News 10/16/20
Top News
Private equity firm JLL Partners acquires analytics solution vendor MedeAnalytics from Thoma Bravo, which acquired a majority stake in MedeAnalytics in 2015.
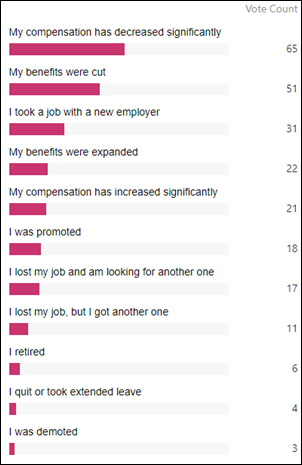
Reader Comments
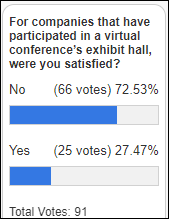
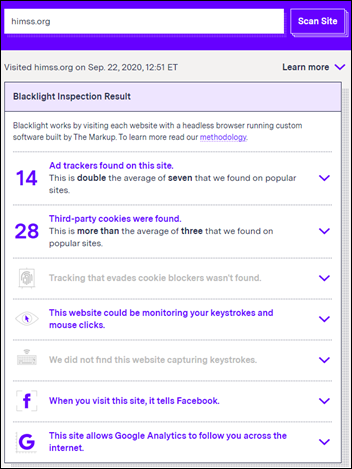
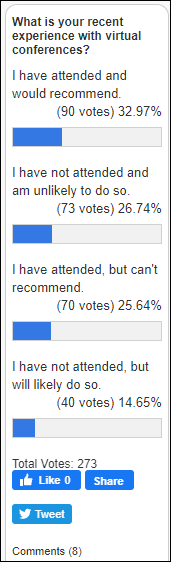
From Chief Complaint: “Re: virtual exhibit halls. Your poll found that companies that paid to participate in a virtual conference’s exhibit hall didn’t find it worth the money or effort. I would be interested to hear from someone who has exhibited and can give their pros and cons, takeaways, what they would do differently, etc.” If you were in charge of a virtual exhibit at HIMSS, HLTH, CHC, etc., how about writing up your experience? I’ll make it anonymous if you’d like. Or if you aren’t motivated to put it in writing, I’ll interview you by phone (again, happily keeping you anonymous if you like). The poll results were interesting as a broad reaction, but it would be fun to get more firsthand insight. I haven’t heard much (any) buzz from Virtual HIMSS, so we’ll see how the even-larger RSNA does in a few weeks, then attendees can for the first time keep eating Thanksgiving leftovers at home instead of bundling up for Chicago.
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor CancerIQ. The Chicago-based company’s precision health platform enables providers to identify, evaluate, and manage entire patient populations based on individual genetic risk factors. By analyzing family history, running predictive risk models, and automating NCCN guidelines, CancerIQ empowers providers with the genetic expertise to prevent cancer, catch it early, and/or create personalized care plans. The platform has been rapidly adopted by some of the top health systems in the country and fully integrates with genetics laboratories, EHRs like Epic and Cerner, and specialty software vendors to streamline workflow, guide clinician decision-making, achieve cost savings, and most importantly, improve patient outcomes. CancerIQ is scaling the use of genetic testing to predict, preempt, and prevent disease. The company offers a toolkit for providers who want to quickly and effectively kick-start a telehealth-powered cancer genetic screening program. Thanks to CancerIQ for supporting HIStalk.
Here’s a video from the American Journal of Managed Care in which CancerIQ co-founder and CEO Feyi Olopade Ayodele, MBA describes how the company is making cancer genetic screening practical.
Listening: new from Sir Chloe, indie rockers from Bennington, Vermont. It’s kind of guitar-forward grungy pop with sweet singing, formed by singer Dana Foote two years ago as her senior-year thesis at Bennington College.
Webinars
October 27 (Tuesday) noon ET. “Don’t Waste This Pandemic (From a Former Healthcare CEO).” Sponsor: Relatient. Presenter: Monica Reed, MD, MSc, former CEO, Celebration Health. Some healthcare organizations are trying to get back to the normalcy of 2019, but tomorrow’s leaders are accelerating even faster in 2020. Two- or three-year roadmaps were accomplished in six months, so what’s next? The presenter will describe how technology was changing before COVID-19, how the pandemic accelerated plans, what we can expect to see as a result, how leaders and providers can adapt, and what healthcare’s digital front door looks like going forward and how it can be leveraged.
October 28 (Wednesday) noon ET: “How to Build a Data-Driven Organization.” Sponsor: Newfire Global Partners. Presenters: Chris Donovan, CEO and founder, Adaptive Product Consulting; Harvard Pan, CTO, Diameter Health; Jason Sroka, chief analytics officer, SmartSense by Digi; Jaya Plmanabhan, data scientist and senior advisor, Newfire Global Partners; Nicole Hale, head of marketing services, Newfire Global Partners. The panel of data experts will discuss the opportunities that data can unlock and the challenges involved with becoming a data-driven organization. Attendees will learn why having a data strategy is important; how to collect, manage, and share data with internal and external audiences; and how to combat internal resistance to create a data-driven culture.
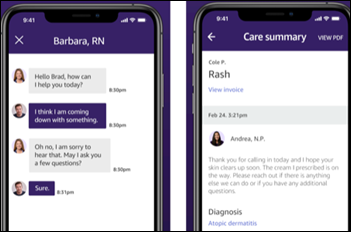
October 29 (Thursday) 1 ET. “How Presbyterian Healthcare Services Is Preparing for a Post-Pandemic Future Using Digital Care Tools.” Sponsor: Bright.md. Presenters: Ries Robinson, MD, SVP/chief innovation officer, Presbyterian Healthcare Services; Ray Costantini, MD, MBA, co-founder and CEO, Bright.md. Presbyterian Healthcare Services changed the way New Mexico patients access healthcare with its pres.today digital front door, which has given patients easy access to care during a global crisis. The health system’s digital care strategy goes beyond simply offering virtual visits and instead makes every episode of care — regardless of where it is delivered — better by streamlining clinical workflows and by directing patients to the most appropriate venue of care. The presenters will describe how Presbyterian has continued to meet patient needs during the pandemic, how it is deploying digital tools to tackle the combined COVID-19 and flu seasons, and how the health system is innovating care delivery to prepare for a post-pandemic future.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Digital check-in vendor Clearwave acquires Odoro, which offers a similar product as well as patient scheduling.

Allscripts shares jumped 30% following news that it will sell CarePort Health to WellSky for $1.35 billion. MDRX shares have increased 2% in the past year versus the Nasdaq’s 46% gain, with the company’s market cap at $1.75 billion, of which CarePort Health and the cash it will generate obviously represent a surprisingly significant portion.
Shared decision-making platform vendor WiserCare raises $3.6 million, increasing its total to $9 million.
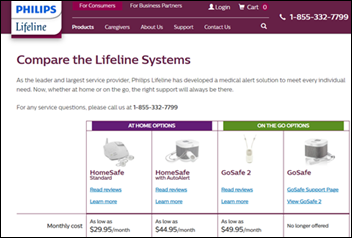
Philips is reportedly seeking a buyer for its Lifeline personal emergency response business. Philips acquired Lifeline for $750 million in January 2006, when Lifeline was generating $150 million in revenue with a 15% operating margin.
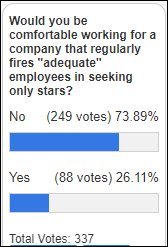
Physician search and appointment scheduling platform vendor Zocdoc says that the lawsuit against the company filed by its former CEO for staging a “fraudulent coup” against him is without merit, it has boosted profit by moving from a flat subscription fee to a per-patient charge to providers, and it responded to COVID by launching video visits in April 2020 and a free video service in May. The company admits that it was in big financial trouble in 2015, adding that it couldn’t replace salespeople fast enough because of company culture problems. It hired a new CEO in November 2015 and says it has reinvented the Zocdoc around core values and a rejection of the “growth at all costs” mindset. The company has raised $226 million through a Series D round (almost none of that after 2015), and with this public mea culpa, seems to be looking for more investment action, maybe via one of those blank check SPACs that are suddenly all the rage.
Sales
- HHS’s Office of Women’s Health contracts with Premier for data and performance improvement methodology to address maternal health. Premier will bring at least 200 hospitals together in a Perinatal Collaborative to implement outcomes-proven best practices and care bundles.
People

Jay Colfer (Geniq) joins Medstreaming as CEO.

Quest Analytics hires Barbara Dumery, MS (Imprivata) as chief product officer.


MDLive promotes Mindy Heintskill, MBA to the newly created position of chief growth officer and hires Kristy Kaiser, MBA as chief product officer.



Healthcare automation technology vendor Olive hires Rohan D’Souza (KenSci) as EVP/GM of cybernetics; Mike Biselli, MA (Catalyst HTI) as VP of emerging technology partnerships; and Tony Brancato as VP of products for cybernetics.

Brian Norris, RN, MBA (OurHealth) joins employee health management company Marathon Health as SVP of population health.

NeoGenomics Laboratories hires David Brooks, MBA (Medlio) as VP of its informatics division, where he rejoins his Medlio co-founder Lori Mehen.
Announcements and Implementations
Epic will use InterSystems IRIS Data Platform, a next-generation system that includes database management, interoperability, and analytics capabilities for data-intensive applications.
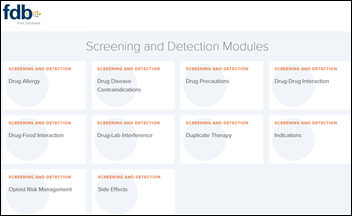
CliniComp will incorporate First Databank’s FDB MedKnowledge database into its EHR, where it will be used in ordering, conflict checking, documenting, and dispensing. It will also implement FDB Interoperability Module for medication reconciliation and interoperability with external systems such as automated dispensing cabinets.
Epic lists 314e’s Speki EHR help solution in its App Orchard.
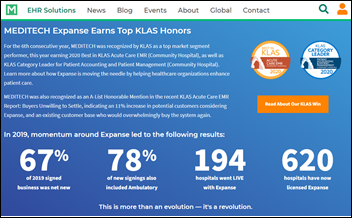
Longtime Meditech user Milford Regional Medical Center (MA) goes live on Expanse.
AMIA announces its 2021 fellows.
CloudWave expands its Meditech hosting to Puerto Rico and the Caribbean in partnership with IT services and telecommunications provider Neptuno.
Government and Politics
The Department of Defense says that private sector connectivity expanded significantly when DoD, the VA, and the Coast Guard connected to CommonWell last week.
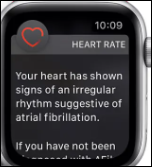
CMS expands the list of telehealth services that Medicare will pay for during the pandemic.
COVID-19
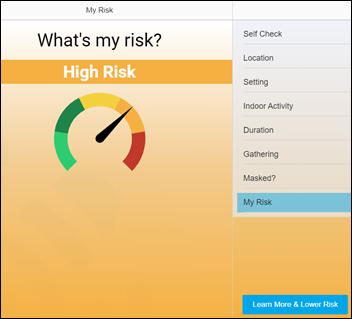
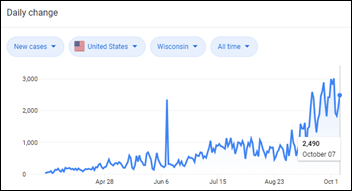
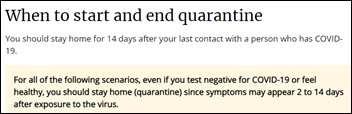
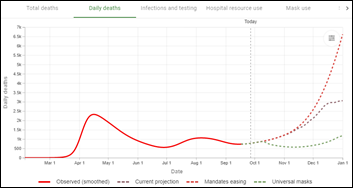
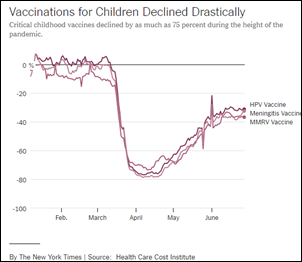
CDC warns that small family gatherings are a growing source of coronavirus spread, reminding everyone that that mitigation is essential, especially with Thanksgiving coming up in which weather forces people indoors and cautious older family members will likely be exposed to younger and less-careful friends and relatives.
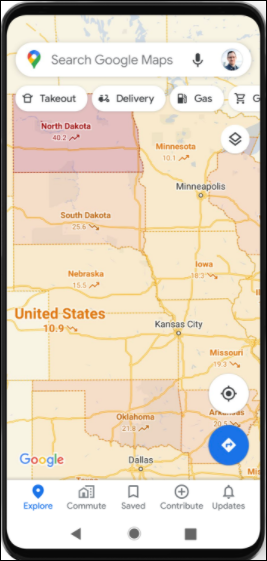
An investigative report published in Science, the journal of the American Association for the Advancement of Science, finds that White House Coronavirus Task Force Coordinator and former CDC employee Deborah Birx, MD drove the decision to abandon the CDC’s hospital data collection system and turn it over to private contactor TeleTracking. One CDC employee immediately quite because of the toxic atmosphere, others said the change was unnecessary because experienced staffers could reliably estimate totals even with missing data, and one texted to a colleague, “Birx has been on a months-long rampage against our data. Good f—ing luck getting the hospitals to clean up their data and update daily.” CDC employees told Science that she is largely responsible for the CDC’s credibility crisis because of her desire to please the White House and her lack of listening ability, noting that she had obtained data from every US hospital while running a CDC HIV/AIDS project and failed to understand why weekly data collection during a global crisis was any different. Birx says 98% of hospitals are reporting, but Science obtained an internal document indicating that only 24% are sending all of the data requested. TeleTracking’s system is also updated 3-4 days behind, struggles to report hospitals the share ID numbers, and consistently reports “nonsensical” numbers, such as 1,500 incidents in which it showed that a hospital had more occupied beds than its total beds.
WHO’s much-awaited Solidarity clinical trial finds that remdesivir does not improve survival rates of COVID-19 patients. The study of 11,266 hospitalized patients found that repurposed drugs such as remdesivir, hydroxychloroquine, lopinavir, and interferon had little effect on mortality or the need to ventilate patients. Remdesivir manufacturer Gilead Sciences says the conclusions of the report, which was made public before its publication, are not consistent with several other studies that showed remdesivir’s clinical benefit. A study published last week shows that use of the drug, which costs $2,340 per five-day course, was associated with a hospital stay reduction from 15 to 10 days with no mortality benefit.
Other


I’m fascinated by the bio of Darren Sommer, DO, MBA, MPH that I ran across. He’s founder and CEO of telemedicine hardware vendor Innovator Health, but his backstory is what caught my eye. He dropped out of college, joined the US Coast Guard at 19, completed EMT training, went back to school to earn an undergraduate degree and then a DO/MPH, then on the day after he finished his residency, joined the US Army’s 82nd Airborne Division, 2nd Brigade Combat Team and spent 15 months serving two tours in Afghanistan, where he also earned a Parachutist Badge and achieved the rank of major. He came home, earned an MBA at Duke and is now an Army Reserve lieutenant colonel along with his CEO job. I like these quotes:
- “The influence of the Airborne’s culture, which is to drop in behind enemy lines and find a way to succeed or expect to die, changes the way you face all challenges in life.I now meet every obstacle in my life with the expectation that failure is not an option.”
- “A hero is someone who does the right thing no matter the consequences. I worked with heroes every day. Some that I worked with received high accolades like the Silver Star or Purple Heart, but most of the heroes I worked with never even received a thank you. These were the soldiers that gave blood when we had a MASCAL [mass casualty], volunteered for patrols so their battle buddy could get rest, or risked their lives to ensure America stayed safe and Afghanistan could be free. This is why when you see a veteran, always thank them for their service. They have been a hero to someone.”
- “I plan to stay in [the Army reserves] another 10 years. I don’t look forward to the day when I can no longer wear the uniform and serve my country.”
- “It was my time in Afghanistan that really shaped my future. I was still a relatively inexperienced physician, and I was taking care of some very sick patients, in some very austere environments. Patients with conditions that I did not get exposed to in my civilian residency. The Army had an excellent communications infrastructure that allowed me to use technology to reach out to other physicians in Afghanistan, the US, and around the world. Their mentorship helped me to make better clinical decisions. It was my first exposure to telemedicine … [upon returning home to practice in a rural hospital] I kept asking myself why telemedicine wasn’t being used here in America like it was being used in Afghanistan.”
- “It took me a long time to realize the difference between failure and success was my effort.”
- “If you hear a horn honk at you while you are driving, it might be your driving, or it just might be them. When you hear a lot of horns honking at you, it is probably you.”
A former British cycling team doctor who has admitted to ordering banned substances claims that a hard drive failure prevents him from providing medical records data to the world governing cycling body. This is the third time he has claimed that a computer problem preventing him from complying with inquiries – he told authorities in 2011 that his laptop had been stolen, then last week said he destroyed his own laptop to prevent “Indian hackers” from accessing its data.
Sponsor Updates
- CentralReach will incorporate Change Healthcare’s RCM software and services into its EHR for autism-focused providers and educators.
- Health Data Movers publishes a new white paper, “Transplant Data Conversion: How We Make It Happen.”
- Healthfinch joins the Health Catalyst family.
- AI Tech Park interviews Saykara founder and CEO Harjinder Sandhu.
- Kyruus publishes the “2020 Patient Access Journey Report.”
- Coffeyville Regional Medical Center (KS) implements Meditech’s depression screening and suicide prevention toolkit.
Blog Posts
- 3 Things to Know About RCM (Experity)
- Introducing Brenda Ashley and Optimum CareerPath (Optimum Healthcare IT)
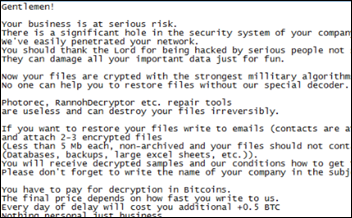
- Evolving the Cybersecurity Landscape (Fortified Health Security)
- You Need More Than a Scripting Engine to Monitor Citrix or VMware Horizon (Goliath Technologies)
- Multidisciplinary Collaboration: Healthcare’s Secret Weapon During Pandemic (Halo Health)
- Four Benefits of Automating Charge Note Reconciliation (Ingenious Med)
- Our Focus at AHIMA20: The Marriage of Prospective and Retrospective Audits (Hayes)
- Embracing Human Centered Design in Healthcare Digital Transformation (The HCI Group)
- Four Strategies Drive High-Value Healthcare Analytics for COVID-19 Recovery (Health Catalyst)
- It’s time to clinically integrate the healthcare supply chain (Infor)
- Four Benefits of Automating Charge Note Reconciliation (Ingenious Med)
- Tales and Tricks of Social Engineering 20 Years Ago and Today (Ingenious Med)
- How to Manage Change in a Dynamic Healthcare Environment (InterSystems)
- The Trends Defining Healthcare’s Next Normal. The Hospital Financial Model They Require (Loyale Healthcare)
- Build Community with Engagement (Medhost)
- Tracking COVID-19 Immunizations Relies on Accurate, Consistent Patient Identification (NextGate)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.







































































































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en