News 6/19/13
Robert M. Wah, MD, a reproductive endocrinologist, chief medical officer for Computer Sciences Corporation, Navy veteran, and ONC’s first deputy national coordinator, is elected president of the AMA. He’ll take office in June 2014.
Reader Comments
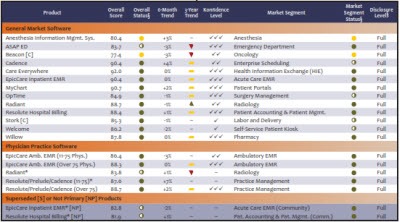
![]() From Alectrona: “KLAS Mid-Term report. Epic was the only acute care EMR to earn a green stoplight.” In KLAS-speak, a green stoplight indicates a customer satisfaction that’s at least six points above the average for that product segment. EpicCare Inpatient scored 90.4 compared to the 12-month segment average of 73.2. Cerner Millennium PowerChart came in a distant second at 77.5. The average score for community hospital EMRs was 70.6, indicating a good deal of discontent across both segments. Ambulatory EMRs fared better, led by PCC EHR (94.5), EpicCare Ambulatory (88.3), and SRSsoft EHR (86.7).
From Alectrona: “KLAS Mid-Term report. Epic was the only acute care EMR to earn a green stoplight.” In KLAS-speak, a green stoplight indicates a customer satisfaction that’s at least six points above the average for that product segment. EpicCare Inpatient scored 90.4 compared to the 12-month segment average of 73.2. Cerner Millennium PowerChart came in a distant second at 77.5. The average score for community hospital EMRs was 70.6, indicating a good deal of discontent across both segments. Ambulatory EMRs fared better, led by PCC EHR (94.5), EpicCare Ambulatory (88.3), and SRSsoft EHR (86.7).
From Stephanie: “Re: EMR. Can you recommend a system that would be ideal for a small, new epidemiology practice?“ I’ll open the floor to suggestions, particularly for EMRs known to work well for a practice of that type.
From Re-Org: “Re: Springfield Clinic. Dual-headed CIO initiates re-org and dismantles the clinical informatics department, which merges with IT. Top talent jumps ship along with dual-headed CIO. HR will no longer meet with confused, misled, and frustrated employees.” Unverified.
HIStalk Announcements and Requests

Welcome to new HIStalk Platinum Sponsor SpeechCheck. The Yorkville, IL company can help prevent errors that occur when physicians (especially radiologists) fail to correct mistakes created by speech recognition systems, which is often a problem with their rapid rollout. Those mistakes can cause embarrassment, loss of reputation, patient care problems, and lawsuits. The company analyzes a facility’s reports, trains their physicians, and develops measurable quality standards that include a goal of 98 percent accuracy and zero critical errors. The result is improved care, risk management, and increased reimbursement. Choose from four service packages that offer choices for type and frequency of auditing, creating or reviewing templates, one-on-one physician training and conversion to self-edit , and compliance updates. See where you stand by finding your documentation quality metric. As the company says, we’ve all seen radiology reports where the technology failed to wreck a nice beach recognize speech. President and CEO Lee Tkachuk is a friend of HIStalk going way back; she also leads ChartNet Technologies and Keystrokes Transcription Service. Thanks to Lee and SpeechCheck for supporting my work.
Maybe I should have taken a picture with my iPhone. I noticed a guy standing at the urinal in the restroom at work doing his business while frantically keying into his iPad mini with both hands. I dawdled at the sink to see if he washed his hands afterwards since I wondered if he could stand the separation from his beloved gadget. He did, not that it mattered at that point.
Acquisitions, Funding, Business, and Stock
CareCloud secures $20 million in Series B financing led by Tenaya Capital, bringing its total funding to $44 million.
Mobile health monitoring provider Medivo raises a $15 million Series B round.
PaySpan, a provider of automated healthcare payments and reimbursements, acquires the assets of mPay Gateway, a point-of-service patient payment solution for healthcare providers.
Sales
St. Mary’s Health Care System (GA) selects Merge’s iConnect Access and iConnect Enterprise Archive for enterprise imaging.
OnePartner HIE will add the Allscripts dbMotion platform to enhance reporting and connectivity.
Nature Coast ACO (FL) expands its relationship with eClinicalWorks to include eCW’s Care Coordination Medical Record.
Community Health Network (IN) will deploy OpportunityAnyWare business analytic solutions from Streamline Health Solutions.
WellStar Health System (GA) selects Avantas to provide consulting services and its Smart Square labor management software to improve labor performance in its nursing units.
Lehigh Valley Health Network (PA) will implement Salar’s TeamNotes solution to capture clinical documentation and comply with ICD-10.
People
HIMSS Analytics promotes Bryan Fiekers (above) to director of consulting solutions sales and Matt Schuchardt to director of market intelligence solution sales.
CareCloud hires Tom Cady (athenahealth) as VP of professional services.
Former CMS Administrator Donald Berwick announces that he will run for governor of Massachusetts.
John Frenzel (Conifer Health Solutions) joins Convergent Revenue Cycle Management as CFO.
Announcements and Implementations
Cedars-Sinai Medical Center reports it has recovered more than $300 million by reducing net A/R with the help of Hyland Software’s OnBase ECM platform.
Mary Greeley Medical Center (IA) implements PeriGen’s PeriCALM fetal surveillance solution, interfacing it to Epic Stork.
Glenn Medical Center (CA) goes live on CPSI.
Laurel Regional Hospital and Prince George’s Hospital Center, affiliates of Dimensions Healthcare System (MD), activate Cerner.
EvergreenHealth (WA) goes live with PatientKeeper Charge Capture.
Bumrungrad International Hospital (Thailand) deploys the Intelligent InSites RTLS solution.
ARC Community Services (WI) implements Forward Health Group’s PopulationManager to monitor addiction treatment programs.
Cerner will embed the MedAssets Claims Management solution within its patient accounting solution.
University of Ottawa Heart Institute (Canada) goes live on the Med Access EMR.
Adventist Health finishes its implementation of Strata Decision Technology’s StrataJazz for operating budgets and management reporting and will begin rolling out additional StrataJazz modules for capital planning and strategic planning.
Government and Politics
![]() National Coordinator Farzad Mostashari, MD has supposedly confirmed that the ICD-10 transition date will not be extended beyond October 1, 2014. If CMS weren’t notorious for soft deadlines, would this even be news?
National Coordinator Farzad Mostashari, MD has supposedly confirmed that the ICD-10 transition date will not be extended beyond October 1, 2014. If CMS weren’t notorious for soft deadlines, would this even be news?
White House Senior Advisor Ryan Panchadsaram, a former executive of Ginger.io and former Rock Health fellow, talks about patients accessing their electronic records at TEDMED 2013.
Other
The first of 4,000 Cerner employees begin moving into the first of two high-rise towers at the company’s new Cerner Continuous Campus in Kansas City, KS.
The Meditech system of Memorial Hospital (IL) has been down since June 11 after upgrade-related problems and won’t return to normal operation until June 24, forcing the hospital to go back to paper charts for almost two weeks.
The UK government fines North Staffordshire Combined Healthcare NHS Trust $86,000 for exposing the medical information of three patients by manually entering the fax number of a psychiatric facility incorrectly and sending it instead to someone’s house.
Sponsor Updates
- Optum donates $10,000 to Arnold Palmer Hospital for Children (FL) in connection with its successful “Make Every Step Count” campaign during this week’s HFMA-ANI conference.
- PeriGen pledges support for the first published draft of nursing care quality measures developed by the Association of Women’s Health, Obstetric and Neonatal Nurses.
- e-MDs expands its headquarters to three locations in the Austin, TX area.
- An eClinicalWorks survey finds that the primary motivator for becoming an ACO or PCMH is to improve patient outcomes, with respondents also stating that an integrated EHR would be the most valuable IT feature.
- 3M Health Information Systems introduces the 3M CAC System, a computer-assisted coding solution for small hospitals.
- Bay Area News Group includes First DataBank on its list of Top Workplaces based on employee feedback.
- David M. Walker, former US comptroller general, provides the keynote address at the SCI Solutions Client Innovation Summit October 15 in Braselton, GA.
- Advocate Health Care (IL) says its use of the Healthcare Workforce Information Exchange from API Healthcare has given the organization the ability to link patient satisfaction with employee satisfaction.
- Craneware introduces enhancements to its Chargemaster Toolkit software.
- Hayes Management Consulting discusses common areas to consider for increased EHR efficiency.
- GetWellNetwork integrates its Interactive Patient Care solution with Rauland Responder nurse call system to improve nursing workflow and communication.
- Capsule posts a white paper that discusses medical device connectivity that is vendor-neutral, open architecture, and device-specific.
- SRSsoft completes the first phase of certification for the 2014 Edition of the SRS EHR.
- HIStalk sponsors AT&T and Ping Identity are included on Computerworld’s “100 Best Places to Work in IT 2013.”
- MedAssets introduces its Procure-to-Pay Solutions suite, which is designed to enhance the management and oversight of contract compliance, standardization, and pricing accuracy.
- Beacon Partners hosts a four-part Webinar on getting the maximum value from HIT systems beginning with a June 21 discussion on optimizing systems to improve workflow around patient access.
- T-System posts a video highlighting its RevCycle+ solutions for physician.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.






























































Re: Dr Z. Great story, but whatever happened to professional courtesy???