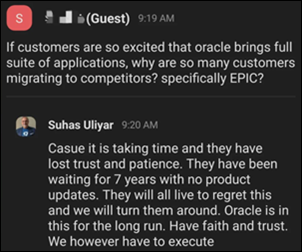
Mr. H is running a poll that asks, “Is it ethical for doctors to prescribe the drugs of their pharma sponsors to people who seek specific treatments?” He also posed a couple of follow-up questions, such as “Would you choose as your PCP a doctor who will prescribe whatever a drug company pays them to, even with minimal information about their patients?” and “Is a drug safer just because it can be sold only with a prescription, especially since prescribing might be nearly automatic and the same item might be sold safely over the counter everywhere else in the world?”
I like the response choices that Mr. H included in the poll. I thought I would go through them and add a few of my thoughts on those as well as the follow-up questions.
No. The patient should see their regular doctor. As a primary care physician, I agree with this one in my heart. Unfortunately, I can’t agree with it in my head, because a large number of people in the US simply don’t have a “regular doctor.”
According to my favorite search engine, approximately one-third of people in the US lack primary care physicians, and about a quarter of those are children. Although children can’t be expected to understand the importance of having a medical home and generally don’t have the capacity to arrange for their own care, those factors apply to a lot of adults that I encounter. Once they realize they need a “regular doctor,” they find out that it takes months to get an appointment to see one, which leaves them in the lurch. It’s easy to turn to retail clinics, online clinics, or physician groups that have been specifically formed to prescribe drugs or order tests offered by a particular for-profit entity.
No, unless they review the patient’s medical records. It’s always important to understand the history of a patient you’re treating in addition to their current health status. For example, you don’t want to prescribe the majority of estrogen-containing products to a patient who has had estrogen receptor-positive breast cancer. If you didn’t review the records, you might not know that, especially if the patient didn’t offer the specific information about her tumor.
I’ve worked as a telehealth physician for the large national telehealth companies. Most of the time in those situations, you don’t have the patient’s records. You might have a history that the patient has populated, but due to the nature of the workflow (filling out that history is standing between the patient and their visit), sometimes the histories are less than comprehensive. Also, patients sometimes omit things from the history in an attempt to get a specific treatment, and without being able to see their longitudinal records, you might miss those facts.
No. It drives costs up for everyone. This response is currently scoring rather low, but it’s an important one. Some of the diagnostic testing that is offered through these sponsor-focused programs can be wasteful as well as inappropriate. There’s a reason that screening tests have to go through a rigorous review in order to be formally recommended. Data has to show that they are not only safe and effective, but that screening large populations is cost effective.
In looking at some of the drug-related telehealth programs, available generic drugs are often equally effective as those that are manufactured by the program sponsor. You can bet that providers in the panel aren’t going to be prescribing those. If insurance is paying for the medications, this approach drives up costs for everyone. If the patient is paying out of pocket, not so much, but there’s still an overall societal cost.
No. It’s a prescriber lawsuit waiting to happen. I’m a little on the fence about this one. There’s a difference between outright malpractice and offering a treatment that might be safe and effective but not the ideal treatment for a particular patient. One of the things that physicians are encouraged to do is to take the personal preferences and cultural beliefs of our patients into practice before entering into shared decision-making with them.
If that sounds like a mouthful, that’s because it is. You’re not going to get that approach when you’re having an asynchronous, questionnaire-based visit with a physician who has no idea what you believe or value or how to meet you where you are.
Yes. It’s legal and what patients want. I’m going to channel millions of parents of teenagers here. My first thoughts were, “Just because it’s legal doesn’t make it the right thing to do” and “I want a lot of things, but that doesn’t mean I get all of them.”
I’ve treated many patients who think they want something. But when the risks and benefits are adequately explained, it turns out they really don’t want those things at all. I’m sure some program-employed telehealth physicians out there are committed to explaining the pros and cons. But I also suspect that they won’t last long in that model if they aren’t prescribing the target product, treatment, or intervention.
Of course, this happens during in-person visits as well. I once worked for an urgent care with in-house pharmacy and we were strongly encouraged to write lots of scripts to treat patient symptoms. Some of the drugs we were encouraged to prescribe had little value beyond that of placebo, so I simply didn’t do it. Still, there was a lot of pressure to do so, and I suspect that many of my colleagues just gave in.
Not sure, but it’s puzzling that doctors do this. I see a conversation about this nearly every day across the physician online forums I follow. A lot of reasons are cited for working in these models. Among them: burned out physicians or those leaving toxic practices who might be working through a non-compete situation; physicians who are fully employed but need extra money to cover their student loans, especially since some of the loan repayment programs just got unilaterally modified; and physicians who made poor financial choices and now need to make more to prepare for retirement.
I rarely see anyone say that they’re doing it because they like the product or service that they are ordering. Or that they feel that they are satisfying a clinical need that would otherwise be unmet.
As for Mr. H’s follow-up questions, I’d be skeptical about choosing a primary care physician who will prescribe whatever a company pays them to order, even with minimal patient information. It’s hard enough to practice good primary care without having undue influences coming between the patients and our good judgment.
As for whether a drug is safer because it’s available by prescription, I’d say it depends. Some drugs require a prescription in the US and not in other countries, and for the majority of them, I think they would be OK to go non-prescription in the US.
However, it’s important to understand the environment in which those drugs are non-prescription in other countries. Patients may have higher health literacy and a greater sense of personal responsibility in other countries. Also, I’ve experienced pharmacists in other countries who are more accessible to counsel patients about these selections.
Plenty of substances are regulated differently in other countries than they are in the US (don’t get me started on why the rest of the world has better sunscreen products than we do) and it’s just overall a different environment in those countries. Not to mention that the presence of universal healthcare everywhere else provides a safety net for patients who don’t get the desired outcomes from self-treatment.
It will be interesting to see the final poll results when they come in. Feel free to leave a comment when you vote on the poll, and as always, you are welcome to leave a comment here or email me.

Email Dr. Jayne.






































I find it incredibly ironic and rather hypocritical that the co-founder of an Epic-centric consulting firm is calling for the…