News 4/23/21
Top News
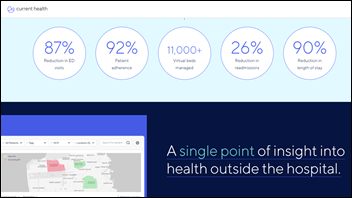
Home monitoring platform vendor Current Health raises $43 million in Series B financing.
The company says its revenue grew 3,000% last year. Its platform is FDA-cleared for performing virtual clinical trials with remote monitoring and video visits.
EHR integration – using HL7, FHIR, or Redox – is available for Epic, Cerner, Allscripts, and Athenahealth.
The CEO completed a master’s in computer engineering and left medical school in Scotland to start the company in 2015 with his co-founder and CTO, who had just completed a PhD in computing science.
The company styles itself as a “mission control” for health systems to transition care to the home. It lists as customers Mayo Clinic, Mount Sinai, Geisinger, Massachusetts General Hospital, Britain’s NHS, and drug companies AztraZeneca and Amgen.
Reader Comments
From Iza Vendor FoSho: “Re: HIMSS. Selling software now as a competitor to its corporate supporters?” HIMSS-owned Healthbox announces Idealy, a system that accepts internal submissions for innovation projects, then allows participants to score them and solicit feedback. HIMSS strays into commercial and potentially competitive territory fairly often, as do many member organizations that collect support dollars from those competitors, but this doesn’t sound like a product that steps on exhibitor toes. The target audience seems to be those big health systems that aspire to play with the big boys in the investment and innovation world, the track record of which is spotty (that’s like asking the DMV to develop photo portraiture software).
From Ivan Issue: “Re: resume. Please review mine.” Suggestions, which I’ll generalize beyond yours specifically having looked at many LinkedIns:
- Don’t refer to yourself in the third person, aka “Mr. Smith,” as though you convinced an all-knowing deity to craft your CV.
- Personalize your “About” section beyond the usual stilted “accomplished, seasoned executive with demonstrated experience …” It’s funny how people think their overview sounds more professional when written as droning, incomplete phrases that are devoid of personality, the admirable brevity of which is often cancelled out by the barrage of tired buzzwords that follows. This is exactly what you wouldn’t do in an interview.
- Don’t list self-assigned, pretentious labels in your LinkedIn description, such as “thought leader,” “visionary,” or “change agent.” It’s mildly effective when others brag vaguely about you, but annoying when you brag vaguely about yourself. I have never seen a self-proclaimed “thought leader” whose thoughts I would allow to lead me.
- Leave out anything under “Education” that isn’t an actual degree from an accredited college or university. Nobody cares where you prepped except your fellow preppies and they already know, while weekend seminars and degrees that were sought but not attained for whatever reason don’t inspire a lot of confidence about determination.
- Include a high-resolution headshot that doesn’t include a cropped-out ex-spouse, wedding formalwear, or a vacation background. Don’t crop or shrink the image since LinkedIn does that while allowing a full-view display by clicking. Use a straight-on view that covers neck to top of head, with no artsy-craftsy poses or filters. Do not under any circumstances fail to include a photo unless you have beliefs about graven images – we all have camera-capable phones, so photo omission suggests issues with self-esteem.
- This is probably just a me thing, but it’s hard when trying to sort out an executive’s career wanderings when the list includes board assignments, volunteer work, trying to get consulting gigs while looking for a job, etc. instead of actual paid jobs working for someone else.
- Be careful about listing a bunch of licenses and certifications that aren’t relevant to the position you hold or want to hold. Health system CEOs who are looking for CIOs don’t care about your CPHIMS or MCSE.
- Spell and capitalize correctly, advice that I’m ashamed to have to offer to executives who surely could have afforded a paid proofreader or commanded an underling who writes well to review their draft.
HIStalk Announcements and Requests
I’m reacting negatively to the overused term “sat down with” in trite reference to interviews, where given limitless quantity (and clearly limited quality) I gag through it several times per day. I say go for the “Madonna with the fake British accent” affectation and call it having a natter, a chin-wag, or a palaver.
Webinars
April 27 (Tuesday) noon ET. “The Modern Healthcare CMIO: Best Practices for Implementing Digital Innovations.” Sponsor: RingCentral, Net Health. Presenters: Nathan Gause, MD, assistant professor of medicine and orthopedic surgeon, University of Missouri Healthcare; Ehab Hanna, MD, MBA, VP/CMIO, Universal Health Services; Subra Sripada, MSIE, partner, Guidehouse; Jigar Patel, MD, VP/chief medical officer, Cerner Government Services. This panel of CMIOs will discuss how their organizations are leveraging digital medicine to improve patient outcomes and provider workflows. Topics will include AI and analytics, effectively implementing AI solutions, establishing data governance and oversight for AI-powered products, care and treatment changes on the horizon, and interoperability of large EHR systems.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Goldman Sachs predicts that even though interest in SPACs has cooled off since the first quarter – when 55 special-purpose acquisition companies were formed, creating a deal-making frenzy that exceeded even the dot-com boom – they could drive $900 billion worth of M&A deals over the next two years. It notes that 394 SPACs are looking for companies to take public, armed with $129 billion of equity capital and a two-year deadline to land a dance partner. It will be interesting to see how many seemingly successful health IT companies are lured into going public by the siren song of a SPAC – with the only surefire money-maker in the transaction being the SPAC’s sponsor – and then wilt under quarter-by-quarter investor pressure, mandatory operational transparency, a divergence of customer demands versus market realities, and the never-ending quest to convince investors that all-important growth will last forever. Not to mention that when the boom inevitably busts, either selectively or broadly, some unicorn-anointed companies that could not have survived IPO scrutiny will be suddenly living a less-rosy life filled with disillusioned investors, squirmy executives surreptitiously eyeing the exit, and curmudgeonly bystanders like me providing a constant reminder that the wisest investors – notably insiders – cashed out their stake at first opportunity before irrational exuberance collided with reality.

London-based Proximie, which offers a live, mixed-reality telesurgery collaboration platform for clinicians performing OR and cath lab procedures, raises $38 million in a Series B funding round.

Medchart, which provides patient-authorized information to attorneys, to patients themselves, and eventually to researchers, raises $17 million in seed and Series A funding. It hopes to expand its information work to researchers.
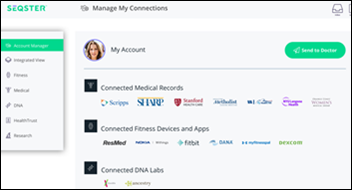
Seqster, which aggregates data from EHRs, wearables, and consumer genomics companies for payers, providers, and researchers, raises a $12 million Series A funding round.
HCA Healthcare announces Q1 results: revenue up 9%, EPS $4.14 versus $1.69, beating Wall Street expectations for both. Shares are up 87% in the past year versus the Dow’s 48% rise, valuing the company at $67 billion. HCA received $9 billion in federal COVID-19 relief funds last year, but returned all of it in October, saying the financial urgency of its 180 hospitals had passed and that returning taxpayer dollars was “appropriate and the socially responsible thing to do.”
Tenet Healthcare announces Q1 results: revenue up 6%, EPS $1.30 versus $1.28, beating expectations for both. Shares are up 172% in the past 12 months, valuing the hospital operator at $6 billion.
Sales
- Cerner chooses life insurance data vendor MIB Group to sell consented access to its 54 million patient medical records, adding to MIB’s list of EHR partners.
People

Analytics vendor Cotiviti hires RaeAnn Grossman, MSP (Wick Healthcare Group) as EVP of risk adjustment and quality.

Chrissy Braden Worth, MBA (Helix) joins Apple in a business development and partnerships role.

Industry long-timer Mitch Morris, MD (OptumInsight) joins EMed as chief operating officer.
Announcements and Implementations
PMD adds medical billing and collection services to its revenue cycle platform offerings.
Regenstrief Institute modifies the open source EHR OpenMRS to meet the needs of Indianapolis first responders who expected to treat more COVID-19 patients in triage center. The team’s work, which took one week, allowed the EMS to register patients and collect their basic clinical information that could be sent to the state’s HIE. The system was never used, however, as the expected demand never materialized.
USPTO awards Medsphere a patent for its Multi-Disciplinary Treatment Plan solution.
PatientKeeper integrates its mobile app with Meditech Expanse, offering users access to patient lists, vital signs, lab and other test results, clinical notes, med list, allergies, and order status.
Tech-aspirational health insurer Oscar launches +Oscar, which is some kind of health plan and member engagement platform that it poorly described. The announcement used the word “stack” eight times, which discouraged me from studying the announcement more than the first few times in my ultimately failed attempt to comprehend it.

CAQH publishes a repository of validated payer FHIR endpoints and third-party apps, allowing payers and developers to find information exchange connections.
Change Healthcare launches InterQual 2021, the latest version of its evidence-based screening tool. It adds four new Medicare criteria modules and new guidance covering COVID-19 treatment, social determinants of health, and the appropriate use of telehealth.
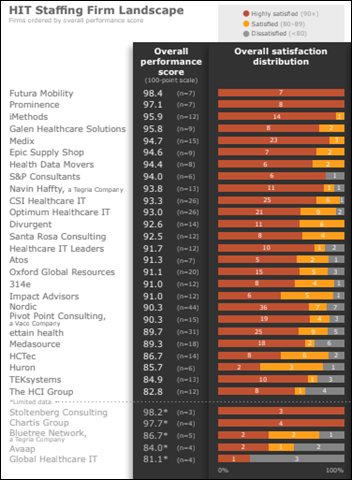
KLAS publishes a report covering health IT staffing firms.
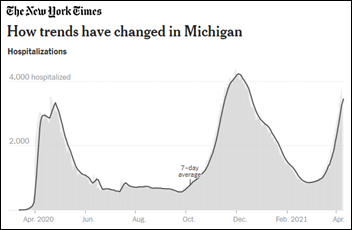
COVID-19
Johnson & Johnson publishes results of its Phase 3 clinical trial of its COVID-19 vaccine, which showed a 67% efficacy 28 days after vaccination, 77% in severe and critical cases, and 64% efficacy against the South Africa variant after 28 days.
Former FDA Commissioner Scott Gottlieb, MD says in a Wall Street Journal opinion piece that the government did the right thing in pausing the use of J&J’s vaccine while reports of rare blood clots are investigated, but FDA rather than CDC should have been put in charge. CDC’s advisory panel adjourned last week without making a decision, while FDA is accustomed to assessing emerging data and advising physicians on benefits and risks.
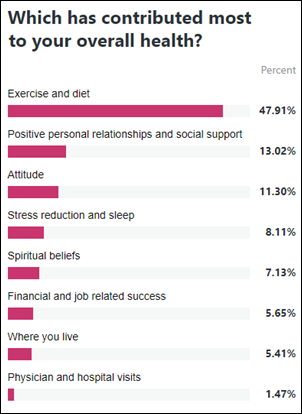
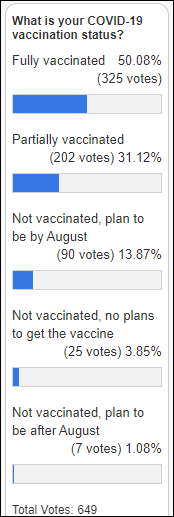
President Biden says the government’s goal of administering 200 million doses of COVID-19 vaccine in 100 days has been met, calling on employers to use available tax credits to get their workers vaccinated. CDC reports that 52% of American adults have received at least their first shot, although numbers are declining for the first time as concerns about vaccine hesitancy begin to outweigh vaccine distribution worries.
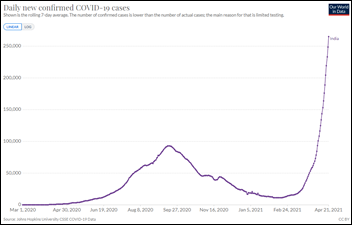
A second wave of infection has pushed India’s cases and deaths to record highs, hospitals are swamped, and oxygen is in short supply. Thursday’s count of new cases in India reached 315,000, the highest ever reported by any country since the pandemic began.
An oxygen tank leak kills at least 22 patients at a public hospital in India that is treating 150 COVID-19 patients. Oxygen is running out everywhere, as the above SOS tweet from Delhi’s health minister makes clear (a tanker arrived at 1:30 a.m. with 30 minutes to spare). The government started building new oxygen plants in October, but none have apparently been finished, with shortages so severe that states are hijacking shipments that are headed elsewhere.
The National Institute of Allergy and Infectious Diseases will launch a study to determine whether the two-dose COVID-19 vaccine cycle works when the products are made by different companies. The study, which hopes to have data available by fall, will also look at whether booster doses are necessary.
Other
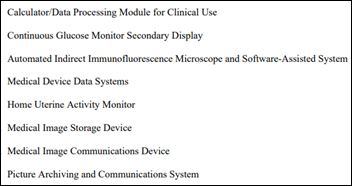
A good observation by AuntMinnie.com – FDA’s announcement this week of the definition of eight classification regulations says it will no longer use the term “PACS.” FDA will now refer to imaging systems as “medical image management and processing system,” which is equally acronym-friendly as “MIMPS.”

I snickered at the breathless announcement of respiratory monitoring vendor Respiratory Motion about its new logo, about which it quoted (falsely, I’m sure) its CEO who supposedly spontaneously ejaculated this in delight: “That is the symbol of action and spirit to construct a positive brand culture with different values: innovation, trust, reliability, discovery, and experiences.” In case that wasn’t eye-rolling enough, we get a pointless animation and an insider’s view, incorrectly punctuated, of how the magnificent logo was developed: “The brand name’s letters RM are exceptionally modified. With the modified crossbar and a higher contrast promoting the depth and upward movement. The balance of two simple ‘RM’ letterforms in the beginning and the end constructed the stability and solidity of the logotype.” I can almost make out the “RM” if I squint, but darned if I can spot innovation, trust, reliability, discovery, and experiences. Marketing is like many things in life – those who are good at it don’t need to convince you.
Sponsor Updates
- Everbridge announces that Steve Forbes, chairman and editor-in-chief of Forbes Media, will keynote its Spring 2021 COVID-19: Road to Recovery virtual leadership summit May 26-27.
- Inc. profiles CarePort Health CEO Lissy Hu and her journey through two acquisitions.
- Forbes names Cerner to its 2021 list of “America’s Best Employers for Diversity.”
- The HIMSS SoCal podcast features Healthcare Triangle VP of Technology Joe Grinstead.
- Impact Advisors is named as one of Modern Healthcare’s Largest IT Consulting Firms for 2021.
Blog Posts
- You’ve Invested Millions for an EHR Your Clinicians Don’t Like. Don’t Replace it – Just Fix it. (Medicomp Systems)
- Supporting the COVID-19 vaccination process with technology and data (Cerner)
- Efficiently Accessing Waveform Data Can Yield Stronger Clinical Research and Outcomes (Capsule)
- What an Emergency Mass Notification System is and Why it Matters (Everbridge)
- 5 Reasons to Conduct Yearly Penetration Testing (Fortified Health Security)
- Vital Change Management is Often Forgotten (Optimum Healthcare IT)
- Glucommander Named 2021 Medical Design Excellence Awards Finalist (Glytec)
- Industry First Citrix Cloud Connector Module (Goliath Technologies)
- The History and Evolution of Conversational AI (Gyant)
- Health Literacy & Care Team Communication: Where We’re Falling Short (Halo Health)
- Predicting Denials to Improve the Healthcare Revenue Cycle and Maximize Operating Margins (Health Catalyst)
- Second Round of Funding for FCC COVID-19 Telehealth Program Announced (Impact Advisors)
- Are Adverse Drug Effects Equal Opportunity Risks? (First Databank)
- Ingenious Med: Supporting a Comprehensive Productivity Optimization Program for a Top US Physician Company (Ingenious Med)
- Part 1 – 2021 Hospital National Patient Safety Goals Series: Identifying Patient Safety Risks (Medhost)
- A Conversation with Carl Smith, CIO, King’s Daughters Medical Center (Meditech)
- 7 Signs It’s Time to Update Your PT Billing System (MWTherapy)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.





































































































Wayne Gillis' LinkedIn post. Neither Rehoboth McKinley or Great Falls Clinic is on Epic. Did he miss a workplace on…