Bobbie Byrne, MD, MBA is VP/CIO of Edward Hospital of Naperville, IL.

Tell me how your Epic project is going.
It’s going really well. I’m really very happy to be on this end of the project 10 weeks after go-live. That period of time is little nerve-wracking. It’s like being very, very pregnant and just wanting to give birth.
But even though it’s going really well, it’s really hard. Expectations of what a good go-live means … it’s important to keep resetting that within the organization, that even though we’re having challenges, even though we’re not quite sure how this workflow is supposed to work, and even though we are making a lot of system changes, that’s expected from a good go-live.
I liken it to the patient who wants to know why they can’t run a marathon 10 weeks after having open heart surgery. Well, you just had open heart surgery. We’re not up to marathon speed yet. I think that’s probably typical.
Has anything been a disappointment so far?
I don’t think there’s anything I’m disappointed in. There’s a lot of things I wish I had done differently. If I get the chance to do this again, I will definitely do certain things differently. There are some things that I thought would work out well that worked out beyond my expectations, and then other things that I thought were going to be really great that have faltered a little bit, but nothing that’s been disappointing.
How much of the Epic decision and the Epic satisfaction going forward is based on the personality of the company rather than the product?
I knew from the beginning and in that period before we went live that I felt 100 percent confident that Epic was going to be there with whatever resources or whoever resources were required in order to get us live safely and effectively. I felt this huge confidence of having the company behind us. I knew they would circle the wagons if we needed it.
In certain areas, we did ask for that. “Hey, you know, we really need some help in this area. We didn’t expect that it was going to be this complicated.” Even after we went live we said, “Please come down and help us with this” and they absolutely did. That was no problem.
But you know, I’m kind of an old development junkie. I really believe that the product is super important. Where we have elegant workflows based on sophisticated and intelligent design, things go really well. Where we have workarounds because the product doesn’t quite reflect the nature of the care that we’re giving here, we have a lot more issues.
So it’s the product and it’s the company. I’m going to say it’s half and half.
What is the biggest differentiator that Epic offers that the competitors don’t?
It’s that 100 percent confidence that they’re going to get us to a successful implementation and they will do whatever it takes to get us there. But they also have all the breadth of products that we needed in order to do a complete rip-and-replace of a hospital. They really do have a very robust surgery system and a very robust medical record system as well as clinical systems and revenue cycle.
Nobody in my organization, no department feels like they got the shaft, like they had to take the immature product or they had to take the worst part in order to give up for the rest of the organization. The product suite is mature across the board. Those two things really made me happy that we chose Epic.
One of the discussions that always seems to come up is that CIOs get fired over Epic for whatever reason. Do you think that …
[laughs] It seems seems to be happening even more lately.
Do you think it’s a problem with Epic? What would it take from your viewpoint as a CIO to get you fired in the middle of an Epic implementation or shortly after?
I don’t want to give anybody any ideas [laughs] Two things that I think were really, really key to our implementation — and not being close to those other situations, I have no idea whether these were impacts those other situations, but for us these were really important — is that number one, our revenue cycle implementation was outstanding. We very quickly got our daily charges out the door, got payment back for care that we were giving one and two and three days after go-live. We did not have a big dip in the finances due to Epic.
If you think about the way that healthcare is going today, where there’s just declining reimbursement all over the place for a whole host of reasons that have absolutely nothing to do with HIT. You take hospitals that maybe had some financial stress and then you add Epic and a negative impact for Epic on the finances and I can see why the CIO would be blamed, because now we have some real pain for the organization. That did not happen for us. We had an excellent revenue cycle implementation for a whole host of reasons that I won’t get into.
The second piece is setting the expectations. When you first purchase Epic, there’s a great excitement and everybody is very, very excited about, “We’re going to get Epic and we’re going to do all these new things.” There was a period of time when people thought that Epic was going to solve every problem that has ever happened from a workflow perspective in the hospital.
I started months and months and months ago talking about how hard this was going to be and trying to set the expectations very reasonably. I don’t know if I did it 100 percent and I don’t know if it got through to everybody, but people were saying that all I did for the last three months is walk around saying, “You know, this is really, really going to suck.” So that when there was pain, it was like, “Remember when I told you about how hard this was going to be? This is what I was talking about. This is painful.”
Now we have completely new interactions between nurses and pharmacists, so our nurses and pharmacists get along really well. But now we have these things where the pharmacist says, “I think nurses should do that.” Nurses think, “I think the pharmacist should do that.” These are the kinds of hard choices that we knew we were going to need to make and it’s going to make somebody unhappy.
I think the expectations for the high of buying Epic and the long implementation and then the high around going live and then you head into that we call the valley of despair, where you realize it’s just really, really hard and it takes really lot of work. When we hit that valley of despair, people were expecting it. They said, ”Oh, yes, you told us so. You told us that this was going to come.”
One of my responses to the idea that Epic seemed to be coincident with the CIOs losing their job was that if you were going to fail, there was a strong likelihood that Epic’s executive status report told you you were going to fail. Did you find that to be true?
It’s probably a matter of degree. We did not expect some of our issues around the high turnover procedural areas and that was a little bit of surprise. We had some challenges with that workflow. But for the most part, Epic was warning us, saying, “You know, your staff is a little bit low on this team. That’s worrisome.”
When it came down, those probably were the areas that we should have shored up and maybe would have avoided some of it. But you know, part of this is just a complexity. You think this is thousands of people, thousands of different processes. Epic is really good, but I don’t think even they’re going to be able to totally predict which way your implementation is going to go. And you know, at 36 or 72 or one week or three weeks later, who are going to be the portions of your hospitals that are going to be doing really, really well and who are the portions that are going to be having some challenges. They just don’t have that much of a crystal ball.
One of the other arguments made about why CIOs seem to lose their job after Epic is the huge post-live expense burden. Suddenly the CIO has to try to make things work within the budget that’s allowed when that expense was larger than expected. Do you think there will be surprises in what’s going to cost you to keep running Epic?
No. We talked very extensively at the time that we were doing the purchase and discussing with our board which resources we’re going to stay on. We set the expectations from the very beginning that we were absolutely not going to be able to run Epic on our previous Meditech-level staffing.
The pieces that potentially are coming up as a little bit of a surprise to the organization are the costs of implementing additional modules. The only two things we didn’t implement are the lab product and anesthesia intraoperative documentation. Almost everything else turned over.
When we started to look at what it cost to implement the lab product, there was some surprise. We said, “Wait a minute. I thought we already bought this. It’s part of the enterprise license.” We did have the license fee, but then the additional implementation resources and additional maintenance fee … they thought they were getting a free lab product. We have a joke around here that with Epic, nothing is free, but a lot of things are included.
You have to think about the frame of reference. If you’re trying to do the cheapest IT system you can, Epic is clearly not your vendor, but if you’re trying to think about value for a price and how much we get for how much we pay, I think it seems a little more palatable.
What work is keeping your busiest?
Certainly where we are with Epic is still keeping me busy. We also just closed on a merger with another hospital, Elmhurst Memorial, which is about 17 miles from our core Naperville campus. There’s a lot of work that’s going on in just trying to figure out how these two organizations are going to come together.
We have started to to implement Lawson, which is our ERP system at Edward. We have started that implementation at Elmhurst.
For me, it’s related to stabilizing Epic and getting the Epic mother ship in good shape. Then, how do we extend it out to our new sister hospital?
They are also a Meditech site, right?
Correct.
Is anything going on with the HIPAA changes coming up?
I saw that in some of your talks online. This is something that we have discussed quite a bit internally and felt pretty prepared for. I don’t know whether our compliance and legal team is just maybe a little bit more HIPAA happy than others. It seems like some of your other readers were kind of surprised by this, but these are things that were really were already in play, for us so that’s not something that I am really too worried about.
We continue to have all the worries around how we’re going to grow our data warehouse and how are we going to continue to provide all of the quality data that are required for patients that are medical home. We’ve applied to be in ACO. We have certainly a number of pay-per-performance initiatives going on with different payers.
Maybe a year ago I would have said that’s really what’s keeping me up at night. Now it is is how do I find and recruit enough report experts and people who can work on our data warehouse to keep feeding this beast of requests for more and more and more information? Which by the way, they all seem to want to be formatted it in a slightly different way and have slightly different requirements and definitions. That has become an operational challenge for that team.
Are you using Epic’s Cogito or do you have some other product that will be your data warehouse?
We have a SQL longstanding homegrown data warehouse that we use for many different purposes and have many feeds that go into them, including all of our historical information. We also feed Epic into there. We would want to keep up with as Epic becomes more sophisticated in their capabilities. We certainly want to make sure that we take advantage of what they’ve developed instead of continuing to develop our own, but right now, I feel like we’re in transition.
Are you planning to buy anything for the possibility of your ACO-type arrangement?
I don’t think the contract is signed, so don’t want to speak about it, but yes, we do have a few add-on analytical products that we need to get implemented in order to feed data in, get comparisons, render it back to our physicians in a way that is helpful, that drives behavior, and allows us to bend this cost curve and try and deliver better care at a lower price and then hopefully drive back the gain-sharing that all these systems are intended to drive back to the hospital.
It seems like that’s everybody’s first purchase when they contemplate a risk arrangement is to be able to go to their physicians with data in hand and have the peer pressure do the work for them. How are you planning to take that information out?
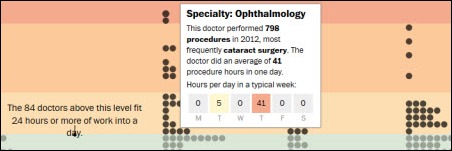
We have the beginnings of the team. They haven’t fully hired all of the bodies that will do that. We already have a physician liaison program in place. I think a lot of hospitals do, where they are going out to the private offices and so know the individuals in their private offices and have developed those relationships. What we’ll do is expand that model, arming these physician liaisons with the analytics and the dashboards and the … not just the ‘Hey doc, do a better job,” but, “Here’s the key parts of this. Here is how other practices have improved their quality scores.”
I think the first part is to get the data out there to the physicians. Makes a lot of sense. We’ve been working on that for quite a while on inpatient data, saying, “Hey doc, your length of stay in the ICU is much longer than all of your counterparts. What’s going on there? Your medication costs per patient are much higher than all of your counterparts. What’s going on there?”
We’ve been doing that for a while on the inpatient side. Now it’s more of just getting the individuals out of the hospital into the offices to work on the ambulatory data, which is of course where most of the care is delivered and most of the care that we will be at risk for is delivered.
Most of your physicians are mostly community based, right?
We have a relatively large employed physician group, about 135, so a medium-sized employed physician group. We also have a partner medical group, which I believe now almost 400 physicians, that we work very closely with. We share an instance of Epic with them. That means that for our own employed medical group and for DuPage Medical Group, it’s seamless experience for them. That maybe makes up about 55 to 60 percent of our physicians and then the other 40 percent are independent. The DuPage Medical Group is certainly independent, but we have a tight IT relationship with them.
When you look at the problems you’re being asked to solve in general, do you see a need for technology that you don’t either have or doesn’t exist?
I see a need to utilize the technology that we already have invested in to a much greater degree more than I see the need that I don’t have a product that solves this problem. Here actually I have the opposite. Somebody says, I have a particular quality initiative that I want to work on, and oh by the way, I found a niche product and some vendor and salesperson called on me and here, I want to buy this product.
When you dig in, you say, OK, but wait a minute. Can’t we already do this with the systems that we have today? That’s where it is a constant going back to, say, instead of buying another product, another product, another product, how can we leverage the investment that we’ve made?
I don’t see that there is a lack of products available for what I want to do. I think sometimes that’s not through the organization, because clearly my organization is still looking for these niche products. I think the piece that we really struggle with — and people say they can do it but I kind of I’m a little skeptical — is getting the ambulatory data out of the private physician offices. People go in and say, yes, I can go into 10 different offices running 10 different EMRs and I have a secret sauce that lets me mine each of those 10 different EMRs and feed quality data back so that we can do things like clinical integration or ACO contracting. I just haven’t seen it, so I’d like to see that actually work.
Does having Epic shut the doors for the need for a lot of other systems?
We come back to our core vendor. We’re focused on that core vendor strategy, so for us, it’s Epic, Lawson, DR PACS, and Merge. We really are starting to say, of these systems that we already own, can one of them already do what this niche vendor might do? So it is very often Epic.
Epic also is very good about telling you they don’t have something. They don’t have case management yet, so they’ll say, “Don’t try and take our system and pervert it and put it into some strange configuration in order to make it into a case management system. It isn’t a case management system. When we have it, we will tell you, and then you can implement it.” I don’t feel like we’re trying to do a square peg around hole a lot. I think it’s just a matter of knowing what the full system’s capabilities are.
When you look down the road five years, what do you see is the biggest challenges and opportunities that your department has or your hospital has?
I think the biggest challenges are going to be the new world order of healthcare. How do we take more risk as hospitals, which many of us have never been insurance companies and don’t have that kind of background, so we don’t really understand what that’s going to be? How do we have the higher quality for everyone, not just for certain subsections of the population? How do we do it at a lower cost?
And then probably most importantly, how do we not go bankrupt between now and that future state? Right now, we still get paid more for doing more. In the future, we will not. But you have to adjust your rate of change with the changes and reimbursement or we won’t even be around in five years in order to continue to serve our community. It’s a very interesting time in healthcare.

















































"most people just go to Epic" that's a problem because then EPIC becomes a monopoly in healthcare, if it isn't…