News 8/21/19
Top News
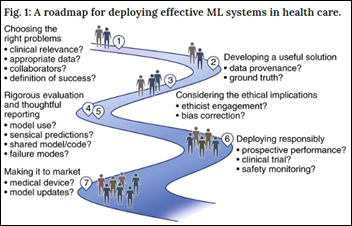
Nature magazine has run some good healthcare related articles lately (they are always called to my attention via tweets from Eric Topol). A new perspective piece covers the responsible use of machine learning in healthcare, containing many points that are likely new to the healthcare-inexperienced technologists who might be searching for any protruding nail for their proudly-created hammer:
- Choose the right problem, not just one for which a convenient ML training database exists. You can predict in-hospital mortality from a wealth of data, but does it tell clinicians something they don’t already know? Will the right people be involved in considering the actions that will be taken in response?
- Make sure the data elements are appropriate. ICD-10 codes entered after the patient’s encounter won’t be available when they are needed. They may also be driven by billing requirements rather than clinical ones.
- Account for inconsistent data collection practices across departments and health systems.
- Make sure that training data represents all populations.
- Watch for potential bias, such as creating an algorithm of whether a patient should have surgery based on those patients who actually did, who are probably more affluent than those who didn’t. Or in cases of a system that can infer information that the patient declined to provide, such as smoking or HIV status, which may cross ethical boundaries.
- Avoid “label leakage” in model testing, such as randomly assigning X-rays between training and testing sets without recognizing that patients have multiple images, which would then overweight the model’s accuracy.
- Break out the model’s testing results into the specific areas where it either excels or fails. Potential users need to know what a particular model works well in adults but not pediatrics, for example.
- Use clinically relevant evaluation metrics that look at the positive predictive value and sensitivity. A model whose high false-positive rate predicts a situation that requires high-cost, limited-value drug therapy isn’t going to be useful.
- Publish results with restraint, sharing code, data sets, and documentation so that other researchers can make their own assessments of usefulness.
- Test the system on real-life patients in silent mode only, where clinicians review the predictions without acting on them. Then move on to randomized controlled trials while recognizing that randomization at the patient or physician level is difficult and could endanger patients.
Reader Comments
From Mo Exposure CEO: “Re: links. Thanks for linking to our company’s news item. The response from HIStalk readers was amazing.” Thanks for deciding to sponsor the site as a result, especially since I don’t run fluff news pieces, meaning your announcement had to earn its way into my news post. Items I mention sometimes get a lot of clicks. Even webinar announcements sometimes get a couple of thousand clicks, and announcing a new sponsor always draws several hundred. Sponsor support comes from having loyal, influential readers, so my only job and outcomes measure is to make it worth their while to return.
From She Lives on Love Street: “Re: [RCM business line omitted.] Word on the street is that it’s been sold to [acquirer name omitted].” I’ve emailed the rumored acquirer’s PR contract but haven’t heard back. I’m running the redacted version to remind myself to follow up.

From Core Cutter: “Re: Apple. This CNBC article suggests internal trouble with its health offerings.” Reporter Chrissy Farr sometimes writes good health IT-related stories, but this isn’t one of them. I suspect her editors are pushing her too hard into drumming up questionably researched, speculation-based stories that hold minimal news value, as in her never-ending quest to take guesses at “what Amazon is doing in healthcare” because naming those big names draws eyeballs, but leave their owners with little useful information. This one tries to extrapolate Apple’s health-related departures into “differing visions for the future” that aren’t backed up by the stated facts. My take:
- She interviewed “eight people familiar with the situation,” none of whom are the people whose departures she noted, and those people she spoke to are simply speculating on why those people left.
- The five folks listed as having departed held wildly unrelated Apple “health” jobs, ranging from marketing to wellness clinic executives. It’s not like a mass exodus, either in numbers or in area of focus.
- The denominator of health-related jobs at Apple isn’t given, so we only know that it’s five positions out of hundreds.
- The story reports from the unnamed sources a difference of opinion among health-related employees about Apple’s direction, but those weren’t tied directly to the departures and those former employees didn’t say that’s why they were moving on.
- The clickbaity, present-tense headline implies a sudden uptick in internal tension, but does little to back that up with facts.
- We don’t have anything to suggest that Apple is disappointed in its health-related results or that it would like to change direction.
- Health and health IT have always had high turnover, some of it based on unreasonable expectations or finding out that big companies just want to make money instead of making people healthier, but in Apple’s case there’s also the possibility of parlaying an Apple credential into an even better job.
- Even if the story is right in claiming internal tension, so what? You’ll know if Apple makes major product or organizational changes. Speculating beforehand may be entertaining doesn’t really add value, except for the sites trying to sound insightful.
HIStalk Announcements and Requests
I Google-discovered Zenni in helping a friend get eyeglasses and it’s pretty cool. You key in the vision numbers from your eye doctor’s prescription (they don’t want the actual prescription), use a ruler to measure the distance between your pupils, and then head off through a long list of frames to choose your glasses. It takes a couple of weeks to received them in the mail from China and then you’re set unless you need to bend them a bit like your optician does for a perfect fit (not necessary in his case). The biggest draw beyond convenience is price – a pair of snazzy progressive glasses cost him less than $50 (they look exactly like his $300+ pair from Costco), single-vision sports glasses with polarized lenses were $60, and no-nonsense single-vision sunglasses were $15 (!!). At these prices, you could stash a pair of prescription sunglasses in every car, get some glasses set for computer monitor distance, and get backup normal glasses for next to nothing. What you end up with is pretty much exactly what the optician would sell you for five times the price after two trips to the store. You still need an eye exam every year or two, but what happens afterward is Zenni’s strong suit. You could do a life-changing but inexpensive good deed by treating someone who can’t afford glasses to a pair of Zennis.
Color me skeptical: a new Frost & Sullivan white paper (which you can download only if you provide work details) predicts that clinical decision support systems “are poised to become the user interface of choice for clinical interaction with health IT,” replacing the EHR. My take is exactly opposite – clinical decision support systems will feed their information and recommendations through the EHR, disappearing in the background but providing no less of a service in recognizing that clinicians rightfully want everything placed into their EHR workflow and design. Nobody in their right mind would suggest that CDSS systems contain everything a clinician needs to see, or to visualize how those systems would interact with the user when several are in use (one for radiology image appropriateness, one for antibiotic stewardship, etc.) I think F&S is way off base here, and had I cared enough to download the report, I bet I would find some CDSS vendor involvement. The HIMSS rag gave it a dramatic headline, a pointless stock art photo, and a non-critical acceptance of what the report’s author said, assuming they paraphrased it accurately. This is one of those reports that predicts huge growth in some market segment, knowing that a more realistic report wouldn’t exactly fly off the shelf.
Webinars
September 5 (Thursday) 2:00 ET. “Driving 90% Patient Adoption Across Your Network: How US Dermatology Partners is Showing Us The Way.” Sponsor: Relatient. Presenters: Michele Perry, CEO, Relatient; Sara Nguyen, VP of applications and integrations, US Dermatology Partners. US Dermatology Partners is helping its physicians reclaim time they can spend with patients and is turning patient engagement strategies into business results across its 90 locations in eight states. Attendees will learn how US Dermatology Partners defined its patient engagement objectives and physician-optimized strategies. They presenters will provide advice on starting or accelerating patient engagement goals.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
The newly hired, cost-cutting CEO of India’s second-largest hospital chain will slash its expenses by 20% in trying to recover from the misappropriation of company funds by its previous owners. Publicly traded Fortis Healthcare will reduce doctor pay, replace people with software, close underperforming hospitals, sell non-essential assets, and ensure that nurses perform only those tasks that lower-paid employees can’t do.
EHealth Exchange announces go-live of a national, single-connection, InterSystems-powered gateway service whose charter members include the VA, AdventHealth, InterCommunity CCO, and OCHIN.
Sales
- Vanderbilt Health chooses Sectra for PACS and VNA in diagnostic radiology and cardiology.
- Medical records retrieval vendor Womba chooses Allscripts Veradigm EChart Courier to aggregate provider patient records to its attorney clients.
People

Spok hires Matt Mesnik, MD (Vigilant Diagnostics) as chief medical officer.

Josh Hoders, MBA (DrFirst) joins Forward Health Group as sales VP.

FDA hires Vid Desai (Vyaire Medical) as CTO.
Announcements and Implementations
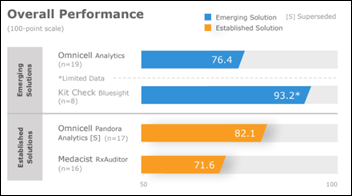
A KLAS review of drug diversion monitoring technology finds that Omnicell Analytics is the most widely adopted solution, but many customers fail to achieve their expected outcomes because they decline to pay the extra cost of EHR integration.Medacist RxAuditor has a lot of customers, but outdated technology and workflows cause most of them to use only its simplest dispensing reports in then chasing down problems via manual workflows. Kit Check’s Bluesight for Controlled Substances holds promise based on early adopter reports.
Other
The URL of Sonoma Valley Hospital (CA) is “maliciously acquired,” forcing the hospital to change its prized three-letter domain name of “svh.com” to “sonomavalleyhospital.org.” The hospital’s URL registration was good through late 2021, but someone updated it using credentials from an unknown source to take control, which an expert contacted by the local paper says is nearly impossible to reverse. I checked the Whois for the URL and it’s now running on China-based servers with “registrar lock” turned on. I thought it was straightforward to contact the web registrar or ICANN with proof of ownership to get the transfer reversed, but regardless, hospitals should:
- Use complex passwords for their domain service’s website.
- Change the registration address if it points to the same domain since otherwise you’ll lose the ability to be contacted if someone grabs that URL.
- Turn on the “registrar lock” option of your domain service so it can’t be transferred.
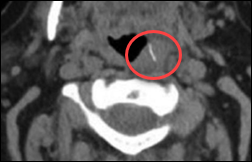
A fired VA hospital chief pathologist is charged with three counts of involuntary manslaughter after a review of his needle biopsy cases showed a misdiagnosis rate of 10%, 10 times the expected rate. The VA says he was responsible for at least 15 deaths and an unknown number of incorrect diagnoses. Colleagues had complained of his erratic behavior for years, but the VA let him continue working while he underwent drug and alcohol rehab, finally firing him in 2018 after a DUI arrest.

Kaiser Health News covers the plight of several “no-stoplight” rural towns that believed Miami entrepreneur Jorge Perez, who promised to save their tiny local hospitals but instead used them in a massive insurance fraud scheme that took advantage of higher lab billing rates for rural hospitals. A 14-bed hospital cranked out bills for $120 million in just six months, of which $80 million went to the hospital’s new owner and little to the hospital, as employees reported running out food, cleaning supplies, and IV fluids, with patients in one of them displaced because their hospital beds were repossessed while they were still occupying them. When insurers eventually stopped paying, 12 of the hospitals filed bankruptcy and eight closed. Perez paid $3.5 million to settle the the DoJ’s false claims charges and says he’ll now focus on his software businesses.
Sponsor Updates
- Hackensack Meridian Health Jersey Shore University Medical Center reduces stroke-related readmissions by 50% after implementing Vocera Care Inform to provide personalized audio discharge instructions and educational materials.
- Healthfinch announces several new customers of its Epic-integrated Charlie Practice Automation Platform and its exhibit at Epic’s UGM next week.
- Aprima will host its 2019 User Conference August 23-25 in Grapevine, TX.
- Artifact Health publishes a new case study describing how its mobile physician query tool helps Western Maryland Health System accurately code episodes of care in a quality-based reimbursement program.
- Burwood Group is raising money for the Boys & Girls Club of Greater San Diego.
- Wolters Kluwer Health releases six new Audio Digest Topical Collections for CME.
- CoverMyMeds and Culbert Healthcare Solutions will exhibit at Epic’s UGM August 26-29 in Verona, WI.
Blog Posts
- Healthcare ERP System Selection (Optimum Healthcare IT)
- Receive a well-rounded educational experience at Evo19 (AdvancedMD)
- 5 years ago, Mayo Clinic made 3 huge bets. Are they paying off? (Advisory Board)
- How Are IT Risks Different For A Company That Handles Protected Health Information? (Fortified Health Security)
- How do you build, deploy and maintain an imaging data management strategy? #The Imaging Data Management Strategy Series (Agfa Healthcare)
- More Than Medicine: Southcoast Health Raises the Bar with Avaya (Avaya)
- Collective Medical Stands by ACEP’s Efforts to Make EDs Safer (Collective Medical)
- Updates from Our 2018 CoverMyQuest Winners: Part 2 (CoverMyMeds)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.









































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…