Kevin Phillips, MBA is business category leader of acute care informatics with Philips Capsule.

Tell me about yourself and the company.
I joined Philips in 2021 through the acquisition of Capsule. I’ve been with the company for 16 years.
Now more than ever, we have an opportunity to make an impact on improving how clinicians can more effectively care for their patients and reduce the tedious elements of documentation, the steps to find information, and the need to react to details, all to allow making faster and more informed decisions.
How does the former Capsule Technologie business fit into the healthcare strategy of Philips?
It’s clear for us that to support the move toward virtual care, to remove some of the manual repetitive tasks for the frontline care team, we need to find ways to arm clinicians remotely to support and assist that frontline care team. It all starts with how we harness the live data that is connected to all of those devices around that patient bedside,
We started, decades ago, with how we automate data for use in medical device integration to the EMR. That has now expanded to, how do we leverage that same data and transform that into actionable insights in a host of different locations? It could be within the central station at the nursing center station. It could be at centralized virtual care centers. It could even be at the mobile handset of that care team. They can now start to manage their patients really anywhere.
It started with the observation that live streaming data is a critical resource for moving from reactive to proactive care.
Once all of that data became available and the opportunities to analyze it became obvious, how did it shake out whether that would be done a company like yours or the EHR vendors themselves?
If we look back over the past 25 years, medical device integration was once a Class Two medical device. Most EMR companies have historically shied away from moving into the medical device realm. Also, connecting to these devices requires at times hardware connectivity such as hubs and unique cabling that gets deployed in the room.
For those two reasons, while a few EMRs have moved in that direction, it was a logical place for a dedicated entity to focus. Philips, as a leader in patient monitoring, said, we have the capabilities to connect to all these devices in the room. Not just manage them for getting data into the EMR, because less than 1% of that data makes its way into that patient record, but to leverage all of that data for more proactive use cases as well. Other use cases around full disclosure databases, where you can dive into risk initiatives or leverage things for alarming and alerting as well.
Moving more and more into this regulated space is why EMRs haven’t dipped their toes fully into the space today.
What is the value of that other 99% of data that EHR vendors don’t use?
In most charting systems, you’ll typically chart every one to 15 minutes. The key element is that there needs to be a clinical validation step. That’s why they’re not doing it in more routine fashion.
What is missed when you capture only a snapshot of that data is alarms, waveforms, and device settings that provide comprehensive but subtle insights in patient care, such as the physiology of that patient and the status of devices. If you start to understand those subtleties, can new insights be brought? How can we, through partnerships where these same questions are being asked, better leverage all of that data to leverage some insights as well?
What kind of device monitoring do you do?
One example is the different modes of a ventilator. The data is critical for a respiratory therapist to understand the state of the respiratory care for that patient. Those sorts of elements give additional context to not just the device, such as ventilators, but if we look at all the devices that are surrounding that patient and capture all of that together, you can have a richer view of that patient.
There are also scenarios of failure modes for devices or sensors falling off. Understanding those alarms or states can give additional clues around how somebody who responds to those alerts remotely, or who provides secondary oversight, can tell the bedside care team or the remote care technician how to effectively manage that patient and how to manage the devices in that room. That’s why even the device settings are of critical importance in many situations.
How much of the company’s strategy is driven by data needs that didn’t exist or weren’t possible a few years ago, such as clinical surveillance, virtual care, and real-time analytics?
Most of our investments are toward moving us into that direction. We’ve invested significantly in the data model of all the drivers that are communicating to each of these medical devices to truly support this semantic interoperability where waveforms, alarms, and device settings can be liberated and ubiquitously understood by all endpoints.
Secondly, we are seeing this move towards flexible, centralized monitoring units. Remote virtualization, where patients may not move from one care setting to another, but the technology does and the care team moves and adjusts with them. To do that, we needed to find ways that we deploy this data management backbone so that data can be leveraged. But also tools, applications, holistic viewers, and the ability to alert assigned care teams to changes in that status.
The technology now supports these new care models. But there’s also this collaboration with our clinical services team and clients that help understand their objectives are and how we can help them change how care is delivered from that in-person to remote virtual care location as well.
Is the level of EHR integration as deep as you need? Does the EHR need to follow you along as you come up with new concepts of how the data you capture can be used on their side?
Yes, but I would say that sometimes the EHRs get maligned with “they’re not interoperable” and “they won’t share data.” We share a lot of the data that we capture from devices. The context around the ADT, labs, and patient history is fairly easily obtained from the EMR.
This relevant context, when paired with live data, that deliver this additional insight. A lot of the research and partnerships that we have with key academic hospitals like MGB are allowing us to identify these observations and then deliver those insights back into production.
I find the EMRs to be actually quite collaborative in this. For the clinicians, these are contextually launched within EMRs. It’s actually a quite collaborative process across the board.
What opportunities does AI present?
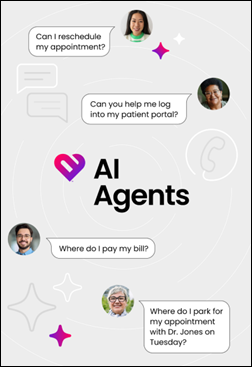
We have used machine learning techniques to help us build a variety of our algorithms that are deployed in our solutions today. We’re also seeing that new agentic AI helps us streamline mapping that we use within our drivers, obviously with human validation at the back end.
We also have many different reporting, retrospective reporting solutions. We have surveillance tools where you can see alarm events trends, but sometimes you just want to ask a simple question about what has happened. These are areas where generative AI and assistants can be deployed in these tools. We are continuing to explore that area and drive it into the solutions moving forward.
Agentic AI will allow us to reason with the data and eventually integrate video over time. We can reduce and streamline unnecessary workflow steps. That is just fascinating. In all aspects of our life, we are evaluating how AI can reduce the number of steps to get certain activities completed. That’s no different than what we are trying to accomplish within Philips as well.
What factors will be most important to your business strategy over the next few years?
We have seen tremendous advancements in technology. But we have to co-create with hospitals to identify how we can support clinical adoption and change workflows. Activating virtual nursing, virtual observation, and virtual surveillance use cases requires a shift in the activities that are done at the bedside, which activities are done virtually, and how that collaboration occurs. There is certainly a big push and a need to move towards that. But we have to figure out how we continue to collaborate with our health systems to maximize and streamline that workforce.
There is also the reimbursement landscape and the regulatory landscape around deploying AI into solutions and medical devices. We expect to see additional guidance from the FDA. How can we identify the best pathway to introduce this new technology in a safe and effective way? That’s always our core focus.
We could focus on a million different use cases. Our focus is to co-create with specific leading health systems and work backwards from highly impactful use cases.
If we do these things, our investments will have a global impact with the clients who use our solutions.
Comments Off on HIStalk Interviews Kevin Phillips, Business Category Leader, Philips Capsule











 e
e






![image[10] image[10]](https://histalk2.com/wp-content/uploads/2025/11/image10.png)
![image[6] image[6]](https://histalk2.com/wp-content/uploads/2025/11/image6.png)





There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…