News 4/8/20
Top News
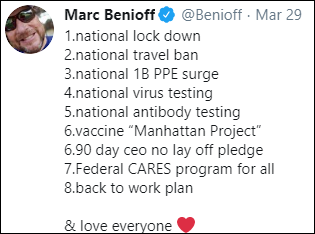
Duke’s Margolis Center for Health Policy – along with former FDA Commissioners Mark McClellan, MD, PhD (the center’s director) and Scott Gottlieb, MD, former National Coordinator Farzad Mostashari, MD, and other participants – proposes a national COVID-19 surveillance system to allow the country to transition from universal stay-at-home orders to case-based, regional options. Recommendations:
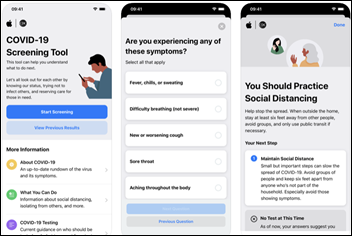
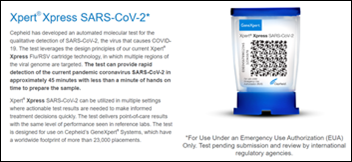
- Roll out rapid diagnostic testing everywhere and for every person with COVID-19 symptoms, allowing quick identification of those infected and of those at high risk (such as healthcare workers), and conduct random tests to detect small outbreaks.
- Use the test-and-trace results to feed a national syndromic surveillance system that transparently reports outbreaks.
- Conduct widespread serologic testing to identify immunity markers and to supporting making decisions about sending people who are immune back to work.
- Require providers that receive federal coronavirus grant money to actively participate in the surveillance and response system.
- Encourage standards-based lab results reporting (CDC, CMS, and ONC).
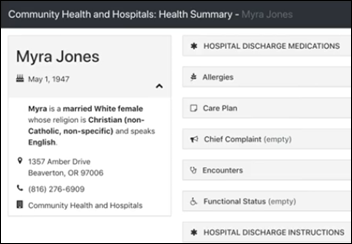
- Incorporate ADT notices into the surveillance system for COVID-19 detection and for correlation to clinical observations, admissions, and transfers to ICU (CDC).
- Publish daily summaries from the surveillance system at the metro area level.
- Improve the use of technology to manage case-based isolation.
- Develop a common platform to query data from hospital EHRs, HIEs, and CommonWell and Carequality (CDC, ASTHO, ONC, and OCR).
- Help health systems and insurers manage patients who have tested positive (CDC).
- Publish best practices and case management models to maximize the ability to treat new cases at home or in local isolation facilities (CDC).
- Pay providers based on case outcomes (CMS and CDC).
- Lead and fund projects to answer questions about asymptomatic spread, the impact of more refined physical distancing measures, the ability predict and influence case severity, and the role of children in transmission (CDC).
Reader Comments
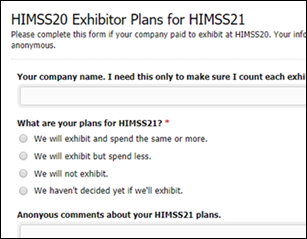
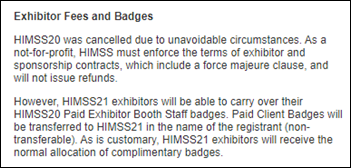
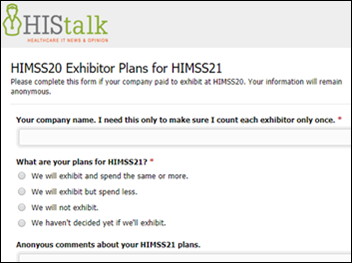
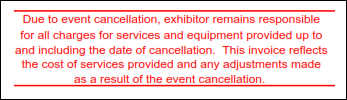
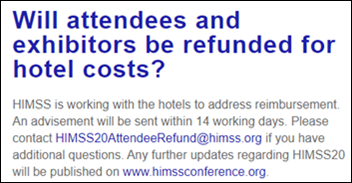
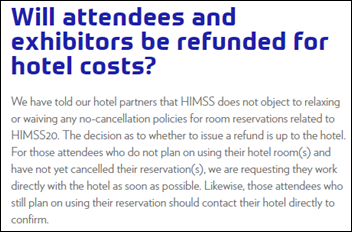
From Anointed Two: “Re: HIMSS20 hotels. I can almost understand Marriott keeping one night’s deposit, but keeping the entire prepaid amount is inexcusable greed. I hope that we vendors remember how HIMSS and OnPeak did nothing to negotiate on our behalf when it comes to HIMSS21.” The hotel rather coldly told this reader this: “The agreement that the hotel entered with HIMSS was an advance payment of each attendee regardless of circumstances. The hotel will be retaining these prepayments.” The HIMSS rationale for requiring exhibitors to book hotels through OnPeak is that the convention center allocates exhibit hall space based on hotel rooms booked. I can confidently predict going forward that convention centers will have all the space any exhibitor could ever want given the dying conference business, not to mention that the HIMSS track record should be adequate to convince the convention center to not stiff it on space. All that aside, I don’t think the hotel policies have caused many gripes in the past, so unless another HIMSS conference is cancelled inside the no-refund window, it’s probably all moot anyway, although I would refuse on principle to book any Orlando hotel for HIMSS22 that screwed me for HIMSS20.
HIStalk Announcements and Requests
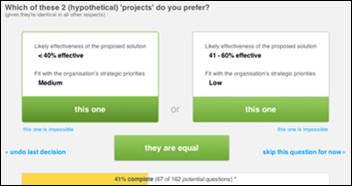
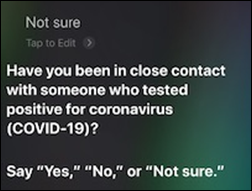
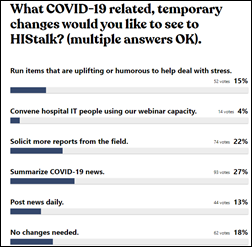
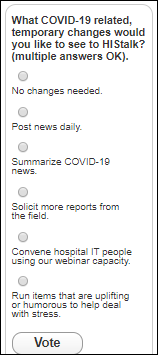
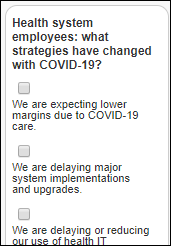
I tweaked my current poll about personal COVID-19 experience to include “presumed positive” in addition to “tested positive” (since testing availability is still a train wreck). It’s still not perfect but the best I can do without creating a multi-page survey that nobody would complete, but you can always add more descriptive comments after voting.
Webinars
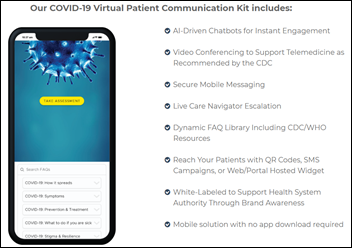
April 15 (Wednesday) 1 ET: “Scaling front-line COVID-19 response: virtual education, screening, triage, and patient navigation.” Sponsor: Orbita. Presenters: Lawrence “Rusty” Hofman, MD, medical director of digital health, Stanford Health Care; Kristi Ebong, MPH, MBA, SVP of corporate strategy, Orbita. The presenters will describe how chatbots can be quickly deployed to streamline individual navigation to the appropriate resources, administer automated virtual health checks for monitoring and managing specific populations, increase access to screening and triage for high-risk populations across multiple channels (web, voice, SMS, and analog phone), and reach individuals in multiple languages.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Hospital operator Quorum Health files Chapter 11 bankruptcy as part of a pre-packaged plan to reduce debt. The company says its 23 hospitals and Quorum Health Resources subsidiary will continue to operate normally.
Companies that inserted mandatory arbitration terms in their business and employment agreements to avoid class-action lawsuits (Epic was the US Supreme Court test case for employers) are subverting the process they created after being overwhelmed with mass arbitration claims. Big companies – which assumed that people wouldn’t bother filing claims — are now refusing to pay the arbitration costs that they themselves specified. One law firm filed 6,000 arbitration claims on behalf of independently contracted delivery drivers for DoorDash, which balked at paying the $9 million in arbitration fees and then rewrote its terms to require using a particular arbitrator whose rates were lower. An unsympathetic federal judge ordered the company to pay the fees, saying, “Your law firm and all the defense law firms have tried for 30 years to keep plaintiffs out of court. And so finally someone says, ‘OK, we’ll take you to arbitration,’ and suddenly it’s not in your interest any more. Now you’re wiggling around, trying to find some way to squirm out of your agreement. There is a lot of poetic justice here.”
People

Clinical AI vendor Jvion hires industry long-timer Jay Deady (Recondo) as CEO.

Chris Aulbach, MS (Cognizant) joins CipherHealth as chief product officer.
Announcements and Implementations
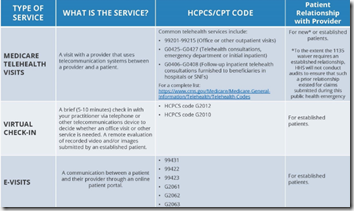
The American Medical Association publishes a 128-page physician guide for implementing virtual visits, which includes a section on evaluating related technologies.
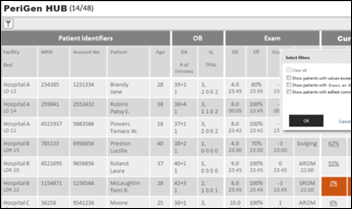
Santa Barbara Cottage Hospital (CA) goes live on PeriGen’s PeriWatch Vigilance automated maternal-fetal early warning system. Part of that system is a centralized acuity management tool that facilitates remote monitoring of laboring patients anywhere, providing flexibility for COVID-19 staffing.
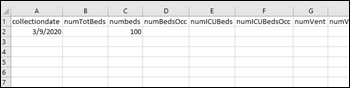
HCA Healthcare and Google Health create the COVID-19 National Response Portal to allow hospitals to share pandemic metrics.
Audacious Inquiry launches the Situation Awareness for Novel Epidemic Response (SANER) Project, which is working on a specification to allow hospitals to send situational awareness reports to public health authorities.
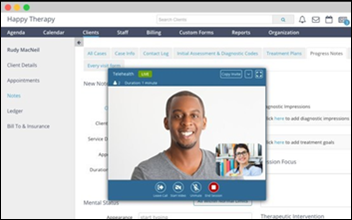
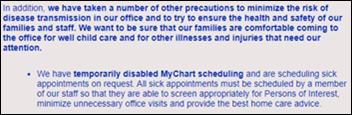
Epic almost never issues press releases, but pushed out this one touting its telehealth capabilities. It calls itself “the nation’s largest electronic health records company,” which it certainly isn’t in terms of company headcount or revenue compared to Cerner, but perhaps is that among companies whose only business is selling EHRs. Novant Health went from 200 video visits per year to 12,000 per week, while NYU Langone Medical Center is conducting 6,500 virtual visits per day, more than 70% of its total. Another Epic update says the company’s EHR now includes two COVID-19 related patient registries to track known or suspected cases.
COVID-19

Former FDA Commissioner Scott Gottlieb, MD tells CNBC that someone needs to take ownership of the surveillance and isolation program to get it in place by August, along with developing 1-2 drugs that can help treat COVID-19 patients with even modest success, to avoid having the economy stall at 80% of pre-coronavirus levels. He expects schools to reopen in the fall, but with added vigilance to detect local outbreaks, and reiterates that development of a vaccine is the ultimate solution at least 18 months down the road.
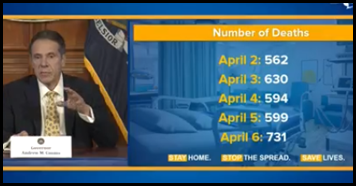
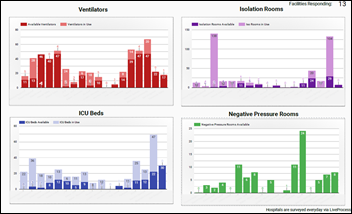
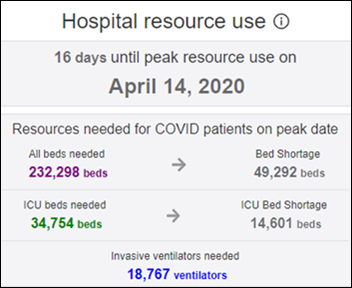
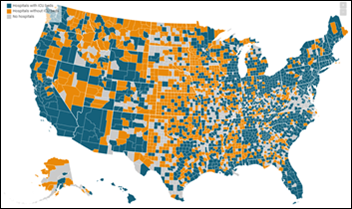
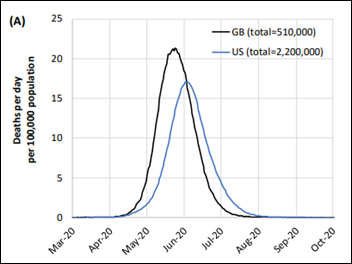
National COVID-19 hospitalization numbers are trending down, as the curve-flattening seems to have worked in reducing demand for ICU beds and ventilators. Deaths are still increasing in New York as a lagging indicator (731 on Monday), but are expected to be lower than initial projections for both New York and the US.
Amazon launches a hospital-only section of its Prime service for selling face shields, masks, thermometers, ventilators, exam gloves, and sanitizer. The company will verify the qualifications of potential buyers and will waive its commissions on purchases.
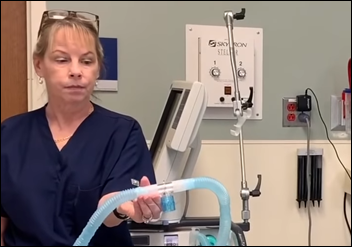
Educational non-profit EDX and Harvard launch an free online course on ventilator use, hoping to help those clinicians who are reassigned to the ICU.
The New York Times explains why official coronavirus death counts are probably far below the actual numbers:
- Coroners don’t have the tests they need to detect coronavirus.
- Early cases in February and early March were likely listed as being due to pneumonia or influenza.
- The system of filling out death certificates and the responsibility for doing so is inconsistent.
- Also inconsistent is the reporting of deaths in which coronavirus is proven or suspected to be present, but not necessarily provable as the single cause of death.
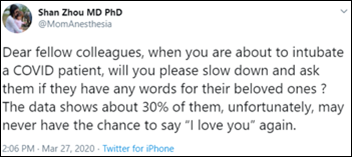
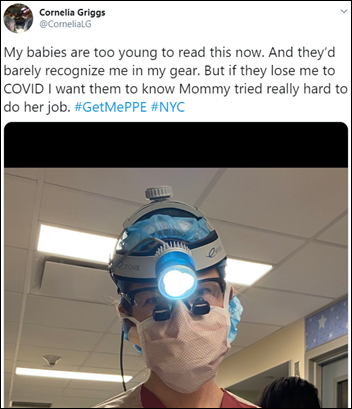
HCA Healthcare-owned West Hills Hospital and Medical Center (CA) suspends a nurse for asking Facebook friends to donate personal protective equipment that her employer wasn’t providing. The hospital says she mentioned in a private chat group that her unit was treating COVID-19 patients only and those statements violated HIPAA and the hospital’s social media policy. She’s in quarantine after being exposed to the virus. An ED nurse at the same hospital said that he was also suspended after mentioning that he was working in a COVID-19 unit. Some healthcare workers are filing whisteblower lawsuits after being fired for issuing social media pleas for PPE.

ICU nurses at Newark Beth Israel Medical Center (NJ) were so desperate for gowns and masks that they raised money on GoFundMe to equip themselves via Ebay purchases. Hospitals executives then suspended Olga Matievskaya, RN, BSN, the nurse who organized the campaign, for distributing unauthorized PPE.
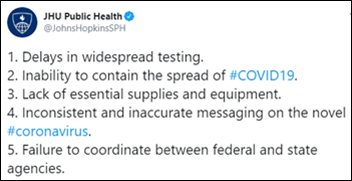
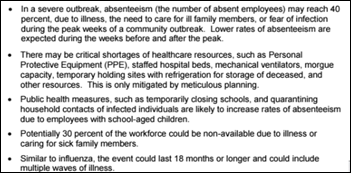
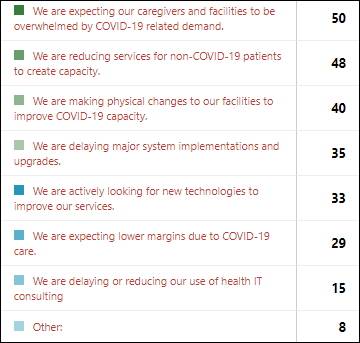
HHS OIG’s survey of 323 hospitals from late March lists their coronavirus-related concerns. President Trump dismissed the report in Monday’s coronavirus briefing, saying “it’s wrong” and scolding the inspector general on Twitter for not talking to “admirals, generals, VP, and others in charge” before publishing the hospital survey results. Hospitals report:
- They are experiencing severe shortages of testing supplies and waiting seven or more days for results, limiting their ability to monitor the health of patients and staff.
- Shortages of PPE are widespread, federal and state help is uncertain, and some vendors are price gouging.
- Hospitals aren’t always able to meet staffing needs due to a people shortage, also worrying that exposure fears and burnout may contribute to short staffing.
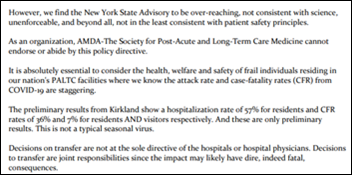
- Post-acute care facilities won’t accept hospital discharges until the patient tests negative for COVID-19, tying up acute care beds.
- Hospitals are running out of IV poles, medical gases, linens, toilet paper, food, thermometers, disinfectants, and cleaning supplies.
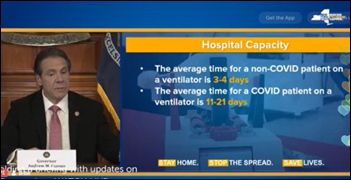
- They are worried about ventilator shortages that may force them to choose which patients get them.
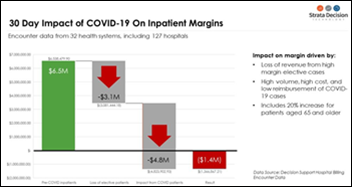
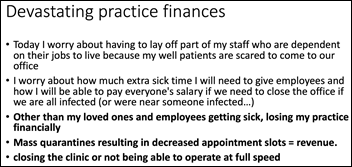
- Costs are increasing as revenues decrease with elimination of elective procedures, quickly depleting cash reserves.
- Guidance from federal, state, and local authorities is ever-changing and inconsistent, and public misinformation is causing patients to show up unnecessarily.
This is well outside my area of expertise, but a New Jersey hospital needs PPE and asked me to forward contact information for anyone who has access to it. Email me and I’ll forward the information.
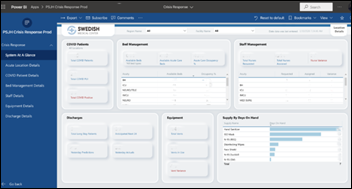
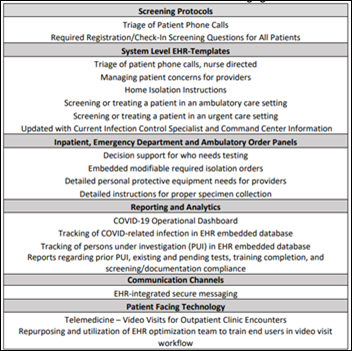
Cerner sent these hospital recommendations for dealing with COVID-19 patient surge, from St. Joseph’s Healthcare System (NJ) VP/CIO Linda Reed, MSN, MBA:
- Review and implement the EHR vendor’s COVID-19 updates and packages.
- Review telehealth documentation and education.
- Prepare to develop lab interfaces for state surveillance.
- Create daily dashboard reporting.
- Review the IT requirements for opening surge beds in non-traditional areas.
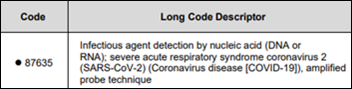
- Implement the new COVID-19 diagnosis and billing codes.
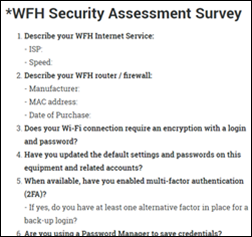
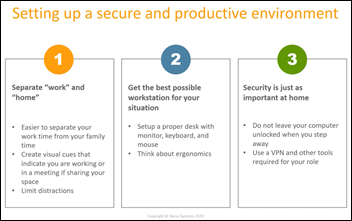
- Prepare to support additional work-from-home technology needs.
- Review government reporting requirements.
- Use remote support tools to support desktops to limit trips to hospital units.
- Prepare for updating EHR access to accommodate clinicians who are reassigned.
- Use remote patient visualization technology to limit room entry.
Other

A Florida business paper covers Orlando Health’s replacement of Allscripts Sunrise with Epic. Orlando’s other big health system AdventHealth, is also implementing Epic, replacing Cerner.
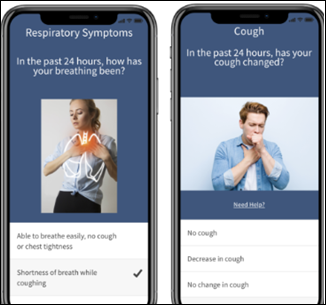
A Baltimore TV station covers the use by Lifebridge Health and Johns Hopkins of technology from Emocha to keep in touch with self-quarantined clinicians. It offers symptom reporting, asynchronous video check-ins to verify thermometer readings, and two-way messaging.
Verizon cancels making onsite Internet connectivity service calls for homes and businesses, with some users reporting they were given a date of November to regain connectivity.

Miss England 2019, Bhasha Mukherjee, MBBS, shelves her overseas humanitarian work and returns to the UK to work at NHS’s Pilgrim Hospital. She explains, “When you are doing all this humanitarian work abroad, you’re still expected to put the crown on, get ready, look pretty. I wanted to come back home. I wanted to come and go straight to work.”
Sponsor Updates

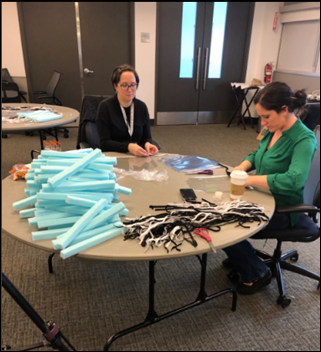
- AGS Health spotlights employee Adelaide Rose’s mask-making efforts for hospitals in New Jersey.
- Medsphere’s ChartLogic division adds integrated telehealth to its ambulatory EHR that allows patients to launch video rooms from its patient portal for a virtual evaluation.
- Baxter Regional (AR) expands its use of EClinicalWorks technology to include virtual visit capabilities.
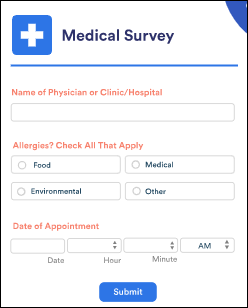
- Access releases COVID-19 Rapid Response EForms, which allows hospitals to offer contactless registration by sending patients an online screening form and then pre-registration documents to complete and sign remotely.
- Diameter Health partners with insurance technology company Clareto to improve underwriting and claims adjudication with data-cleansing technology.
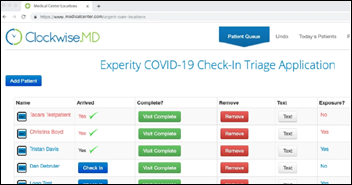
- Experity updates its travel screening questionnaire to help urgent care providers identify new cases of COVID-19.
- Healthwise launches a Coronavirus Resource Center.
- Datica releases a new podcast, “ONC Final Rules on Information Blocking – Part 2.”
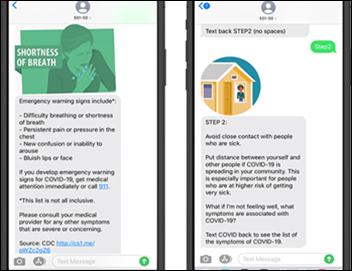
- CareSignal and Americares bring a new COVID-19 text messaging program to the uninsured.
- Clinical Architecture joins the COVID-19 Interoperability Alliance.
Blog Posts
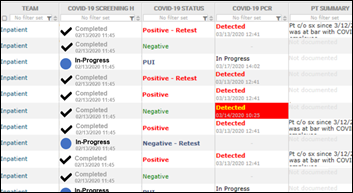
- Leveraging Business Intelligent for COVID-19 Screening (314e)
- How are you coping? We love success stories. (AdvancedMD)
- Keeping Veterans and Responders Connected During a Crisis (Avaya)
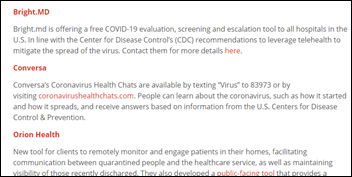
- Social Distancing, Flattening the Curve, & Raising the Bar (Bright.md)
- What is Zoom Bombing? Immediate Steps to Protect Your End Users (Burwood Group)
- The Critical Role of Interoperability During COVID-19 (CarePort)
- Mentoring in the Tech Industry is Rewarding but Requires Time and Soul Searching (CentralLogic)
- How HIE is Playing a Role in Navigating the Coronavirus Outbreak (ChartLogic)
- Expanded Telemedicine Regulations: Documentation Requirements Overview (CereCore)
- NAS Strategies Across the Nation (Collective Medical)
- Expanding How CoverMyMeds Helps Patients Access Their Medications (CoverMyMeds)
- How Analytics can Help Hospitals Better Manage Their ICUs (Dimensional Insight)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


























































































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…