Mitchell Morris, MD is a principal with Deloitte Consulting LLP.

Tell me about yourself and the company.
I am a partner at Deloitte. I lead our health information technology practice.
My background is a little unusual. l started as a physician and was in academic practice for nearly two decades at MD Anderson Cancer Center. I got very interested around problems of quality and efficiency in healthcare, as so many of us do, and what technology tools can be brought to bear to solve those problems.
I complained a lot, got put on a committee, kept complaining, and I was chairing the committee. Eventually they said, “Well, if you think you’re so smart, here’s a budget, you do it.” Over a period of years, I ended up being the chief information officer at MD Anderson, a post I held for about six years. I left for consulting in 2001. I have been with Deloitte for going on seven years now.
Most of us in hospitals think about Deloitte working with providers, but you have responsibility over pharma and medical devices as well. Do you a lot of issues that overlap with what we traditionally think of as healthcare IT?
Yes. It’s a fascinating time. One of the things about being at Deloitte, the nature of our company gives us exposure to some of the areas of convergence that are happening.
Some great examples are large health plans acquiring medical practices and even hospitals with an eye towards payment reform and accountable care. We’re seeing tremendous convergence there. We’re seeing a great level of interest in life sciences companies – pharma, biotech, devices — in better understanding and integrating with what goes on in the provider world. Their business models are driving them towards closer integration and accountable care is even a part of that.
An interesting phenomenon to watch is academic clients — academic health centers and universities, who in a sense can be viewed as small biotech companies on their own as they have a research agenda — are also linking up the combination of genomic and phenotypic information from electronic health records with what goes on in the laboratory.
It’s a pretty exciting time when you look at all of the different pieces that are in the mix. The driver of health reform making everyone go into a frenzy has created a lot of activity. It’s fun to get creative and innovative around it, but then it’s all sometimes a little frightening as to where we’re all headed and how much control we have over it. But it’s been a good time from that point of view to be a healthcare consultant.
Every kind of company is positioning themselves for whatever they think the healthcare system will look like. The roles are becoming blurred about who’s the provider and who’s the payer. Do you think all this is going to benefit patients?
That’s a great question and I don’t think there’s an easy answer. Certainly the current healthcare system is too fragmented, broken, and too expensive, so we needed to change. What I wonder about is how much pain we’re going to go through during the change process and how quickly we will get to something that actually does help patients.
I think at the end it will help patients and consumers. Part of it also is your perspective. In the US, we tend to have a perspective of healthcare from the point of view of the individual. What’s going to happen to me or my loved one and what can I access for them? Most other countries have the perspective of the population. I’ve got a bucket of money. I have a population I need to serve. How can I do the most good with the bucket of money I have?
As we transition as a country from a very individual view of healthcare — that we do everything for everyone — to a more population-based view of population health management, another common term along with accountable care, there’s definitely some pain that we will go through and some careful examination of our values as consumers and providers of healthcare as to what we think is most important. I’s a not easy decision ahead of us on that score, I don’t think.
Most of the science of public health was developed in this country, yet most of it gets exported to other countries whose citizens accept that concept better than ours. Is there a movement that suggests we will begin to behave more like a public health organization?
There are signs that Health and Human Services is directing funding to that end. I think the different iterations of value-based care, whether it’s accountable care organizations or other forms of value-based payment systems, are a step in that direction. The formation of the PCORI and their funding and pushing clinical effectiveness studies and the regulatory pieces that are coming out for pharma and for healthcare providers around clinical effectiveness are pushing us in the right direction. We make decisions and consumers make decisions not based on what they saw on the television commercial for that new drug, but rather let’s look at some data and see not just from a Phase III clinical trial but actually out in the market, what’s the most effective way to spend our healthcare dollar to be most helpful?
The pace sometimes seems fast to us, but I think it’s proceeding fairly slowly. I think an open question is this. We get to 2014 and as the health insurance exchanges kick in and more people have access to care, there will be further pressure on reimbursement. The whole sequestration issue in Washington right now is having a big impact on that as well with a 2 percent Medicare cut.
I think those things are going to be drivers in the marketplace to accelerate the adoption of some these other approaches to reimbursement and care in general. It has a potential to move faster than it is, but one thing I’ve been guilty of in the past is thinking things will happen faster than they will. I wouldn’t be surprised if change continues to be at a relatively slow pace and maybe that’s a good thing.
Are we putting too much faith in both the motivation and the ability of providers to use business intelligence and analytics to improve outcomes and reduce costs?
You probably went to HIMSS and a lot of your readers did. I think at least half the industrial exhibits there had the word “analytics” on the booth somewhere. There’s certainly a great deal of interest, but also a fair amount of hype.
The question will be when provider organizations in particular have to continue their march towards Meaningful Use, they have to deal with ICD-10, they have to deal with shrinking reimbursements and their cost-reduction initiatives –are they going to be willing to spend on things that are not required to do? If they do spend something, will it be a minimalist approach or a more comprehensive approach towards analytics?
Trying to run a healthcare organization today without good at analytics is like flying a plane blind. But I haven’t seen a huge change in organizations’ willingness to significantly invest in this.
The good news is with all the competition that’s out there creating solutions, that’s driving prices of solutions around analytics down. You don’t have to spend millions of dollars. There are out-of-the-box things that can help you, for example, analyze your revenue cycle or analyze readmissions or fill in the blank of what your current problem is.
To do a comprehensive approach to solve the analytics problem at an organizational level requires some investment, careful thought, and careful adjustments of governance and organizational structure to make it work. I think we’re ways away, but as measured by the interest at HIMSS, it seems like a lot of people are talking about it, that’s for sure.
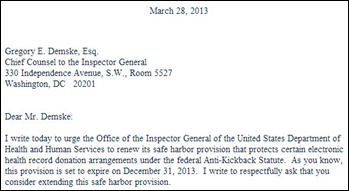
Do you expect to see any new government involvement with healthcare IT issues, for example usability or FDA regulation?
As we take each federal agency, I think FDA has a strategy that they are enacting at a careful pace that will include a greater degree of regulation and oversight and a broadening of what they provide oversight for. I think in terms of what comes out of ONC and the rest of Health and Human Services, it’s hard to guess what kinds of things will come out from them. I think they pretty much have a full plate right now, but I wouldn’t want to speak for what their intentions are. Deloitte does a lot of work for those organizations, so I feel it will be improper for me to speculate.
What’s your overall thought on Meaningful Use as a program?
It certainly stimulated a lot of spending and a lot of progress. It’s far from being perfect, but I think overall it has driven a lot of benefit and organizations that had been taking a wait-and-see or very slow approach to the adoption of electronic health records –and certainly in the case of medical practices — it’s really accelerating things.
The challenge that we have as an industry is not just getting in a system and checking the boxes on the Meaningful Use attestation document, but being able to really say as a group medical practice or as a hospital system, we’re driving benefits around quality and efficiency by using a system that we didn’t we have before.
While there are examples of electronic health records achieving benefits, there are also examples where it didn’t work out so well. It’s frustrating for me personally that as an industry, we haven’t done a better job of showing a broad and widespread benefit. We shouldn’t even be asking this question, and debating is kind of shameful in a way.
The good news is most organizations I’m working with and our teams at Deloitte are working with are showing really great progress. It’s happening at a much faster pace because of the federal funding compared to prior to that. The maturity of the software also has a lot to do with it today, too.
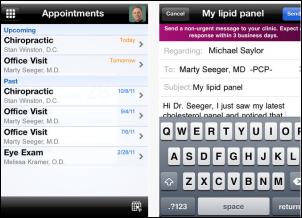
Other than the minimal requirements for Meaningful Use, are providers showing an interest in technologies that engage and motivate consumers or patients directly?
I think that’s emerging. In terms of working directly with consumers, some of the healthcare organizations — and I’ll include health plans in this — that are a little more on innovator side are really looking at solutions that involve mobile technologies that go into the home or to the workplace and help with wellness and chronic disease management. There’s plenty of examples of where those things have been successfully implemented.
As we get towards more mature versions of accountable care, linking together all the providers in a consumer’s ecosystem that they deal with and allowing things to happen at home or retail settings is a tremendous advance. A lot of that is technology enabled. You can’t do it without technology.
We’re still at the early stages of developing transactional systems that advance the agenda around population health management. We’ve got some pretty good back-end analytics stuff that we’re capable of doing today. We still have a way to go on on the transactional side.
Part of it is that interoperability is still off in the future somewhere. Every community has a bunch of different systems that they have to put together, so that that makes it challenging. But there are some interesting emerging technologies from several software vendors that, as they mature, are going to bear some fruit.
What healthcare IT changes do you predict over a three- to five-year timeline?
It’s always difficult to predict disruptive things that might come along. Barring that, I look at what our clients are really challenged with. Managing and reducing cost is a huge issue, not just of IT, but overall. Being able to manage IT spend, looking and doing that through selective sourcing, making sure the organization is firing on all cylinders, being able to support analytics for your organization to reduce cost, making sure the revenue cycle systems are firing on all cylinders. Those things are going to be tremendously important.
We see the healthcare industry consolidating. At Deloitte, we have very large merger and acquisition practice. They’re tremendously busy, and we are doing a lot of post-merger integration. When all of the consolidation occurred in the 1990s, very often there wasn’t consolidation of IT and supply chain and HR, etc. Now because of the cost drivers, as we are seeing medical groups consolidate, hospitals consolidate, health plans consolidate, they are all trying to figure out, how do we get IT to be a key enabler of the efficiencies that we expect to gain from the merger or the acquisition? We’ll see a lot of that.
Preparing for value-based payments through accountable care and all the analytics need to support that we’ve already touched on. Convergence with the health plans and life sciences will be another significant driver. What’s going to wind down a little bit as this big round of primary implementations gets finished for Meaningful Use around clinical systems, that work will diminish, although there’s still a lot of optimization work that can be done out there. “I installed Epic, Cerner, fill-in-the-blank system, but to really get the benefit I expected, I need to spend more time looking at workflow and efficiency and quality and decision support. I think that’s work that I will spend time on.”
ICD-10 is going to wind down. I think mobility is going to crank up. The whole layer of coordinating care at the population level rather than at the facility level will create some opportunities for existing software companies, there will probably be some new entrants into the market who are able to beyond what an HIE does, really coordinate the care and the workflow beyond the walls of an organization. There’s multiple pieces of the provider supply chain taking care of people out there.That will be a really interesting one to watch.
At the Deloitte Center for Health Solutions, we recently released some work by Dr. Harry Greenspun that interviewed some CIOs of large systems and what they’re thinking. Some of the things I’m saying are reflected in that, and as well as some of challenge, which is juggling so many different priorities. I think one of the challenges our CIOs and healthcare today face, if you ask them what’s their number one priority, they’ll list 10 things because they’ve got so many things they have to do. That competing set of priorities that are all number one gets reflected in everything that we’re doing in the industry, and everybody who works in it is a reflection of all those things that are going on in healthcare. Those things are fun, but also a headache at the same time.
Comments Off on HIStalk Interviews Mitch Morris, MD, Principal, Deloitte Consulting LLP








































The CEO sentenced to jail for massive healthcare fraud will get pardoned in a week.