Happy Thanksgiving, HIStalk! I hope you all had a wonderful and safe holiday yesterday. I know this Thanksgiving looked very different for the majority of us this year, but I hope your day was spent giving thanks and enjoying time with friends and family (distanced or not)!
This column will focus on another interview with a professional in the healthcare IT industry. This time, the focus leaned on the now and the next of healthcare IT throughout the pandemic. I really learned a lot about the nature of healthcare IT’s growth during strenuous times like these, and I hope this column relays some of that well.
Mike Pietig works for Avtex Solutions, an IT service management company founded in 1972 that offers full-service customer experience consulting and solutions. “Avtex is in the business of helping their clients deliver an exceptional experience to their own customers,” Mike said.
Mike has been with Avtex for a year, focusing on a healthcare line for customers who use the company. Avtex needed someone who was familiar with healthcare, who knew the right terms, regulatory requirements, and connections in the field. His role has helped the healthcare line of Avtex Solutions grow faster.
Because Avtex Solutions is a connection solution builder, the company is always seeking ways to solve problems and develop strategies for doing so. Mike has been in the healthcare IT field for about 17 years, and coupled with his workplace’s goals, I figured he would be a great person to talk about the major changes in healthcare IT. We broke it down into two major questions — how has healthcare IT changed and where is healthcare IT going next?
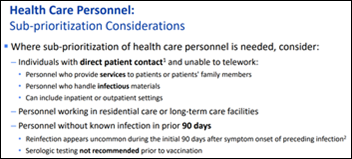
“The first big change was driven by regulatory requirements, government change that forced the healthcare industry to implement electronic medical records and other solutions to satisfy their requirements,” Mike said. “The innovation was happening within individual hospitals, but it wasn’t happening across an entire industry, so the government mandated some of those.”
Mike mentioned regulatory requirements such as the Affordable Care Act and the HITECH Act, both of which were written between 10 to 15 years ago and enforced more accessibility to health insurance and the use of EHRs. These rulings further pressed the healthcare industry as a whole to create platforms that were usable, valuable, affordable, and high speed.
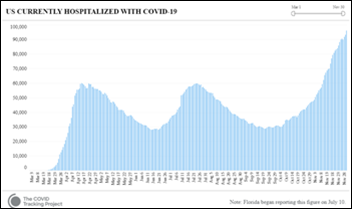
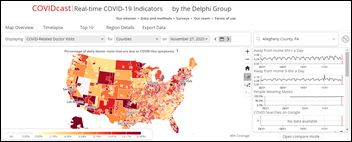
Mike then turned to the pandemic itself to discuss another major change in the healthcare IT industry. COVID-19’s presence has acted as an accelerant that boosted the growth of telehealth, and prompted IT professionals to really ask how and why patients could get better care in a safe environment.
“I would say [COVID-19] probably accelerated innovation by somewhere between five years on the low end to 10 years on the high end, in terms of the technology solutions,” Mike said. “Also in terms of the adoption of telehealth, and virtual visits, and digital front doors, and the idea of consumer-driven healthcare.”
Mike also mentioned a client that had a year-long goal to implement telehealth in nine areas of their hospital. When the pandemic hit, the hospital knew they had to get telehealth going fast, and implemented all nine areas within six weeks.
Mike’s words lead me to think about COVID-19’s impact on not just healthcare in general, but at the fundamental level of how care is delivered. He said that patients need to be treated as a consumer, as someone who has choices where to go and how to get care instead of someone only interested in need-based care.
“We have to deliver a really great experience,” Mike said. “Because otherwise, those customers can take their business elsewhere. Healthcare is now really starting to recognize that.”
I was very curious about this trend, about why COVID-19 acted as a catalyst in a consumer-driven market during a time where the consumer is not necessarily the driving factor. Consumers are benefitting from the exponential growth of the healthcare IT market during a global pandemic because of how quickly providers have had to innovate solutions for safe patient care that slows the spread of the virus.
“We’ve got so many choices now that I’m going to go where I feel I can get the best outcomes and the best value and the best experience,” Mike said. “That is fundamentally different now than the way it has ever been in healthcare.”
Mike’s answers to the next part of my questions were just as interesting. Where is healthcare IT going next? If we’ve grown and adapted so quickly, what could possibly be next?
“I don’t think the technology will go away,” Mike said. “I think there is even more openness or an appetite to new ideas coming into healthcare because everybody is trying to figure out, ‘how do I do more with less?’”
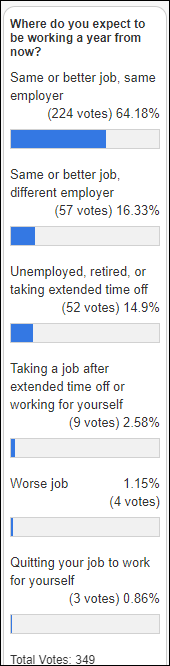
Mike reflected on a recent survey of over 1,000 patients to find out what was important to them during this time in healthcare. Patients don’t want to wait in waiting rooms, touch clipboards, or touch a kiosk, Mike said. The top 10 concerns from respondents were centered on safety. The survey showed that people want quick, efficient, and safe care. Is this the trend that the future of healthcare IT will continue to follow?
Healthcare IT will continue to move forward, most likely with a heavy emphasis on telehealth and its ease of application. But Mike did say that the approval of initiatives is what takes the longest and can be the hardest to do. If an initiative or an idea can prove to be applicable not just when someone is sick, but all year round, it can move forward.
“If you’ve got a strong business case and you can generate more revenue, or measure the expected savings, people will still find the funding for it,” Mike said.
Mike talked a lot about how much he reads HIStalk and how impactful it is to him for work and for understanding the industry. I wanted this column to focus more on healthcare IT, but Mike did say that HIStalk is in his top three reading recommendations for newcomers at his work and for anyone new to the industry.
I know I mentioned doing some research on COVID deaths, but I received an interesting comment that I’d like to do a column on beforehand, if possible. User Kermit mentioned that a friend of theirs is a therapist, and I’d love to interview a therapist currently using a telehealth service to hear their ideas of the pros and cons surrounding its usage. Mr. HIStalk and I discussed the importance of researching the provider side of telehealth. I’d also love to interview a doctor about these aspects, so if you’re either of those or know someone, I’d love to connect.
That’s it for today! I hope you had a great Thanksgiving, and happy Friday!
Katie The Intern
TLDR: Katie The Intern interviewed Mike Pietig from Avtex Solutions. Mike said that the two major changes in healthcare IT over the years have been regulatory requirements and the pandemic as an accelerant for growth.

Email me or connect with me on Twitter.






































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…