News 6/11/25
Top News

Mayo Clinic will invest in and partner with Hellocare.ai, whose platform supports virtual nursing, virtual sitting, patient engagement, ambient documentation, and remote monitoring.
Sponsored Events and Resources
Live Webinar: June 18 (Wednesday) noon ET. “Fireside Chat: Closing the Gaps in Medication Adherence.” Sponsor: DrFirst. Presenters: Ben G. Long, MD, director of hospital medicine, Magnolia Regional Health Center; Wes Blakeslee, PhD, vice president of clinical data strategies, DrFirst; Colin Banas, MD, MHA, chief medical officer, DrFirst. Magnolia Regional Health Center will describe how its Nurse Navigator program used real-time prescription fill data from DrFirst to identify therapy gaps and engage patients through timely, personalized outreach. The effort led to a 19% increase in prescription fills and a 6% drop in 30-day readmissions among participating patients. Attendees will learn why prescribing price transparency is key to adherence, how real-time data helps care teams support patients between visits, and how Magnolia aligned its approach with value-based care and population health goals.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
Virginia Mason Franciscan Health (WA) will lay off 116 employees within its Virtual Health Services division and outsource those jobs to a different region, citing state-based financial pressures.
Sales
- Southwest General Health Center (OH) selects Notable’s patient engagement, registration, and intake software.
- MD Anderson Cancer Center (TX) will implement and further develop HealthEx’s patient consent and data management platform.
- St. Charles Health System (OR) selects WovenX Health’s virtual visit and care pathway technology for gastrointestinal patients.
People

California-based HIE SacValley MedShare names Tiffany Hodgins, MSHI (Health Catalyst) chief technology and quality officer.

MedEvolve promotes Matt Seefeld to CEO.

Vaughn Paunovich (Amwell) joins Lifestance Health as CTO.

Dave Icke (Humana) is named CEO of Medisafe, replacing founder Omri Shor, MBA.

CommonSpirit Health promotes Carolyn New, RN, MSN to VP/chief clinical informatics officer, south region.
Announcements and Implementations
Altera Digital Health will integrate Health Gorilla’s interoperability network into Sunrise EHR.
The deadline to submit HIMSS26 presentation proposals has passed even though the annual meeting is nine months away.
Government and Politics
State officials and advocates raise privacy concerns about CDC’s planned consolidation of disease surveillance data on Palantir’s Foundry platform.
Privacy and Security

Jackson Health System (FL) fires an employee who inappropriately accessed 2,000 patient records between July 2020 and May 2025 as part of a scheme to promote a personal healthcare business.
The AMA advocates for limits on how the personal and biological data of physicians is collected and used to address burnout, requiring opt-in informed consent and advance disclosure if data is identifiable.
Other
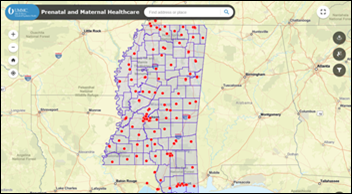
Researchers at the University of Mississippi Medical Center’s Myrlie Evers-Williams Institute develop an online tool and hotline to help pregnant women find clinics within the state that offer prenatal care and accept Medicaid.
An Orlando Health study finds that using the EHR to identify and stratify high-risk metastatic cancer patients for targeted interventions decreased 30-day readmissions and length of stay.
UC Davis Health (CA) sees a considerable uptick in pediatric e-consults after developing specialty-specific e-consult protocols, adjusting referral options within its EHR to remind pediatricians that they can request an e-consult, and increasing messaging about e-consults amongst the larger UC Davis Health community.
Sponsor Updates
- AdvancedMD announces 2025 summer product updates and makes Waystar its preferred clearinghouse partner.
- Altera Digital Health offers a new client story titled “Bolton joins up and accelerates district nurse referrals across secondary and community care using Sunrise EPR.”
- Greece ranks among the lowest-performing nations in Europe across critical digital health benchmarks, according to findings from Black Book Research.
- Arcadia will exhibit at AHIP 2025 June 16-18 in Las Vegas.
- Gartner recognizes Censinet as a representative vendor in its “2025 Market Guide for Third-Party Risk Management Technology Solutions.”
- Clinical Architecture will sponsor a networking breakfast at the CHIME Innovation Summit June 11-13 in Fairfax, VA.
- Capital Rx releases a new episode of “The Astonishing Healthcare Podcast” titled “The Future of Health Benefits: Integrating the Power of Pharmacogenomics (PGx), with Burns Blaxall, PhD, and Caitlin Munro, PharmD.”
- Wolters Kluwer Health updates its Sentri7 Drug Diversion and Sentri7 Pharmacy solutions.
Blog Posts
- Navigating Change: Key Priorities for Revenue Cycle Management Leaders (AGS Health)
- Reducing Wait Times, Restoring Trust: A Purpose-Driven Approach to Patient Access (Tegria)
- Move assets from staging to production with Promotion (Redox)
- From confusion to confidence: Navigating rapid digital technology changes (Altera Digital Health)
- Navigating governance and change management in EHR projects: driving strategic transformation (Cardamom)
- Rethinking the HIPAA Security Rule: Why Forward Path 2025 Might Be the Better Way Forward (Clearwater)
- Driving Change: How To Lead A Digital Strategy For Clinical Innovation (CereCore)
- Innovating Around AI: The Shift Towards Integration and Real-World Impact (Consensus Cloud Solutions)
- Modern Risk Management in Healthcare: Protecting Patients in a Connected World (CloudWave)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Sponsorship information.
Contact us.
























This is a great point—many discussions about patient wait times still focus on staffing or technology, while the real issue…