Curbside Consult with Dr. Jayne 7/6/20

I survived the Independence Day weekend in the emergency department trenches without seeing anyone who had finger or eye injuries, so it was a good one.
I didn’t get to see any fireworks or have popsicles, but the PPE fairy paid me a visit. I’m happy to report that exactly four months after seeing my first positive COVID-19 patient, I finally have an honest-to-goodness actual 3M healthcare N95 respirator, as opposed to a non-medical version from the hardware store. To be precise, I have two of them. Which I’m supposed to rotate indefinitely.
Excuse my cynicism, but I’m not exactly sure what the US has to celebrate today. The actions of our fellow citizens exercising their freedom to not wear masks and their freedom to congregate in large groups is sending patients to the hospital, if not to their graves. Our testing volume is up by about 20%, but our positive case rate is nearly triple what it was recently, so we’re gearing up for a bumpy ride.
Our group has moved into testing entire cohorts of workers from various employers, which is straining resources. The first bolus of patients came from a hair salon, where they are meticulously separating clients with plastic barriers and stylists and clients are all masked. Unfortunately, the 20-somethings who work there all huddle up in a break room together between clients with masks off, or stand outside the door smoking, so close to 80% of them came back positive. No surprises there.
The next set of workers came from a country club, where even though the dining area has been moved outside, servers are still in close contact with patrons. The wait staff also had a communal break area, and frequently took masks off in between runs to the dining area. Now everyone gets to hang out at home for 14 days waiting for tests to come back. Unless something changes with our reference lab, there’s a good chance we’ll be clearing them based on time before their results come back — the lab’s turnaround time has skyrocketed to 10 days.
At this point, I truly wish my EHR had the capability to do a standard visit that could be copied from patient to patient. Although we have some templates for physical exams, everything else has to be keyed from scratch for each patient unless they’re a returning patient. I’d love to be able to bulk-copy these HPIs since they’re essentially the same. “Patient presents for employer-mandated testing, was exposed to a patient over the last two weeks who is now positive. Patient reports non-masked interactions at close range in a common break area and sharing of plates of food by co-workers.”
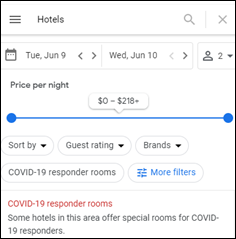
You might ask why I’m writing an HPI when the patient is just there for testing. Our new reality is that payers have gotten burned by the “sure, we’ll pay for COVID-related visits” policies and are now requiring documentation of medical necessity to support payment for testing. I thought this article from mid-June was over the top until I started experiencing “concern” from payer reps about our testing patterns.
As much as everyone is focusing on the struggles of the hospitals and the potential for overwhelmed ICUs, ambulatory practices (especially independent ones) are really struggling right now. Many are not performing testing because of lack of PPE and we’re still challenged to keep patients safe. Unlike larger facilities, small offices don’t have the luxury of being able to set up dedicated respiratory clinics within their footprint or to offer separate waiting areas for suspected COVID patients. The best they can do is to try to separate patients temporally, bringing in the well patients in the morning and sicker patients as the day progresses.
Many of my colleagues in this situation are using automated screening solutions to try to risk-stratify patients the day before, although the system isn’t perfect. For example, one of my patients who came in for food poisoning recently was actually COVID. It’s hard to triage that without doing a full telehealth visit up front.
I get a lot of direct to doctor emails from tech companies, and I’m surprised by the silence from the companies that have sanitizing technologies. There seemed to be dozens of booths at HIMSS for solutions to sanitize laptops and keyboards and otherwise keep technology clean. If anyone is in that space, I would be interested to see what business looks like right now and if you’re just overwhelmed or how things are going.
The push for telehealth technologies has also slowed. It feels like practices that jumped into the pool with Zoom or other non-healthcare solutions are starting to transition to telehealth solutions that are embedded in their EHR or otherwise integrate. I agree that expecting clinicians to work in two systems is daunting and no one wants to do it for long.
There used to be several players in the hand hygiene market. What’s going on in that space? Are hospitals going high tech to monitor staff compliance, or are they running out of money and worried about taking care of the basics? Any action on expansion of robotic healthcare assistants to reduce the need for humans to go in and out of exam rooms?
It seems like there are so many interesting technologies with potential, but I struggle to keep up with how other organizations might be innovating because I’m simply swamped seeing patients.
I hope that readers had a chance to recharge at least a little this weekend. Many people had Friday off in honor of the holiday or had modified work schedules. In many states where cases are rising, this is just the beginning of a long slog.
How is your organization helping workers recharge their batteries, or making sure they are holding up OK under the stresses of our new normal? Have you instituted new technologies to try to make an impact? What about the addition of recharge zones or stress reduction rooms? Leave a comment or email me.
Email Dr. Jayne.























Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…