Top News

Cerner acquires Labotix Automation Inc., which offers specimen handling and transport systems for clinical labs.
Reader Comments
From
Katie:
“Re: market research companies. We as a vendor are interested in gathering information from our target audience of hospital CIOs and HIM leadership. Do you have any suggestions of anyone with market research expertise and connections in these areas?” I always prefer to open these questions up to readers so I don’t miss anybody. Leave a comment or
e-mail me and I will forward to Katie.

From Shannon Vogel: “Re: EHR incentive payments as taxable income. I thought the IRS guidance may be of interest to your readers.” Thanks to Shannon, who is HIT director of the Texas Medical Association, for providing this information for those docs who are probably less than elated to see 1099s in the mail for their Meaningful Use payouts:
EHR Incentive Payments are Taxable Income
Physicians should have received an IRS Form 1099 from the Centers for Medicare & Medicaid Services for the incentive payments. The forms had to be postmarked by Jan. 31 and were mailed to addresses on file with Medicare. If you did not receive your Form 1099, you may request a duplicate copy by calling (888) 734-6433, which will take you through a series of prompts (1-1-1-1-2). You will be asked for your National Provider Identifier. Physicians in the Medicaid EHR incentive program should have received a Form 1099 from their state Medicaid office. The Internal Revenue Service issued guidance on the EHR incentive payments that may help in tax preparation, especially if payments were assigned to your group or hospital.

From Don: “Re: San Diego. Here’s hoping we can bring HIMSS back to San Diego where it belongs! Once the pompous mayor here concedes defeat of his push to renegotiate the hotel room tax, construction can begin. Maybe see you all back in The Gaslamp District in 2016 or 2017. Bring your finest shoe-wear and cut some rug at the grand ball room at The Hotel del Coronado.” San Diego gets the green light for a $520 million expansion of its convention center, which will take about three years. Now it’s up to HIMSS. San Diego, Seattle, and San Francisco are my favorite cities of those I’ve visited because they are on the water, have interesting terrain, enjoy mostly pleasant weather, and are walkable.
HIStalk Announcements and Requests
It’s last call to fill out my quick reader survey. I do it just once a year right after the HIMSS conference. Pretty much every change you’ve seen over my 10 years (hopefully more good than bad) came from survey comments. Inga gets nervous this time of year because after I’ve digested the hundreds of responses, I make our to-do list.
Acquisitions, Funding, Business, and Stock

Sutherland Global Services completes its acquisition of Apollo Health Street, the technology subsidiary of India-based hospital operator Apollo Hospitals Group.

Emdeon reports Q4 revenues of $300.7 million, up six percent from a year ago, and a net loss of $10 million vs. $70 million.

Tenet subsidiary Conifer Health Solutions, which offers revenue cycle solutions, breaks ground on its new headquarters construction in Frisco, TX. The company acquired Dell’s revenue cycle business in November 2012, increasing the annual patient revenue it manages to $21 billion.
Sales
Maricopa Integrated Health System (AZ) selects HP Data Protector and HP StoreOnce for data protection and disaster recovery.

Providence Health & Service will deploy Health Catalyst’s data warehouse and analytic accelerators across its 32-hospital system.
Canopy Partners (NC) chooses the MModal Catalyst for Radiology platform for reporting and analytics.
People

PatientSafe Solutions names Tim Needham (Rubbermaid Health) VP of its western region.

Long-term care provider CenterLight Health System (NY) hires William C. Pelzar (Health Dialog) as its first CIO.

Anita Samarth, Clinovations president and co-founder, is named by the Washington Business Journals as one of the top 25 Minority Business Leaders of 2013.
Announcements and Implementations
Delaware HIN and Kansas HIN validate interoperability by exchange of patient records via Direct messaging using solutions from the Allied HIE Company and ICA’s Direct Messaging and Exchange products.
Beth Israel Deaconess Medical Center (MA) deploys CommVault Simpana for data backup and security.

Beloit Health System (WI) goes live this week on Cerner.
Clinithink releases an online version of CliX, its natural language processing engine.

Lifespan (RI) announces its plans to redesign its delivery model that includes implementing Epic at a cost of $90 million.
AHIMA calls for nominations for its Grace Award that recognizes outstanding achievement in health information management. Evaluation criteria include how organizations contribute to a patient-centered model of care, advance the use of electronic health records, and integrate HIM throughout the workplace.
Government and Politics

ONC launches Web pages to support its goal of having 1,000 critical access and rural hospitals achieve MU by the end of 2014.
Technology
Healthcare IT research funded by AHRQ has helped Partners in Health and the Regenstrief Institute develop an open EMR that supports healthcare initiatives in developing countries.
Seven Tennessee school systems receive $3 million in HRSA grants to implement telemedicine programs so that school nurses can connect with doctors to diagnose student problems, but the Franklin County school board delays its approval to start the program, citing liability concerns.
Other
Boulder Community Hospital (CO) reports that its Meditech system has been down since last week and is not expected to be operational until the end of this week. Officials say the hospital has “detailed plans” for going back to manual operations. The outage has caused delays in scheduling non-critical diagnostic tests and distributing routine test results, but essential services are still being provided. The hospital offered no explanation of the problem. An anonymous physician said the backup response is “not an organized plan,” while a patient told the local newspaper, “If they can’t keep their computer system running, how can we trust them to perform surgery?”
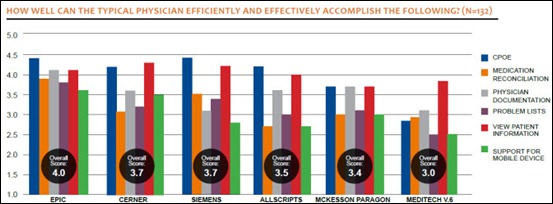
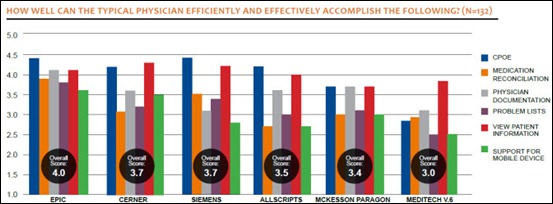
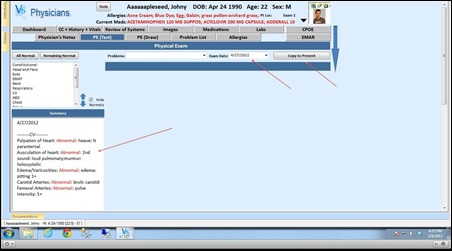
A KLAS report finds that no acute care EMR vendor excels at usability, though Epic and Cerner are best poised to support deep clinical usage. Providers assume the bulk of responsibility for making EMRs usable and 86 percent say that configuring their EMR solution required moderate to extensive effort. Stage 2 MU, with its increased requirements for physician documentation, medication reconciliation, and problem lists, will magnify current EMR challenges.
EMR vendor Lawrence Melrose Medical Record, Inc. notifies the New Hampshire Attorney General’s office of a data breach that has potentially compromised the PHI of two state residents.
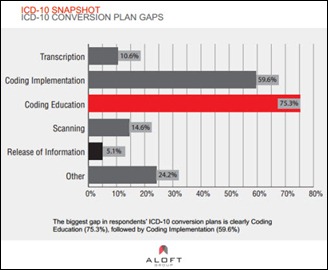
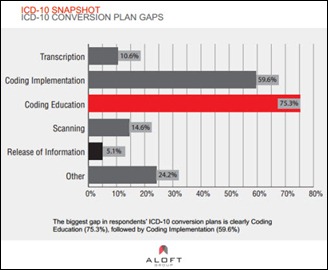
A small study of healthcare professionals finds that 75 percent of organizations are 25 percent or less complete with the ICD-10 transition process. Coding education and implementation are the biggest conversion gaps. Almost half the respondents express some concern about being ready in time to meet the October 1, 2014 deadline.

Weird News Andy finds this “more than an inkling.” Electronic sensors printed directly on the skin, aka “electronic tattoos,” can monitor health signs such as temperature and hydration status. One potential medical use would be to stream surgical wound information wirelessly to providers.
Strange: a nurse from India working in an Australian hospital just a month after finishing nursing school is fired and banned from practice after giving a 79-year-old patient the contents of a bottle marked as containing heart pills that actually held liquid detergent the patient had been using to clean his dentures. The nurse, who argued that he followed four of five medication administration rules, was ordered by the nursing board to take an English competency test, which he failed in six attempts.
Sponsor Updates
- Glenn Focht, MD of Boston Children’s Hospital spoke at a private reception during the AMGA conference in Orlando hosted by Ingenious Med.
- An EDCO Health Information Solutions Webinar profiles two McKesson Patient Folder facilities that enhanced their scanning processes using EDCO technology.
- Industrial Alliance Insurance and Financial Services signs an agreement with TELUS Health to allow certain healthcare providers to use TELUS Health’s eClaims Web portal service.
- ThedaCare (WI) selects Wolters Kluwer ProVation MD Cardiology for its catheterization labs at Appleton Medical Center and Theda Clark Medical Center.
- Ping Identity opens registration for its Cloud Identity Summit 2013 July 8-12 in Napa, CA.
- Emdeon releases details on its upcoming Webinars.
- Prognosis offers a four-part series on strategies for MU success.
- Hayes Management Consulting commemorates its 20th anniversary with an updated website.
- Nuesoft hosts a March 27 Webinar on best practices for medical billing.
- Jason Fortin, a senior advisor with Impact Advisors, discusses the need for smaller practices to select an EHR vendor that is capable of achieving Stage 2 MU certification.
- The Tampa Bay Business Journal names MedHOK the winner of its 2013 BizTech Innovation of the Year Award.
- Surgical Information Systems CTO Eric Nilsson offers a primer on how to set up a clinical quality reporting program.
- Merge Healthcare announces that more than 650 orthopedic surgeons at over 50 practices already have or are in the process of implementing Merge OrthoPACS.
- ChartWise:CDI posts its 2013 conference schedule.
- SiliconMesa partners with DrFirst to provide Rcopia e-prescribing functionality to customers running the SiliconMesa EHR and PM system.
- Craneware announces its support of the Alzheimer’s Association and Alzheimer Scotland as part of its 2013 Craneware Cares corporate responsibility program.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.







































































The CEO sentenced to jail for massive healthcare fraud will get pardoned in a week.