News 6/5/20
Top News
Governments around the world have changed their COVID-19 policies using apparently flawed research findings from virtually unknown US analytics vendor Surgisphere, whose handful of employees includes a science fiction writer and an adult entertainer.

Lancet has retracted the paper and NEJM has begun the retraction process for hydroxychloroquine-related articles that were based on suspicious data from the company, which is led by founder, CEO, and former vascular surgeon Sapan Desai, MD, PhD.
Surgisphere, which does not identify any scientific advisory board that oversees its work, recently pivoted from publishing medical textbooks. It claims to have created a real-time database of 240 million anonymized patient encounters from 1,200 healthcare organizations in 45 countries, It says the information is provided by “our hospital customers,” although the company declines to name them and no hospitals have come forward as being among those data-providing customers.
Desai says the company has 11 employees. He says it uses AI/ML to perform the data analysis, further explaining, “The labor intensive task required for exporting the data from an electronic health records, converting it into the format required by our data dictionary, and fully de-identifying the data is done by the healthcare partner.”
I found a 2015 paper with Desai as the lead author that used Cerner Health Facts as its data source, so I’m wondering if that’s what Surgisphere uses. I’ve asked Cerner to confirm and am waiting to hear back. I have confirmed that the source is not Epic Cosmos.
As an HIStalk reader says, “This is a major setback for science and the credibility of medical expertise.” I would add that it may also call into question how researchers use aggregated EHR data to draw clinical conclusions when they may not fully understand the semantics and sourcing of that data, especially when most of us know how messy and maddeningly inconsistent EHR data can be even within a single health system, with the potential of AI/ML to introduce further errors while trying to clean it up.
Webinars
June 10 (Wednesday) 1 ET. “COVID-19: preparing your OR for elective surgeries.” Sponsor: Intelligent Medical Objects. Presenters: Janice Kelly, MS, RN, president, AORN Syntegrity Inc.; David Bocanegra, RN, nurse informaticist, IMO. The presenters will cover the steps and guidelines that are needed for hospitals to resume performing elective surgeries and how healthcare information technology can optimize efficiencies and financial outcomes for the return of the OR.
June 18 (Thursday) 12:30 ET. “Understanding the ONC’s Final Rule: Using FHIR HL7 for Successful EHR Integrations.” Sponsor: Newfire Global Partners. Presenters: Bob Salitsky, healthcare IT expert, Newfire Global Partners; Jaya Plmanabhan, MS, healthcare data scientist. This fast-paced, 30-minute webinar will provide an overview of the Final Rule and describe how technology vendors, payers, and providers can use FHIR HL7 to deliver true interoperability. Attendees will learn how to define the data, technology, and flows needed for their EHR integration projects; how products can retrieve health information while meeting compliance regulations; and the benefit of adopting quickly to the future of data exchange while simplifying future integration efforts.
Acquisitions, Funding, Business, and Stock
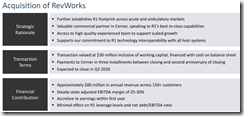
RCM company R1’s shares jumped over 9% on the news that it will acquire Cerner’s RevWorks business in a transaction valued at $30 million. As part of the deal, Cerner will offer R1’s software and services to customers and prospects. In an April 2019 earnings call, company reps said RevWorks had grown stagnant, contributing $200 million in annual revenue. Cerner had been using its RevWorks offerings “to more tightly align the client to Cerner” for additional sales of its software and services.
Sales
- Cumberland River Hospital (TN) selects RCM software and services from TruBridge, and EHR technology from CPSI sister company Evident.
- CHI Texas Health Network selects Innovaccer’s FHIR Data Activation Platform to help it better manage utilization, care workflows, and patient outreach.
People

Moffitt Cancer Center promotes interim CIO Elizabeth Lindsay-Wood, MBA to the permanent VP/CIO position.

MDLive names Cynthia Zelis, MD (University Hospitals) as chief medical officer.


Intermountain Healthcare hires Ryan Smith, MBA (Health Catalyst) as VP/CIO. He replaces Marc Probst, MBA, who will retire.

AI-powered physician assistant developer Saykara hires Joy Efron (Glytec) as VP of marketing.
Announcements and Implementations
Change Healthcare announces GA of Connected Consumer Health, which includes provider search, appointment scheduling, patient intake, messaging, and billing.
Healthfully adds NextGate’s enterprise master patient index to its white-labeled personal health and wellness record.

Banner Health will use video technology to conduct rounding on patients with COVID-19, repurposing patient room TVs with videoconferencing via virtual care technology from VeeMed and Intel.

Beauregard Health System (LA) implements SOC’s Telemed IQ software for critical care, inpatient neurology, emergency neurology, psychiatry, and cardiology.
Government and Politics
Congressional sources say the VA probably won’t restart its Cerner rollout until the fall because of COVID-19 demands.

A GAO review finds that the “Mar-a-Lago group” of three influential associates of President Trump meddled in the VA’s decision-making as private citizens, including influencing its selection of Cerner, but GAO says it was outside the scope of its investigation to determine whether the group constituted a formal advisory committee whose membership and role carry legal ramifications. Mostly it seems the three — none of whom have any government or military experience — wasted the VA’s time in demanding to become involved, pitching themselves and their associates for various projects, and asking newbie questions using the mandate from the president that left VA officials uncertain about how much effort to spend dealing with them.
HHS provides health systems an additional $250 million to help them expand virtual care and telemedicine services, train staff, procure PPE, and coordinate COVID-19 responses.
COVID-19
HHS issues new COVID-19 testing data requirements that it hopes will give it better understanding of the outbreak. Laboratories must report de-identified COVID-19 testing results to the CDC in one of three ways: (a) through local health departments via HL7 or CSV; (b) by a centralized platform such as AIMS whose information is then routed to CDC; or (c) via an HIE. Required data elements include patient demographics (age, race, ethnicity, sex, ZIP code, and county of residence); provider name and NPI; and date ordered and collected. The same information must be provided for home-based tests. HHS asks (but does not require) that the patient’s name, address, phone number, and date of birth be collected and reported. Also recommended but not mandatory is that the lab results include the test result, unique patient identifier, LOINC-coded test ordered, device identifier, and accession number. HHS wants to start receiving the new data elements as soon as possible, but no later than August 1.
Morgan Stanley’s COVID-19 model shows a slowly expanding epidemic in the US, with cases and/or hospitalizations rising in Arkansas, Arizona, North Carolina, Washington, Utah, and Texas, leading to its concerns that the US will experience an earlier second wave than other Western nations and will carry a big infection burden into fall as reintroducing mitigation strategies afterward may not be feasible.
Sweden’s top epidemiologist admits that the country’s controversial strategy of avoiding lockdowns to allow mounting a sustained COVID019 response has not been successful, as its 43 deaths per 100,000 population ranks among the worst globally and the country’s economy is slumping anyway.
Premier asks HHS to make 24 temporary, COVID-related regulatory waivers permanent, primarily those involving telehealth. They include allowing non-rural providers to provide services, expanding the types of practitioners, allowing audio-only visits, and expanding telehealth to occupational and behavioral health services. Premier also recommends changing EMTALA to allow pre-admission screening, allowing nurse practitioners and physician assistants to perform routine medical tasks, and eliminating the rule that requires Medicare patients to undergo a three-day inpatient hospital stay before they can be admitted to a skilled nursing facility.

Fitbit secures Emergency Use Authorization from the FDA for its new Fitbit Flow ventilator. The wearables company developed the device with help from the Mass General Brigham Center for COVID Innovation and emergency physicians at Oregon Health & Science University.
A study published in the New England Journal of Medicine finds that hydroxychloroquine did not prevent people who had been exposed to COVID-19 from developing the disease.
Other
A Cleveland Clinic analysis of EHR data finds that while behavioral health ED visits dropped by 28% with the implementation of stay-at-home orders, suicide-related encounters decreased by 60%. The authors don’t know whether the drop-off was due to people not seeking mental health care, using behavioral telehealth services as an alternative, or experiencing fewer suicidal thoughts while isolated. The authors will correlate these findings with actual suicide rates once those are published.
Sponsor Updates
- Wolters Kluwer Health’s customer support teams for UpToDate, Ovid, and Lippincott each win a NorthFace ScoreBoard Award from the Customer Relationship Management Institute.
- Microsoft awards Billings Clinic (MT) and Health Catalyst a joint 2020 Health Innovation Award.
- Health Data Movers publishes a new case study, “COVID-19 Rapid Response.”
- Dina will sponsor the June 18 virtual demo day of Home Health Care News, where it will showcase its COVID-19 employee health screening and reporting tools.
- Hyland donates $10,000 to The Foundation of FirstHealth’s COVID-19 Response Fund.
- KLAS recognizes Impact Advisors with top marks in its Clinical Optimization Services 2020 report.
- Nordic releases a new edition of its HIT Breakdown podcast, “Automating submission of data to registries.”
- CentralLogic publishes a new case study, “Arizona Surge Line: A unique collaborative response to the COVID-19 pandemic and beyond.”
- Bright.md announces that its Smart Exam virtual care technology is now available in Epic’s App Orchard.
- Health Data Movers announces new account managers.
- Health Catalyst will participate virtually in the William Blair Annual Growth Stock Conference on June 10 and the Goldman Sachs Annual Global Healthcare Conference on June 11.
Blog Posts
- How Connected Medical Devices Can Slow COVID-19 Spread in Hospitals (Capsule)
- Coping with COVID-19 – Part 2 (Ingenious Med)
- Single Sign-On vs. MFA: Do You Know the Difference? (Fortified Health Security)
- Maimonides Medical Center Quickly Troubleshoots “Citrix is Slow” Complaints (Goliath Technologies)
- How Google Cloud partners are supporting customers during COVID-19 (Google Cloud)
- Drive-Through COVID-19 Testing Best Practices (Halo Health)
- Virtual Care in Population Health (The HCI Group)
- HITComm – A COVID-19 HIT Solutions Forum (HCTec)
- The Able Health Quality Measures Solution: Why a Comprehensive Approach Matters (Health Catalyst)
- Implementing Prescription Renewal Technology During a Pandemic (Healthfinch)
- Did You Know That the Imat Platform Brings More Meaning to Data Through Natural Language Processing? (Imat Solutions)
- Planning Your Comeback (Impact Advisors)
- Patient-centric and Cost-effective staffing tools designed for Healthcare (Infor)
- The impact of canceling elective procedures due to COVID-19 (Intelligent Medical Objects)
- To Recover After COVID-19, Healthcare Providers Must Advance Tools for Patient Self-Help (Loyale Healthcare)
- How EHRs Help Nurses Balance Care Planning (Medhost)
- What it means to survive cancer, 10 years later (Meditech)
- 7 Biggest Issues Facing Physical Therapists in 2020 (And Tips on Tackling Them) (MWTherapy)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…