Jonathan Davis is founder and CEO of Trualta of Ottawa, ON.

Tell me about yourself and the company.
I started Trualta about six years ago. I was investing in healthcare education companies that provided training, continuing education, and certification for healthcare professionals. It dawned on me that there were so many great best practices for caring for loved ones, especially aging loved ones, that families didn’t have access to. For example, why did an aide in a nursing home know how to manage a particular symptom of cognitive decline, but a family member didn’t?
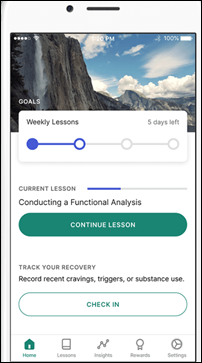
That inspired me to think about how we could adapt professional-level training to the families who need it most. That was the start of Trualta. We built a caregiver education platform with articles, videos, and modules to help families build skills and establish confidence to provide care at home.
Right away, we started working to demonstrate that trained, confident family members can provide better care at home. By proving those outcomes, we could partner with governments, payers, and providers to offer Trualta for free to caregivers. We always believed that the caregiver shouldn’t pay for support. We know caregivers are often already facing unexpected costs.
Since then, the business has grown to offer not just caregiver training and support, but also community and coaching.
People don’t always know in advance that the caregiver role is about to be placed on them. What is the most common training and support they need?
That’s very true. Many caregivers don’t even self-identify as caregivers. The training and support that is most effective is a mix of topics related to the caregiver’s own wellness and how to manage this often unexpected, challenging care situation. We personalize our content to the caregiver’s unique care situation and the conditions they manage at home for their loved one. At the end of the day, all caregiving journeys are different. We anchor on the training outcome. We want our caregivers to feel more confident and less alone, which we know leads to better care for the patient, the loved one they are caring for.
What is the blend of people, technology, and support that makes it possible to successfully send patients home for care?
On the technology side, we’re all about finding the right support for the right caregiver at the right time. Maybe it is post-surgery. Let’s say Mom or Dad got a hip replacement. We know that individual care situation and can target the caregiver with specific content. For example, a common reason for readmission might be a UTI or a bed sore.
Where the technology and the tech-enabled community and coaching come in is that we start to understand how the caregiver is feeling. They’re a bit lonely and isolated, providing care 24/7 for their partner who is recovering at home. We know that they would benefit from a support group, so we direct them to one. It is a virtual, tech-enabled support group, but it is facilitated. To us, that’s a healthy mix of technology and people. If the care situation escalates and we see a high risk of caregiver burnout, we can route that person to a one-on-one coach.
A national challenge is the large number of baby boomers who will eventually need care, but with fewer people to care for them. How will that play out?
This is such a tough problem on both the demand and supply sides. On the demand side, we have this aging population. Folks are also living longer, with a higher likelihood of certain chronic conditions or cognitive decline. We know that older adults prefer to age in place. Then we have government policy promoting home and community-based settings instead of the institutional setting.
Demand is way up, but there’s an acute workforce shortage, so supply is also down. That market dynamic is putting so much on the family members. It’s more important than ever that our healthcare stakeholders support families and people who care for loved ones at home with skills, community, support services, and coaching.
How do you work with partner organizations?
We are thought partners with the organizations we work with. Most of the payers and providers that approach us know that they could be doing more for caregivers, and intuitively understand it will lead to better outcomes for members and caregivers. But they don’t really know where to start. They don’t have a caregiver strategy. Often, they don’t really know who the caregiver is or have contact information for them.
We build that strategy with them. We provide the learning and support platform, and then make sure it’s integrated into the workflow and existing systems.
Do you roll it out broadly, or is it case by case?
Generally, our partners have specific populations in mind where we focus, but access to the program is usually available across the organization, because supporting caregivers is becoming an enterprise-wide priority.
We’ve always focused on high-need populations. We’ve helped a lot of folks in really challenging care situations, like parents of kids with intellectual and developmental disabilities, or caregivers for individuals with dementia, cognitive decline, or a recent stroke. These are areas of focus where a social worker, nurse, or discharge team might be more deeply ingrained with Trualta than in other service lines.
What are the company’s priorities over the next three or four years?
Our vision for Trualta is that caregiver support is as ubiquitous as patient education. At every point of care, any discharge, especially with our aging population and shift to value-based care, it is so important that families are supported.
Our vision is, let’s take caregiver support from being a “nice to have”, where a few teams are doing it with some populations, and make it a critical part of every point-of-care experience. If a caregiver is present, we need to identify them, engage them, and support them to ultimately improve outcomes for their loved ones. We need to make sure that they are not overwhelmed and burning out.


















































Amazing that the takeaway is that its easier to buy a gun than to get credentialed as a physician is…