providers turn to Valence Health’s integrated set of advisory services, analytical solutions, and managed services to make the volume-to-value transition with a single partner, in a practical and flexible way. Valence Health’s 600 employees empower 39,000 physicians and 130 hospitals to advance the health of 20 million patients. For more information, visit www.valencehealth.com.
Giveaway: Come visit us at HIMSS in booth 5073 for a demonstration of our newly enhanced population health technology solutions, and register to win a free Valence Health value-based care readiness assessment. The winning organization will work closely with our subject-matter experts to evaluate your healthcare IT capabilities as they relate to enhancing care outcomes and optimizing rewards for quality.
Versus Technology

Booth 2053
Contact: Stephanie Bertschy, director of marketing
info@versustech.com
231.946.5868
Move over EMR – it’s time for REAL-TIME automation! Manual data entry is so old school. The Versus real-time locating solution (RTLS) is the “engine” needed today to drive automated processes, increased access to care, and enhanced patient experiences. Take your own test-drive at HIMSS15 – Versus offers the only live RTLS demonstration on the exhibit floor. Our Experience Center features a fully operational Versus Sensory Network, demonstrating real-time updates in clinical workflow. Learn how we use location data, combined with powerful workflow intelligence, to not only drive efficiency at the point of care, but also automatically document key performance measures – helping you measure and manage your operations. Plus, be one of the first to see our new Clearview Net Badge and Asset Net Tag, featuring Versus’ accurate, patented infrared (IR) technology in combination with CCX Wi-Fi locating. With five clients presenting four educational sessions at HIMSS, we also offer ample opportunity to speak with real RTLS users. From asset tracking to patient flow process improvement, systems integration and hand hygiene monitoring, we’re sure to put you in touch with a peer who can offer insight into your own initiatives. Real hospitals, real clinics, real surgery centers rely on Versus as their partner for process improvement. Come to booth #2053 to put yourself in the driver’s seat and learn why.
Giveaway: The first 100 visitors to mention HISTalk will receive our collectible HIMSS15 blinky pin.
VisionWare

Booth 7139
Contact: Julie Bastien, marketing director
julie.bastien@visionware.com
508.449.4360
Meet the VisionWare team and find out what makes us the leading provider of master data management (MDM) solutions for hospitals, health systems and healthcare technology companies. We’ll walk you through a demo and show you how our solution ensures the success of our customers’ population health, big data, and patient engagement initiatives by providing a single source of truth across an enterprise. We enable multiple source systems to exchange data easily and empower decision-makers with a holistic view of their patients, providers or system as a whole. We look forward to seeing you at booth 7139!
Giveaway: Visit the VisionWare booth and have your personal caricature drawn by our onsite artists. You can wear it proudly around the halls of HIMSS or make it your new profile picture!
WeiserMazars

To schedule a meeting:
Contact: Marc Grossman, principal
marc.grossman@weiermazars.com
516.641.4210
Wellsoft Corp.

Booth 1742
Contact: Denise Helfand, vice president, sales and marketing
dhelfand@wellsoft.com
800.597.9909
Consistently ranked #1 Emergency Department Information System (EDIS) by KLAS, (most recently awarded Best in KLAS 2014), Wellsoft EDIS offers an exceptional combination of experience, extensive workflow analysis, and award winning customer support. Wellsoft EDIS is certified for Meaningful Use. Software features include patient tracking, clinical documentation, CPOE/results, charge capture including infusion charge capture, risk management and CCD document exchange. Wellsoft is EDIS at its BEST! Visit Wellsoft at booth 1742 for a brief demonstration and to discuss how Wellsoft EDIS fully integrates with HIS and ancillary systems, AND can help with your roadmap to Meaningful Use attestation.
Wolters Kluwer Health

Booth 8103
Contact: Alyssa Lamoreaux, director of communications
alyssa.lamoreaux@wolterskluwer.com
612.313.1510
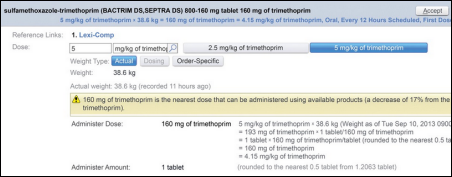
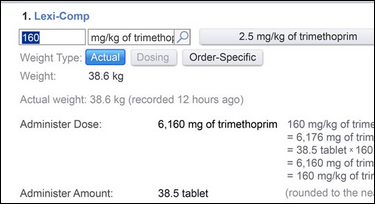
A leader in point of care information, Wolters Kluwer Health Clinical Solutions provide best-of-breed offerings focused on improving the quality of care and driving clinical productivity. Hospitals, ASCs, physicians offices, payers, labs and retail pharmacies turn to us as their trusted partner for the content and tools they rely on every day. From clinical documentation, to clinical drug information, to clinical informatics and surveillance, to clinical decision support, our products deliver meaningful solutions clinicians value. Facts & Comparisons, Lexicomp, Medi-Span, ProVation Medical, ProVation Order Sets, Sentri7, Health Language & UpToDate.
Xerox

Booth 4426
Contact: Kirsten LeMaster, VP, marketing and communications, healthcare provider solutions
hcprovider@xerox.com
877.414.2676
Today’s Xerox simplifies the way work gets done in surprising ways. Like supporting healthcare professionals in over 1,900 hospitals. With consulting services, Midas+ analytics and adoption solutions from The Breakaway Group, A Xerox Company, we help healthcare providers apply, manage and use technology that simplifies caregiver workloads. So you have more time to focus on delivering the level of care everyone deserves.
Heather Haugen PhD, CEO of The Breakaway Group, a Xerox Company, will host a HIMSS session, “Beyond Implementation: Achieving Value from Your EHR after Implementation,” on April 15 at 8:30 a.m. in room S103 (Session ID: 33)
Giveaway: There will be a caricature artist in our booth drawing attendees that stop by our booth during exhibit hall hours.























































































































































































































The New Yorker cartoon of Readers Write articles.